Ghai Essential Pediatrics8th
.pdf



- E ss |
e |
n |
tia |
l P |
e |
iat |
|
|
|
|||
L...; |
: |
|
|
|
|
.. d |
|
ric |
________________________________ |
|||
|
:;:;:,:.:.;;;,;:.;..; |
:.;;:;.;:.:.;.;.:.;;;s |
_ |
|
||||||||
megaly with pulmonary venous hypertension. Echo |
Anomalous Left Coronary Artery |
|||||||||||
cardiogram confirms dilated ventricular cavity without |
from Pulmonary Artery (ALCAPA) |
|||||||||||
hypertrophy of the free wall of the left ventricle or the |
ALCAPA needs specific mention as a cause of congestive |
|||||||||||
septum. The left ventricular contractility is reduced. |
||||||||||||
cardiomyopathy. The diagnosis is likely in a patient with |
||||||||||||
Treatment consists in decongestive therapy with vaso |
||||||||||||
congestive cardiomyopathy with or without a murmur |
||||||||||||
dilators,especiallyACEinhibitors.Beta-blockerscontrolthe |
||||||||||||
suggesting MR and a pattern on electorcardiogram that |
||||||||||||
heartrate,reducevasoconstrictioncausedbycatecholamines |
||||||||||||
suggests anterolateral myocardial infarction (Fig. 15.45). |
||||||||||||
and upgrade beta-receptors. These agents are expected to |
||||||||||||
Echocardiographyshows alarge rightcoronaryarteryand |
||||||||||||
prevent or retard myocardial damage related to high |
||||||||||||
absence of the originofleft coronary arteryfromthe aorta. |
||||||||||||
catecholaminelevels. Carvedilol, a beta-blocker withperi |
||||||||||||
The left coronary artery is seen to arise from the pul |
||||||||||||
pheral vasodilator effect, has shown utility inthe manage |
||||||||||||
monary artery and shows flow in the reverse direction in |
||||||||||||
ment of CCF. Though experience in children is limited, it |
||||||||||||
the left anterior descending artery and the left circumflex |
||||||||||||
should be considered in presence of disproportionate |
||||||||||||
artery. This flow reversal results from collateral flow into |
||||||||||||
tachycardia.ThestartingdoseisO.l mg/kg/dayoncedaily, |
||||||||||||
the left coronary system from the right coronary artery. |
||||||||||||
which is gradually increased up to 0.5 mg/kg/day. |
Angiography is rarely necessary for the diagnosis. The |
|||||||||||
Gradual improvement occurs in a significant pro |
treatment is surgical and requires mobilization and |
|||||||||||
portion of patients. The prognosis for individual patients |
translocating the origin from pulmonary artery to aorta. |
|||||||||||
cannot be predicted and treatment should continue for |
Restrictive Cardiomyopathy (RCM) |
|||||||||||
prolonged periods. |
|
|
|
|
|
|||||||
|
|
|
|
|
Itis relativelyuncommonin children. Restrictionto ventri |
|||||||
Despiteaggressivetherapy,abouta thirdofchildrenwith |
||||||||||||
cular filling is usually associated with either endomyo |
||||||||||||
cardiomyopathy continue to deteriorate with time and |
||||||||||||
cardialfibrosis or endocardial fibroelastosis with a normal |
||||||||||||
eventually become refractory. Intermittent (weekly or bi |
||||||||||||
or smaller than normal left ventricle. Endomyocardial |
||||||||||||
weekly) dopamine or dobutarnine infusions may be used |
