
- •Preface
- •Contents
- •Pattern Approach for Lung Imaging
- •1: Nodule
- •Solitary Pulmonary Nodule (SPN), Solid
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Lung Cancer (Solid Adenocarcinoma)
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Carcinoid or Atypical Carcinoid
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •BALT Lymphoma
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Tuberculoma
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Hamartoma
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Sclerosing Hemangioma
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Ground-Glass Opacity Nodule
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Atypical Adenomatous Hyperplasia (AAH)
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Adenocarcinoma in Situ (AIS)
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Minimally Invasive Adenocarcinoma (MIA)
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •2: Mass
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Pulmonary Sarcoma
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Progressive Massive Fibrosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pulmonary Actinomycosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •3: Consolidation
- •Lobar Consolidation
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Lobar Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Invasive Mucinous Adenocarcinoma
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pulmonary Infarction
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Patchy and Nodular Consolidation
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Airway-Invasive Pulmonary Aspergillosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pulmonary Cryptococcosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •IgG4-Related Lung Disease
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Lymphomatoid Granulomatosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •4: Beaded Septum Sign
- •Diseases Causing the Sign
- •Distribution
- •Clinical Considerations
- •References
- •5: Comet Tail Sign
- •Diseases Causing the Sign
- •Distribution
- •Clinical Considerations
- •Rounded Atelectasis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •6: CT Halo Sign
- •Diseases Causing the Sign
- •Distribution
- •Clinical Considerations
- •Angioinvasive Pulmonary Aspergillosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Metastatic Hemorrhagic Tumors
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pulmonary Endometriosis with Catamenial Hemorrhage
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •7: Galaxy Sign
- •Diseases Causing the Sign
- •Distribution
- •Clinical Considerations
- •Galaxy Sign in Pulmonary Tuberculosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •8: Reversed Halo Sign
- •Diseases Causing the Sign
- •Distribution
- •Clinical Considerations
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pulmonary Mucormycosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Lymphomatoid Granulomatosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •9: Tree-in-Bud Sign
- •Diseases Causing the Sign
- •Distribution
- •Clinical Considerations
- •Aspiration Bronchiolitis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Foreign-Body-Induced Pulmonary Vasculitis (Cellulose and Talc Granulomatosis)
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •Diseases Causing the Sign
- •Distribution
- •Clinical Considerations
- •Bronchial Atresia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Bronchial Tuberculosis and Mucoid Impaction
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Foreign-Body Aspiration
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Allergic Bronchopulmonary Aspergillosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •11: Lobar Atelectasis Sign
- •Disease Causing the Sign
- •Distribution
- •Clinical Considerations
- •Right Upper Lobar Atelectasis
- •Left Upper Lobar Atelectasis
- •Right Middle Lobar Atelectasis
- •Lower Lobar Atelectasis
- •References
- •Cavity
- •Diseases Causing the Cavity
- •Distribution
- •Clinical Considerations
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Langerhans Cell Histiocytosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Septic Pulmonary Embolism
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Cavitary Pulmonary Tuberculosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Paragonimiasis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Cyst
- •Diseases Causing the Cyst
- •Distribution
- •Clinical Considerations
- •Blebs and Bullae
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Pulmonary Sequestration
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Intrapulmonary Bronchogenic Cyst
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Traumatic Lung Cysts
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •References
- •Mosaic Attenuation
- •Diseases Causing the Mosaic Attenuation Pattern
- •Distribution
- •Clinical Considerations
- •Cystic Fibrosis
- •Pathology and Pathogenesis
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Constrictive Bronchiolitis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Chronic Pulmonary Thromboembolism
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Idiopathic Pulmonary Arterial Hypertension
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Airway Disease (Bronchiectasis and Bronchiolectasis)
- •Distribution
- •Clinical Considerations
- •Swyer-James-MacLeod Syndrome
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Dyskinetic Cilia Syndrome
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •14: Air-Crescent Sign
- •Diseases Causing the Sign
- •Distribution
- •Clinical Considerations
- •Aspergilloma
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Rasmussen’s Aneurysm
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •15: Signet Ring Sign
- •Diseases Causing the Sign
- •Distribution
- •Clinical Considerations
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •16: Interlobular Septal Thickening
- •Smooth Septal Thickening
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Pulmonary Edema
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Niemann–Pick Disease
