
- •Adrenaline (again)
- •Adrenergic receptor agonists and antagonists
- •Acetylcholine receptors
- •Acetylcholine
- •Cholinergic receptor subtypes
- •Nicotinic receptors
- •Muscarinic receptors
- •Nicotinic receptors are ion channels
- •Architecture of the nicotinic receptor
- •Other ligand-gated ion channels
- •The 7TM superfamily of G-protein-linked receptors
- •Categories of 7TM receptor
- •Receptor diversity: variation and specialization
- •Binding of low-molecular-mass ligands
- •Calcium sensors and metabotropic receptors
- •Proteinase-activated receptors (PARs)
- •The adhesion receptor subfamily
- •Frizzled
- •Receptor–ligand interaction and receptor activation
- •A two-state equilibrium description of receptor activation
- •Receptor dimerization
- •Transmitting signals into cells
- •The receptor and the effector: one and the same or separate entities?
- •Mixing and matching receptors and effectors
- •Intracellular 7TM receptor domains and signal transmission
- •Adrenaline (yet again)
- •References

Chapter 3
Receptors
But when the blast of war blows in our ears, Then imitate the action of the tiger; Stiffen the sinews, summon up the blood, Disguise fair nature with hard-favour’d rage; Then lend the eye a terrible aspect …
William Shakespeare, Henry V, II.ii.1
Here we begin with a description of the receptors for the catecholamines (adrenaline, noradrenaline, and dopamine) and for acetylcholine.
These provide the basic paradigms by which the main classes of hormone, neurotransmitter, and drug receptors have been defined.
Adrenaline (again)
Adrenaline (epinephrine) is the hormone that is secreted in anticipation of danger, preparing the body for fight or flight.1
As Cannon has pointed out, this secretion (the internal secretion of the medulla of the suprarenal bodies) is poured into the blood during
conditions of stress, anger, or fear, and acts as a potent reinforcement to
37

Signal Transduction
the energies of the body. It increases the tone of the blood vessels as well as the power of the heart’s contraction, while it mobilizes the sugar bound up in the liver, so that the muscles may be supplied with the most readily available source of energy in the struggle to which these emotional states are the essential precursors or concomitants.2
The immediate actions are those of arousal: the sweat glands sweat, body hair stands on end, the pupils dilate to gather more light, the bronchi dilate to improve oxygen supply, the heart quickens and increases its force of contraction. Then, through dilatation of relevant vessels and constriction of others, the blood supply to the myocardium and selected skeletal muscles is increased, while the supply to the skin and visceral organs is reduced, postponing digestive and anabolic processes. Metabolic fuel stores are also mobilized (initially breakdown of glycogen in the liver and muscles, and ultimately the catabolism of fat). Thus the secretion of adrenaline is familiar in the context of emergencies. However, it important to remember that the adrenal gland continuously produces low levels of the hormone and that adrenaline is also released into the circulation during exercise.
Adrenaline belongs to the group of hormones and neurotransmitters known as catecholamines. The other members are dopamine and noradrenaline. Their structures are shown in Table 2.2, page 24. The precursor from which they are
derived by a sequence of steps, is the amino acid L-tyrosine. With a few exceptions (the extracellular Ca2 sensor and the receptors for the amino acid glycine are examples), receptors are stereospecific. The catecholamines are recognized only as their L-enantiomers. Adrenaline differs from noradrenaline by the presence
of an N-methyl group on the side chain. In humans, the chromaffin cells of the adrenal medulla store and secrete both adrenaline ( 80%) and noradrenaline ( 20%), and noradrenaline is also secreted by sympathetic neurons.
-and -adrenergic receptors
The receptors that respond to adrenaline or noradrenaline are called adrenergic receptors and they are present in a wide range of tissues. They may be divided into two major classes, and , although as shown in Table 3.1, these elude any precise definition, either by their location or by the effects they elicit. Nor are they defined by their affinity for their natural first messengers: the differences in their sensitivity to adrenaline and noradrenaline are not large.