||||||||||||
fibrosiswas previously endemic in the state of Keralaand |
||||||||||||
effectively in some patients. It is important to consider a |
||||||||||||
is now quite rare anywhere inthecountry.Pathologically, |
||||||||||||
number of correctable conditions that can masquerade as |
||||||||||||
there is dense fibrosis in the apical and inflow regions of |
||||||||||||
cardiomyopathy (Table 15.23) and correct them. |
||||||||||||
the left and right ventricles. Fibrosis restricts the ventri |
||||||||||||
Clues to presence of these conditions may be obtained |
||||||||||||
cular filling in diastole. Papillary muscles and chordae |
||||||||||||
from clinical examination, laboratory profile or ECG |
may be tethered by the connective tissue, resulting in |
|||||||||||
(Fig. 15.44). |
|
|
|
|
|
|
|
|
|
|
severe mitral or tricuspid regurgitation. |
|
|
|
|
II |
|
|
|
|
|
|
|
|
|
·· |
|
|
|
|
|
|
-- |
-r |
|
|
|
|
-,- |
|
|
|
|
|
|
|
|
' |
|
|
|
|
|
|
|
|
- |
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
,_ |
|
- |
|
,_,..,-- |
|
-,-,- |
_,_ ....... |
- |
,...,, |
,_ |
_...,...... |
,,__ |
... |
|
|
|
|
1- |
|
- • |
I< |
|
|
|||||||||||||||||||||||||
IJ'al -,-,.., |
-- |
|
|
. -- |
|
|
,-. |
|
|
|
|
|
|
|
|
|
|
|
|
,. |
- |
|
|
|
|
|
|
|
|
|
|
|
|
.... |
|
|
|
|
|
(t ) |
|
|
|
|
I |
|
|||||||||||
1.L, |
& |
|
r\.i"', |
,h |
|
"" |
1 |
|
.., |
" |
|
... |
' |
|
|
|
|
|
"I\. |
|
- |
|
|
|
|
|
|
|
|
|
.. |
|
|
|
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||
I |
|
|
|
|
,- |
-'- |
|
|
|
|
|
|
- |
|
|
|
. |
|
|
|
|
- |
|
|
|
'\I"\ |
|
|
I"\ I |
"' |
i |
|
-- |
J;,, |
|
|
|
|
|
|
|
'I |
|||||||||||||||
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
. |
|
|
. |
|
, |
|
|
|
|
|
|
|
|
|
|
|
" |
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
. |
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
... |
|
J |
|
|
|
... |
|
|
|
|
|
|
- |
. - |
|
|
|
|
|
. |
|
|
|
|
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
I• |
|
|
I |
||||||||||||||
|
|
|
|
l•l- |
._ I;_ |
|
|
|
'-L. |
|
|
|
|
|
|
|
- .... |
|
|
. |
|
|
|
|
- |
. |
|
- |
|
|
|
|
|||||||||||||||||||||||||
|
|
|
|
|
|
|
1, - |
|
|
|
|
|
;:"" |
|
|
|
- . |
.I,.,- |
_111. |
- - •·lo-f- |
. - |
_),, |
|
- . - |
|
|
|
I |
|||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
" |
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
'"'" |
||||||||||||
....J |
|
|
|
|
|
- |
7 .... - |
- |
|
|
- |
|
,_ |
,_ |
i |
1',; |
\:, |
|
_ |
|
|
|
|
- . |
|
- |
|
,- |
|
|
|
|
|
|
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
- |
|
|
|
|
|
|
|
|
|
Jll |
|
I |
|
|
|
|
,..t.. |
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
J·- |
|
r11 |
J |
|
|
I - |
|
|
|
|
|
|
|
,_ |
|
|
|
|
|
|
|
ii,. - |
|
|
- |
|
|
- |
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
,..._,_ |
|
|
|
|
I- |
|
|
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
- |
,_ |
|
|
|
|
|
|
|
""' |
|
|
|
.L |
|
|
r |
|
|
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||
|
|
- |
. - . . |
|
|
|
|
|
|
|
|
|
|
|
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
I - |
- |
|
|
|
|
|
|
|
|
|
11 |
