
- •Preface
- •Contents
- •Pattern Approach for Lung Imaging
- •1: Nodule
- •Solitary Pulmonary Nodule (SPN), Solid
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Lung Cancer (Solid Adenocarcinoma)
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Carcinoid or Atypical Carcinoid
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •BALT Lymphoma
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Tuberculoma
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Hamartoma
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Sclerosing Hemangioma
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Ground-Glass Opacity Nodule
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Atypical Adenomatous Hyperplasia (AAH)
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Adenocarcinoma in Situ (AIS)
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Minimally Invasive Adenocarcinoma (MIA)
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •2: Mass
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Pulmonary Sarcoma
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Progressive Massive Fibrosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pulmonary Actinomycosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •3: Consolidation
- •Lobar Consolidation
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Lobar Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Invasive Mucinous Adenocarcinoma
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pulmonary Infarction
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Patchy and Nodular Consolidation
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Airway-Invasive Pulmonary Aspergillosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pulmonary Cryptococcosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •IgG4-Related Lung Disease
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Lymphomatoid Granulomatosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •4: Beaded Septum Sign
- •Diseases Causing the Sign
- •Distribution
- •Clinical Considerations
- •References
- •5: Comet Tail Sign
- •Diseases Causing the Sign
- •Distribution
- •Clinical Considerations
- •Rounded Atelectasis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •6: CT Halo Sign
- •Diseases Causing the Sign
- •Distribution
- •Clinical Considerations
- •Angioinvasive Pulmonary Aspergillosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Metastatic Hemorrhagic Tumors
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pulmonary Endometriosis with Catamenial Hemorrhage
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •7: Galaxy Sign
- •Diseases Causing the Sign
- •Distribution
- •Clinical Considerations
- •Galaxy Sign in Pulmonary Tuberculosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •8: Reversed Halo Sign
- •Diseases Causing the Sign
- •Distribution
- •Clinical Considerations
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pulmonary Mucormycosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Lymphomatoid Granulomatosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •9: Tree-in-Bud Sign
- •Diseases Causing the Sign
- •Distribution
- •Clinical Considerations
- •Aspiration Bronchiolitis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Foreign-Body-Induced Pulmonary Vasculitis (Cellulose and Talc Granulomatosis)
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •Diseases Causing the Sign
- •Distribution
- •Clinical Considerations
- •Bronchial Atresia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Bronchial Tuberculosis and Mucoid Impaction
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Foreign-Body Aspiration
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Allergic Bronchopulmonary Aspergillosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •11: Lobar Atelectasis Sign
- •Disease Causing the Sign
- •Distribution
- •Clinical Considerations
- •Right Upper Lobar Atelectasis
- •Left Upper Lobar Atelectasis
- •Right Middle Lobar Atelectasis
- •Lower Lobar Atelectasis
- •References
- •Cavity
- •Diseases Causing the Cavity
- •Distribution
- •Clinical Considerations
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Langerhans Cell Histiocytosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Septic Pulmonary Embolism
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Cavitary Pulmonary Tuberculosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Paragonimiasis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Cyst
- •Diseases Causing the Cyst
- •Distribution
- •Clinical Considerations
- •Blebs and Bullae
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Pulmonary Sequestration
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Intrapulmonary Bronchogenic Cyst
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Traumatic Lung Cysts
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •References
- •Mosaic Attenuation
- •Diseases Causing the Mosaic Attenuation Pattern
- •Distribution
- •Clinical Considerations
- •Cystic Fibrosis
- •Pathology and Pathogenesis