Adrenergic receptor agonists and antagonists
Agonists
What must characterize the different adrenergic receptors ultimately are the differences in their molecular structures. Knowledge in this area is still only partial, however, but we do have information from their interactions with
38
Receptors
Table 3.1 Properties that distinguish and receptors
|
receptors |
receptors |
|
|
|
Arteriolar smooth muscle |
vasoconstriction in viscera (other |
vasodilation in skeletal musculature |
|
than liver) |
and liver ( 2) |
Bronchial smooth muscle |
(not present) |
bronchodilation ( 2) |
|
|
|
Uterine smooth muscle |
contraction ( 1) |
relaxation ( 2) |
(myometrium) |
|
|
|
|
|
Heart |
|
inotropic effect (increased cardiac |
|
|
contractility) ( 1) |
|
|
increased heart rate ( 1) |
Eye |
pupillary dilation ( 1) |
lowering of intraocular pressure ( 2) |
|
|
|
Skeletal muscle |
|
glycogenolysis ( 2) |
|
|
|
Liver |
glycogenolysis ( 1) |
glycogenolysis ( 2) |
|
|
|
Adipose tissue |
inhibition of lipolysis ( 2) |
lipolysis ( 1) |
|
|
|
Pancreas |
inhibition of insulin secretion ( 2) |
insulin secretion ( 2) |
|
|
|
Platelets |
inhibition of aggregation ( 2) |
|
|
|
|
Order of potency |
adr nor iso |
iso adr nor |
Abbreviations: adr, adrenaline; iso, isoprenaline; nor, noradrenaline.
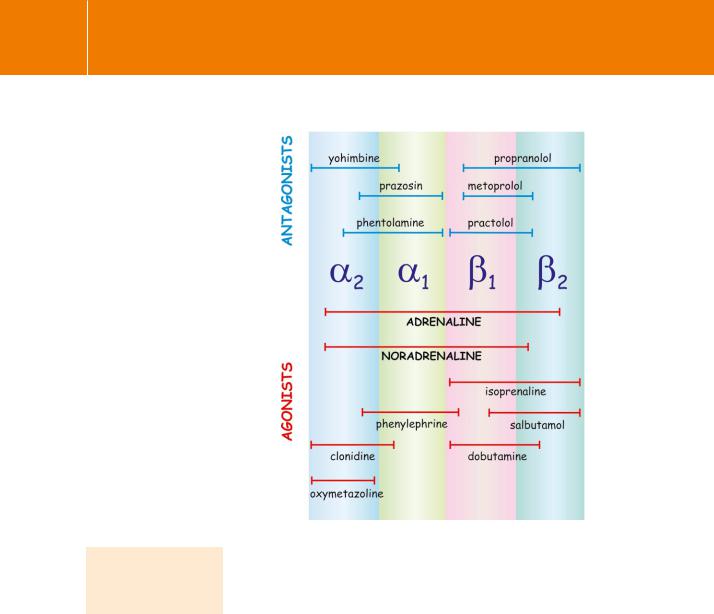
synthetic ligands that act as agonists or antagonists. In fact, they may be further subdivided on this basis, into four well-characterized subtypes 1, 2,
1 and 2 (Figure 3.1).
Although a particular subtype, by virtue of its dominance in a given tissue, may mediate a particular response, what really distinguishes them is their responsiveness to synthetic agonists, such as isoprenaline (isoproterenol) which causes blood vessels to constrict ( ), and phenylephrine ( ) which causes them to dilate. Adrenaline can do either, depending on the particular vessel. Clonidine ( 2) and salbutamol ( 2) are even more specific, since they can distinguish particular subtypes.