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Nodular Septal Thickening
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Pulmonary Lymphangitic Carcinomatosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •References
- •17: Honeycombing
- •Honeycombing with Subpleural or Basal Predominance
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Asbestosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Honeycombing with Upper Lung Zone Predominance
- •Diseases Causing the Pattern and Distribution
- •Distribution
- •Clinical Considerations
- •Idiopathic Familial Pulmonary Fibrosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Chronic Hypersensitivity Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •End-stage Fibrotic Pulmonary Sarcoidosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •18: Small Nodules
- •Small Nodules with Centrilobular Distribution
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Mycoplasma Pneumoniae Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Diffuse Panbronchiolitis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Follicular Bronchiolitis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pulmonary Tumor Embolism
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Pneumoconiosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pulmonary Sarcoidosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pulmonary Alveoloseptal Amyloidosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Small Nodules with Random (Miliary) Distribution
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Miliary Tuberculosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Miliary Metastasis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •19: Multiple Nodular or Mass(-like) Pattern
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Pulmonary Metastasis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pulmonary Lymphoma
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Amyloidomas
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •ANCA-Associated Granulomatous Vasculitis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •Ground-Glass Opacity with Reticulation and Fibrosis
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Ground-Glass Opacity with Reticulation, but without Fibrosis (Crazy-Paving Appearance)
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Pneumocystis jirovecii Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Lipoid Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pulmonary Alveolar Proteinosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Mucinous Adenocarcinoma or Adenocarcinoma in Situ, Diffuse Form
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Desquamative Interstitial Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Ground-Glass Opacity without Reticulation, with Small Nodules
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Subacute Hypersensitivity Pneumonitis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Cytomegalovirus Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Diffuse Alveolar Hemorrhage
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Ground-Glass Opacity without Reticulation, Diffuse Distribution
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Acute Hypersensitivity Pneumonitis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Acute Eosinophilic Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •22: Consolidation
- •Consolidation with Subpleural or Patchy Distribution
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Cryptogenic Organizing Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Chronic Eosinophilic Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Churg–Strauss Syndrome
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Radiation Pneumonitis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Consolidation with Diffuse Distribution
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Viral Pneumonias
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Acute Interstitial Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Diffuse Alveolar Hemorrhage
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •23: Decreased Opacity with Cystic Walls
- •Cavities
- •Diseases Causing Cavities
- •Distribution
- •Clinical Considerations
- •Rheumatoid Lung Nodules
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Cavitary Metastasis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Cysts
- •Diseases Causing Multiple Cysts
- •Distribution
- •Clinical Considerations
- •Lymphangioleiomyomatosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Lymphocytic Interstitial Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Emphysema
- •Distribution
- •Clinical Considerations
- •Centrilobular Emphysema
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •Patient Prognosis
- •Paraseptal Emphysema
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •Patient Prognosis
- •References
- •24: Decreased Opacity without Cystic Walls
- •Mosaic Attenuation, Vascular
- •Distribution
- •Clinical Considerations
- •Airway Diseases Causing Mosaic Attenuation
- •Distribution
- •Clinical Considerations
- •Asthma
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •Distribution
- •Clinical Considerations
- •Cystic Fibrosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •26: Pneumonia
- •Lobar Pneumonia
- •Bronchopneumonia
- •Interstitial Pneumonia
- •27: Drug-Induced Lung Disease
- •Interstitial Pneumonitis and Fibrosis
- •Eosinophilic Pneumonia
- •Cryptogenic Organizing Pneumonia
- •Diffuse Alveolar Damage
- •Hypersensitivity Pneumonia
- •References
- •Systemic Lupus Erythematosus (SLE)
- •Rheumatoid Arthritis (RA)
- •Progressive Systemic Sclerosis (PSS)
- •Sjögren’s Syndrome
- •Mixed Connective Tissue Disease
- •Ankylosing Spondylitis
- •References

Airway Disease (Bronchiectasis and Bronchiolectasis) |
125 |
|
|
more or less concentric fashion in the vessel lumen. Occasionally, the intimal Þbrosis is eccentric in location or traverses the lumen. The plexogenic arteriopathy is thought to be related to the vascular pruning (central arterial enlargement, peripheral vascular obliteration, and mosaic perfusion).