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Constrictive Bronchiolitis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Chronic Pulmonary Thromboembolism
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Idiopathic Pulmonary Arterial Hypertension
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Airway Disease (Bronchiectasis and Bronchiolectasis)
- •Distribution
- •Clinical Considerations
- •Swyer-James-MacLeod Syndrome
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Dyskinetic Cilia Syndrome
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •14: Air-Crescent Sign
- •Diseases Causing the Sign
- •Distribution
- •Clinical Considerations
- •Aspergilloma
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Rasmussen’s Aneurysm
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •15: Signet Ring Sign
- •Diseases Causing the Sign
- •Distribution
- •Clinical Considerations
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •16: Interlobular Septal Thickening
- •Smooth Septal Thickening
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Pulmonary Edema
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Niemann–Pick Disease
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •Nodular Septal Thickening
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Pulmonary Lymphangitic Carcinomatosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT-Pathology Comparisons
- •Patient Prognosis
- •References
- •17: Honeycombing
- •Honeycombing with Subpleural or Basal Predominance
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Asbestosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Honeycombing with Upper Lung Zone Predominance
- •Diseases Causing the Pattern and Distribution
- •Distribution
- •Clinical Considerations
- •Idiopathic Familial Pulmonary Fibrosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Chronic Hypersensitivity Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •End-stage Fibrotic Pulmonary Sarcoidosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •18: Small Nodules
- •Small Nodules with Centrilobular Distribution
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Mycoplasma Pneumoniae Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Diffuse Panbronchiolitis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Follicular Bronchiolitis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pulmonary Tumor Embolism
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Pneumoconiosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pulmonary Sarcoidosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pulmonary Alveoloseptal Amyloidosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Small Nodules with Random (Miliary) Distribution
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Miliary Tuberculosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Miliary Metastasis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •19: Multiple Nodular or Mass(-like) Pattern
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Pulmonary Metastasis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pulmonary Lymphoma
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Amyloidomas
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •ANCA-Associated Granulomatous Vasculitis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •Ground-Glass Opacity with Reticulation and Fibrosis
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Ground-Glass Opacity with Reticulation, but without Fibrosis (Crazy-Paving Appearance)
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Pneumocystis jirovecii Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Lipoid Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pulmonary Alveolar Proteinosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Mucinous Adenocarcinoma or Adenocarcinoma in Situ, Diffuse Form
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Desquamative Interstitial Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Ground-Glass Opacity without Reticulation, with Small Nodules
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Subacute Hypersensitivity Pneumonitis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Cytomegalovirus Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Diffuse Alveolar Hemorrhage
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Ground-Glass Opacity without Reticulation, Diffuse Distribution
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Acute Hypersensitivity Pneumonitis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Acute Eosinophilic Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •22: Consolidation
- •Consolidation with Subpleural or Patchy Distribution
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Cryptogenic Organizing Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Chronic Eosinophilic Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Churg–Strauss Syndrome
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Radiation Pneumonitis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Consolidation with Diffuse Distribution