Antagonists
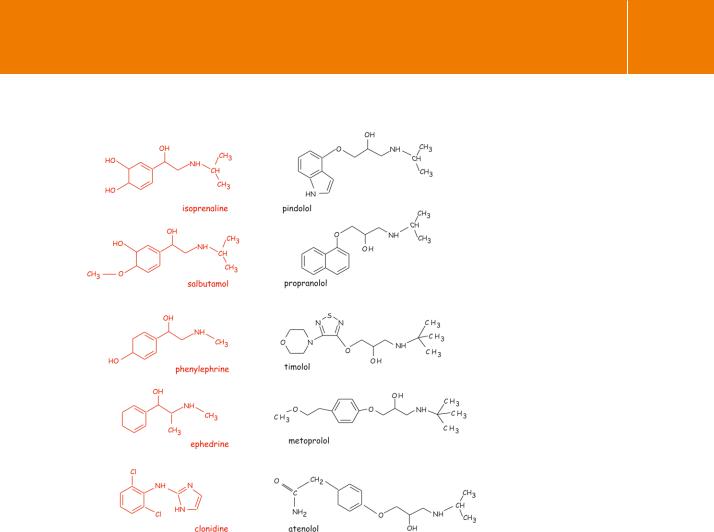
As indicated in Figure 3.1, there are also synthetic antagonists. The structures of some selected examples are shown in Figure 3.2. Propranolol inhibits the action of -receptors. This drug finds application in the treatment of some forms of hypertension, probably because it inhibits the secretion of the peptide hormone renin from the juxtaglomerular apparatus of the kidney.
Molecular cloning has confirmed the existence of 3 adrenergic receptors. Like 1 and 2 receptors, these are linked to adenylyl cyclase through the G protein Gs, but differ in not being subject to phosphorylation by protein kinase A (PKA)
or G protein receptor kinase (GRK2/ ARK). They possess their own characteristic profile of specific activators and inhibitors. They are
expressed predominantly in adipose tissues, where
39
Signal Transduction
Fig 3.1 Adrenergic receptor agonists and antagonists.
Horizontal lines indicate approximate specificities. Note that at high concentrations the selectivities tend to be reduced. Adapted from Hanoune.4
they play an important role in the regulation of lipid metabolism. For review see Strosberg.3
Renin is required for the formation of angiotensin from angiotensinogen. There are other -blockers, such as practolol and metoprolol, which at low concentrations are selective for 1-receptors. Thus, in principle, it should be possible to devise specific 1 antagonists (to suppress cAMP and with which one could treat a heart patient without exacerbating his asthma; (activation of 2-receptors in the lung would cause bronchoconstriction). However, this is not practicable because the selectivity between receptor subtypes
is rarely perfect, especially at higher dose levels. Also, other factors such as the availability of the free form (not bound to plasma proteins), the tissue distribution, in vivo half-life, and toxicity have to be taken into account before drugs can be used in clinical practice. Indeed, the first -blockers failed to reach the clinic because they were found to induce tumours in mice.
How do receptors distinguish agonists from antagonists?
Why do some compounds (such as salbutamol) cause activation whereas others (such as propranolol) are inhibitors of -adrenergic receptor function? Certainly there are some systematic structural features that appear to determine their biological effects. In general, it is found that increasing the substitution on the
40
Receptors
Fig 3.2 Some drugs that interact with adrenergic receptors.
As the substitution of the amine nitrogen on the agonists (in red) is increased, their selectivity for - over-receptors increases. Some of the-adrenergic agonists and all the-blocking agents (in black) lack the catechol nucleus. The antagonists are also characterized by the insertion
of an ether linkage ( -O(CH2)-) in the lateral chain. The structures of the physiological catecholamines adrenaline, noradrenaline, and dopamine are shown in Table 2.1, page 22.
amine nitrogen atom of catecholamines increases the preference for - over-receptors. The -blockers are all characterized by the absence of the catechol nucleus (aromatic ring with neighbouring hydroxyls) and by the presence of an -OCH2- group linking the side chain to the aromatic moiety.
An indication that the interaction of ligands with -receptors differs for agonists and antagonists is given by the finding that reducing the temperature increases the binding affinity of agonists such as isoprenaline, but has little effect on the binding of antagonists such as practolol. A temperature-dependent increase
in affinity indicates an equilibrium shift characteristic of an enthalpy-driven reaction, whereas an insensitivity to temperature suggests that a change in entropy is the main driving force. Indeed, estimates of the thermodynamic parameters reveal that the antagonists bind with an increase in entropy which is to be expected when water molecules organized around a binding site are
displaced. The agonists mostly show a decrease in entropy on binding. This might mean that although the two classes of ligand occupy the same binding pockets within the receptor molecule, which incidentally would explain the competitive
41