Patient Prognosis
With advances in knowledge of the disease and the availability of newer therapeutic agents, such as endothelin receptor antagonists, phosphodiesterase inhibitors, and prostanoids, survival of patients with idiopathic pulmonary arterial hypertension has improved but still remains suboptimal. The French Registry demonstrated that 1-, 2-, and 3-year survivals of pulmonary arterial hypertension are 85.7, 69.5, and 54.9 % for incident cases, respectively [31].
Airway Disease (Bronchiectasis
and Bronchiolectasis)
Definition
syndrome, HIV infection) infection (Fig. 13.6). Bronchiectasis may occur in association with a variety of genetic abnormalities, especially those with abnormal mucociliary clearance, immune deÞciency, or structural abnormalities of the bronchus or bronchial wall (cystic Þbrosis, alpha-1-antitrypsin deÞciency, dyskinetic cilia syndrome (Fig. 13.7), WilliamsÐCampbell syndrome, MounierÐKuhn syndrome, immunodeÞciency syndromes). Noninfectious causes of bronchiectasis include allergic bronchopulmonary aspergillosis (ABPA); asthma, bronchial obstruction by tumor, foreign body, or congenital abnormalities; and systemic diseases (collagen vascular disease and inßammatory bowel disease). Bronchiectasis may also occur in patients with constrictive bronchiolitis including chronic graft-ver- sus-host disease (Table 13.2). Bronchiolectasis is usually associated with bronchiolitis (please refer to section ÒSmall Nodules with Centrilobular DistributionÓ in Chap. 18). In patients with lung Þbrosis (usual interstitial pneumonia, nonspeciÞc interstitial pneumonia) and distortion of lung architecture (pulmonary tuberculosis), traction bronchiectasis and bronchiolectasis are commonly present.
Distribution
Bronchiectasis is irreversible localized or diffuse bronchial dilatation, usually resulting from chronic infection, proximal airway obstruction, or congenital bronchial abnormality [1, 32] (Fig. 13.5). Morphologic criteria on thin-section CT scans include bronchial dilatation with respect to the accompanying pulmonary artery (signet ring sign), lack of tapering of bronchi, and identiÞcation of bronchi within 1 cm of the pleural surface [33] (Fig. 13.5). Bronchiectasis may be classiÞed as cylindric, varicose, or cystic, depending on the appearance of the affected bronchi. It is often accompanied by bronchial wall thickening, mucoid impaction (please note Chap. 10), and small airway abnormalities [33].
Bronchiolectasis is deÞned as dilatation of bronchioles. When dilated bronchioles are Þlled with exudates and are thick walled, they are visible as a tree-in-bud pattern or as centrilobular nodules on CT [34].
Traction bronchiectasis and bronchiolectasis, respectively, represent irregular bronchial and bronchiolar dilatation caused by surrounding retractile pulmonary Þbrosis [35].
Diseases Causing the Bronchiectasis and
Bronchiolectasis
Bronchiectasis can result from chronic or severe bacterial infection (Staphylococcus, Klebsiella, Mycobacterium tuberculosis, nontuberculous mycobacterial disease), fungal (histoplasmosis) infection, and viral (Swyer-James-MacLeod
Bronchiectasis as sequelae of pulmonary tuberculosis typically involves upper lobes [36]. In nodular bronchiectatic form of nontuberculous mycobacterial disease, bronchiectasis usually involves the right middle lobe, lingular division of the left upper lobe, and both lower lobes. In cystic Þbrosis, proximal or perihilar bronchia are always involved when bronchiectasis is present. All lobes are typically involved, although early in the disease, abnormalities show often predominantly upper lobe predominance in their distribution [3]. Although central or diffuse bilateral bronchiectasis is common in patients with dyskinetic cilia syndrome, bronchiectasis involves predominantly or exclusively the lower lobes [37]. In WilliamsÐCampbell syndrome, varicose and cystic bronchiectases are limited to the fourth-, Þfth-, and sixth-generation bronchi [38]. ABPA typically involves segmental and subsegmental bronchi of the upper lobes.