- •Diseases Causing the Pattern
- •Distribution
- •Clinical Considerations
- •Viral Pneumonias
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Acute Interstitial Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Diffuse Alveolar Hemorrhage
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •23: Decreased Opacity with Cystic Walls
- •Cavities
- •Diseases Causing Cavities
- •Distribution
- •Clinical Considerations
- •Rheumatoid Lung Nodules
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Cavitary Metastasis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Cysts
- •Diseases Causing Multiple Cysts
- •Distribution
- •Clinical Considerations
- •Lymphangioleiomyomatosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Lymphocytic Interstitial Pneumonia
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •Emphysema
- •Distribution
- •Clinical Considerations
- •Centrilobular Emphysema
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •Patient Prognosis
- •Paraseptal Emphysema
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •Patient Prognosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •Patient Prognosis
- •References
- •24: Decreased Opacity without Cystic Walls
- •Mosaic Attenuation, Vascular
- •Distribution
- •Clinical Considerations
- •Airway Diseases Causing Mosaic Attenuation
- •Distribution
- •Clinical Considerations
- •Asthma
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •Distribution
- •Clinical Considerations
- •Cystic Fibrosis
- •Pathology and Pathogenesis
- •Symptoms and Signs
- •CT Findings
- •CT–Pathology Comparisons
- •Patient Prognosis
- •References
- •26: Pneumonia
- •Lobar Pneumonia
- •Bronchopneumonia
- •Interstitial Pneumonia
- •27: Drug-Induced Lung Disease
- •Interstitial Pneumonitis and Fibrosis
- •Eosinophilic Pneumonia
- •Cryptogenic Organizing Pneumonia
- •Diffuse Alveolar Damage
- •Hypersensitivity Pneumonia
- •References
- •Systemic Lupus Erythematosus (SLE)
- •Rheumatoid Arthritis (RA)
- •Progressive Systemic Sclerosis (PSS)
- •Sjögren’s Syndrome
- •Mixed Connective Tissue Disease
- •Ankylosing Spondylitis
- •References

Invasive Mucinous Adenocarcinoma |
35 |
|
|
a |
b |
Fig. 3.2 Segmental pneumonia as community-acquired pneumonia in a 38-year-old man. (a, b) Transverse (a, 2.5-mm section thickness) and coronal (b, 2.0-mm section thickness) reformatted CT images show
Table 3.1 Common diseases manifesting as lobar consolidation
Disease |
Key points for differential diagnosis |
Lobar pneumonia |
Acute pneumonia symptoms, homogeneous |
|
airspace consolidation with air |
|
bronchograms |
Mucinous |
Consolidation; stretching, squeezing, and |
adenocarcinoma |
widening of the branching angle of CT |
|
air-bronchogram sign and bulging of the |
|
surrounding interlobar Þssure; MRI white |
|
lung sign |
BALT lymphoma |
Indolent and slow progressive nature of |
|
consolidative lesion |
Pulmonary infarction |
Peripheral wedge-shaped consolidation with |
|
central lucencies |
Note: BALT bronchus-associated lymphoid tissue
CT Findings
On CT, homogeneous airspace consolidation involving adjacent segments of a lobe is the predominant Þnding of lobar pneumonia [7] (Figs. 3.1 and 3.2). Areas of groundglass attenuation can be seen adjacent to the airspace consolidation. The consolidation typically extends across lobular and segmental boundaries. Air bronchograms are usually seen.
CT–Pathology Comparisons
Lobar pneumonia is characterized histologically by Þlling of alveolar airspaces by an exudate of edema ßuid and neutrophils. This Þlling usually begins at the periphery of the lung
segmental consolidation in posterior segment of the right upper lobe. Please note CT air-bronchogram signs (arrows). Patient proved to have
Streptococcus pneumoniae pneumonia
adjacent to the visceral pleura and spreads via interalveolar pores and small airways centripetally, resulting in a homogeneous area of consolidation. Incomplete Þlling of alveoli can be seen as areas of ground-glass opacity. The bronchi remain Þlled with gas and become surrounded by the expanding inßammatory exudates and thus are often seen as air bronchograms on CT scans (Figs. 3.1 and 3.2).
Patient Prognosis
Prognosis depends on the severity of pneumonia. Pneumonia severity index (PSI) is a point scoring system to assess the risk of death due to pneumonia, including age, comorbid illnesses, physical examination Þndings, and laboratory Þndings [12]. CURB-65 is another useful scoring system [13]. Early adequate antibiotic administration and management stratiÞcation according to the scoring system are essential in the treatment of pneumonia.
Invasive Mucinous Adenocarcinoma
Pathology and Pathogenesis
Invasive mucinous adenocarcinoma (formerly mucinous BAC) has a distinctive histologic appearance with tumor cells having a goblet or columnar cell morphology with abundant intracytoplasmic mucin (Figs. 3.3 and 3.4). There is a strong tendency for multicentric, multilobar, and bilateral lung involvement, which may reßect aerogenous spread. They show frequent KRAS mutation [14].
36 |
3 Consolidation |
|
|
a |
b |
c |
d |
e
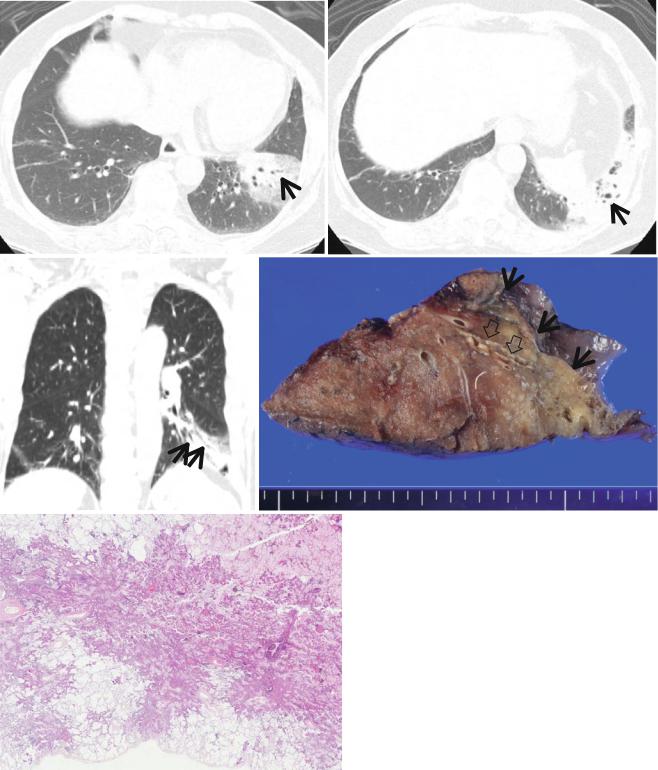
Fig. 3.3 Lobar mucinous adenocarcinoma in a 75-year-old woman. (a, b) Transverse CT scans (5.0-mm section thickness) obtained at levels of liver (a) and splenic (b) domes, respectively, show non-segmental parenchymal consolidation and internal CT air-bronchogram signs (arrows) in the left lower lobe. Also note decreased lobar volume in the same lobe. (c) Coronal reformatted image shows parenchymal consolidation in the left lower lobe with CT air-bronchogram signs (arrows). (d) Gross pathologic specimen obtained with left lower lobectomy
demonstrates a yellow-to-brown and somewhat myxoid tumor (arrows) in the left lower lobe. Also note the dilated bronchus with wall destruction (open arrows) within tumor. (e) High-magniÞcation (×100) photomicrograph shows lack of circumscribed border with permeative tumor spread to adjacent lung parenchyma. Alveolar spaces often contain mucin. Tumor has a distinctive appearance with neoplastic cells having a goblet or columnar morphology with abundant intracytoplasmic mucin

Invasive Mucinous Adenocarcinoma |
37 |
|
|
a |
b |
Fig. 3.4 Diffuse adenocarcinoma in a 57-year-old woman. (a, b) CT scans (5.0-mm section thickness) obtained at levels of the basal segmental bronchi (a) and suprahepatic inferior vena cava (b), respectively, show parenchymal opacity (consolidation and ground-glass opacity) in
the right lower lobe and in a portion of the right middle lobe. Also note CT air-bronchogram signs within lesions. Biopsy specimen obtained from the right lower lobe disclosed adenocarcinoma of moderate differentiation with tumor pleural invasion
a |
b |
c
Fig. 3.5 Bronchus-associated lymphoid tissue lymphoma in a 60-year- old man. (a) Thin-section (1.5-mm section thickness) CT scan obtained at level of the inferior pulmonary veins shows parenchymal consolidation and ground-glass opacity (arrows) in lateral segment of the right middle lobe. Also note small rectangular consolidative lesion (open arrow) in medial segment of the same lobe. (b) Cut surface of gross pathologic specimen obtained with right middle lobectomy demonstrates ill-deÞned
gray-tan consolidative lesion (arrows). Please note central solid area. (c) Low-magniÞcation (×5) photomicrograph discloses tumor expansion from bronchovascular interstitium to alveolar space to form consolidative lesion (arrows) in the right half of specimen. In the left half, tumor cells are conÞned to bronchovascular interstitium only to appear as small centrilobular nodules (open arrows). Also note thickened interlobular septa and venules (arrowheads) with tumor cell inÞltration
38 |
3 Consolidation |
|
|
Symptoms and Signs
Due to abundant mucin production of the cancer cells, patients with invasive mucinous adenocarcinoma can complain of copious amount of sputum, the so-called bronchorrhea. Otherwise, patients may be asymptomatic. As disease progresses to the bilateral lung, shortness of breath develops.