Clinical Considerations
Cystic Þbrosis results from an autosomal-recessive genetic defect in the structure of the cystic Þbrosis transmembrane regulator protein, which leads to abnormal chloride transport across epithelial membranes [7]. The major clinical manifestations of cystic Þbrosis are obstructive pulmonary disease and pancreatic insufÞciency. Dyskinetic cilia syndrome is a group of autosomal-recessive disorders associated with defective ciliary structure and function and
126 |
13 Decreased Opacity without Cystic Airspace |
|
|
a |
b |
c |
d |
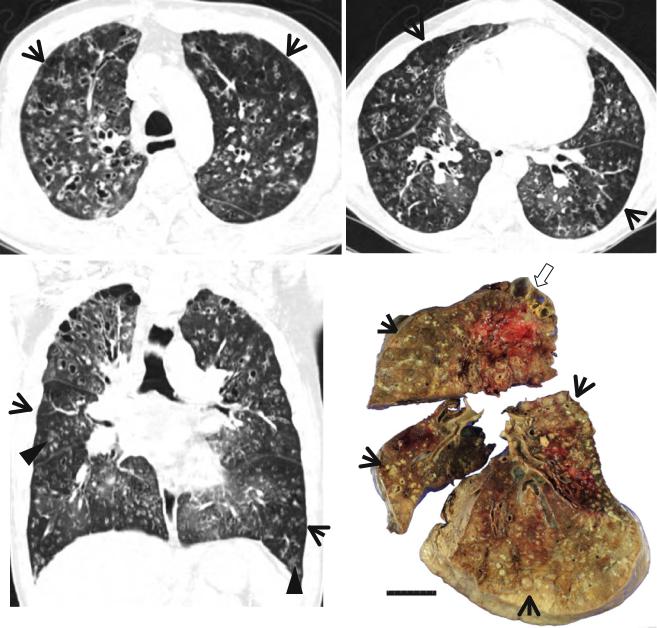
Fig. 13.5 Extensive bronchiectasis in both lungs in a 44-year-old man in whom speciÞc causes for bronchiectasis could not be elucidated. Patient received bilateral lung transplantation. (a, b) Lung window images of CT scans (2.5-mm section thickness) obtained at levels of aortic arch (a) and basal segmental bronchi (b), respectively, show extensive bronchiectasis in both lungs. Also note patchy areas (arrows) of mosaic attenuation. (c) Coronal reformatted CT image (2.0-mm sec-
tion thickness) demonstrates extensive bronchiectasis and cellular bronchiolitis of tree-in-bud signs (arrowheads) in both lungs. Also note patchy areas (arrows) of mosaic attenuation. (d) Gross pathologic specimen of explanted right lung discloses bronchiectatic and bronchiolectatic airways Þlled with abscess (numerous yellow necrotic nodules, arrows) down to membranous bronchiolar level. Also note bullae (open arrow) in right upper lobe
predispose to sinusitis, recurrent pulmonary infections, and bronchiectasis [39]. Situs inversus totalis or heterotaxy is seen in approximately 50 % of patients. WilliamsÐCampbell syndrome is a congenital form of bronchiectasis usually identiÞed in infancy. It shows familial clustering and may be associated with other congenital abnormalities [40].
ABPA results from both type I and type III hypersensitivity reactions to the endobronchial growth of Aspergillus species and is characteristically associated with eosinophilia, symptoms of asthma, and typical imaging Þndings [8]. It is seen almost exclusively in patients with asthma or cystic Þbrosis.