CT Findings
The CT Þndings of invasive mucinous adenocarcinoma include consolidations, air bronchograms, and multifocal and sometimes multilobar solid and subsolid nodules or masses, which tend to be centrilobular or bronchocentric [15, 16]. Stretching, squeezing, and widening of the branching angle of CT air-bronchogram sign and bulging of the surrounding interlobar Þssure may be helpful in the diagnosis of lobar mucinous adenocarcinoma [4] (Figs. 3.3 and 3.4). MRI white lung sign (bright high signal intensity on water-sensitive sequences) is also useful in the differential diagnosis between mucinous adenocarcinoma and infectious pneumonia [8].
CT–Pathology Comparisons
The CT features of invasive mucinous adenocarcinoma showing airspace consolidation and air bronchograms are caused by tumor growth along the alveolar wall (lepidic growth) combined with secretion of mucin [17, 18] (Figs. 3.3 and 3.4). As the tumor Þlls the alveolar spaces and inÞltrates the alveolar septa and bronchial walls, the bronchus becomes stretched, squeezed, and rigid [4]. Production of mucin may result in expansion of the lobe, leading to bulging of interlobar Þssures. MRI white lung sign is related to the high intratumoral content of mucin.
Bronchus-Associated Lymphoid Tissue
(BALT) Lymphoma
Pathology and Pathogenesis
Pulmonary marginal zone B-cell lymphoma of bronchusassociated lymphoid tissue (BALT) is an extranodal lymphoma, which is thought to arise in acquired BALT secondary to inßammatory or autoimmune processes. The neoplastic cells inÞltrate the bronchiolar epithelium, forming lymphoepithelial lesion. They typically show a yellow-gray consolidative mass and appear as diffuse inÞltrate of small lymphoid cells [5] (Fig. 3.5).
Symptoms and Signs
In BALT lymphoma of lobar consolidation type, constitutional symptoms such as weight loss, night sweating, and fever are more common than respiratory symptoms. Chronic cough and dyspnea are the main respiratory symptoms.
CT Findings
The main CT Þndings of BALT lymphoma are airspace consolidation or nodules containing air bronchograms within the lesions [5]. The lesions are usually multiple and bilateral (Fig. 3.5). Other Þndings include single nodule (also note section ÒSolitary Pulmonary Nodule (SPN), SolidÓ in Chap. 1), bronchiectasis and bronchiolitis, and diffuse interstitial lung disease pattern. Indolent and slow progressive nature of consolidative lesion may help make a diagnosis of bronchus-associated lymphoid tissue lymphoma.
Patient Prognosis
Invasive mucinous adenocarcinoma has a strong tendency for multifocal, multilobar, and bilateral lung involvement, which may reßect aerogenous spread. Even if surgically resected in the localized stage, it frequently recurs in the remaining lung. Mucinous adenocarcinoma is essentially insensitive to EGFR-targeted therapy [19]. The overall prognosis for patients with invasive mucinous adenocarcinoma is worse than for those with the nonmucinous adenocarcinoma.
CT–Pathology Comparisons
CT Þndings of BALT lymphoma showing solitary or multifocal nodules or masses and areas of airspace consolidation are related to proliferation of tumor cells within the interstitium such that the alveolar airspaces and transitional airways are obliterated [20] (Fig. 3.5). Because the bronchi and membranous bronchioles tend to be unaffected, an air bronchogram is common. Interlobular septal thickening, centrilobular nodules, and bronchial wall thickening on CT images are related to perilymphatic interstitial inÞltration of tumor cells.