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
I |
||||||||||||
,- |
|
|
.. - |
|
|
|
,,, |
|
|
- |
|
|
|
-,- |
• I |
|
|
|
|
|
,- |
|
|
|
|
|
|
, |
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
- |
|
·11 |
·- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
, |
.... |
|
|
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
I |
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
|
.... |
|
. ,-. |
|
fJI,!.. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
f" , |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
- fJ |
|
|
|
v..i |
\.I |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
.... |
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
|
|
... |
·' |
|
|
|
|
|
|
I l"" |
'I |
l |
|
|
|
|
.. |
1l ... |
|
|
|||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
-. |
|
|
L, |
|
|
|
|
|
|
|
|
|
|
... |
|
|
|
|
|
||||||||||||||||||||||||||||||||||
|
ii'!=( |
|
|
"' - Iii |
|
|
|
|
. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
I |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
I ,I |
|||||||||||
, , |
|
|
|
|
- |
-- |
|
|
|
I |
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
- - |
|
|
|
l |
|
|
|
|
|
|
|
|
|
|
|
|
I |
|
|
I |
|
|||||||||||
t- - -. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
. . - |
|
- |
|
|
|
|
|||||||||||||||||||
- |
|
|
|
|
|
|
|
|
1· |
|
|
! |
|
|
., |
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
.., |
|
. |
|
|
|
I |
|
|
|
|||||||||||||||||
I |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||
Fig. 15.44: Pompe disease; Note the characteristically tall ORS voltages and very short PR interval




___E_ss_ e_ n_ _ tia_ 1_ P_ _ed_ _ ia_ tr_ -ics_ _________________________________
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
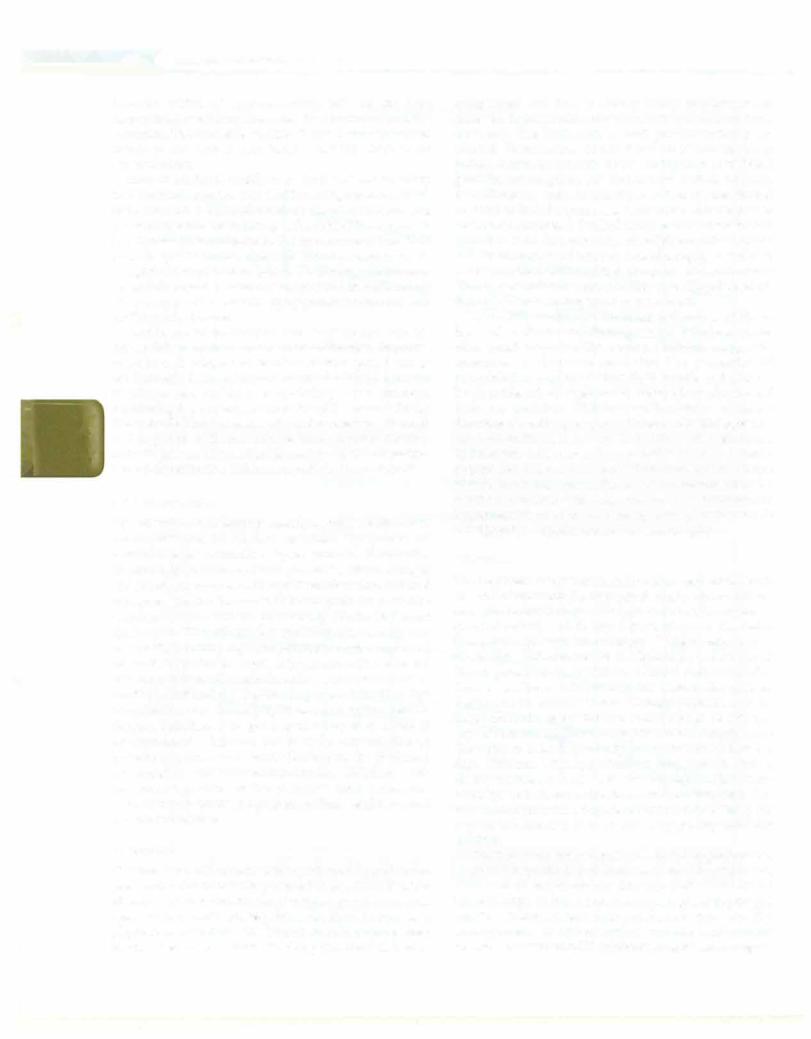
Systolic blood pressure in boys |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
- ---- |
|
|
|
|
|
|
|
|
|
|
-- |
|
|
|
- -- |
|
-------- |
|
|
|
|
|
|
|
|
|
|
|
|
-- - - 160 |
|
|||||||||||||||||||||||||||||||||||
t |
1 - |
-- |
|
1- |
|
----- |
|
|
|
|
|
|
|
|
|
|
-- |
|
|
|
|
|
|
--- |
|
|
|
|
|
|
- |
|
|
|
-- |
-- |
|
|
|
|
|
|
|
|
|
|
|
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
> |
|
- |
--f-- |
-- |
I- ,_ |
|
|
|
t |
|
|
|
|
|
t |
|
|
|
1 |
1 |
; |
|
1 |
|
|
|
+ |
|
|
1 |
|
|
|
1 |
+ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||
l- |
- |
- |
+--- |
|
|
+ |
- |
- |
-+-- |
|
|
|
+- |
- |
|
--- |
-- |
|
|
|
- |
--- |
|
|
--- |
|
|
|
- |
|
|
- |
|
|
|
|
|
|
|
--- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||
1--- |
|
|
!-- |
- |
- |
+ |
-- |
|
|
+- |
-- |
|
|
1-- |
|
|
- |
1 |
- |
|
-- |
|
|
1- |
|
|
- |
-t- |
|
- |
-- |
ll- |
|
-- |
t- |
-- |
|
|
1·-- |
|
-1 -- |
|
|
|
- |
--- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
---t--- |
|
|
i- |
- |
--1--- |
|
|
|
-+--- |
|
-- |
t |
--- |
|
|
|
- |
;- |
- |
|
- |
- |
|
|
|
|
|
-- |
|
|
- |
|
|
|
|
-- |
|
|
|
- |
|
- |
|
-- |
|
|
|
|
|
|
-- |
|
|
|
|
|
150 |
|
||||||||||||||||
-1 |
--- |
|
|
--- ---- ---+ + 1 |
|
|
|
- ---+ t |
--- --1 |
|
- |
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
-- -- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||
|
|
|
|
1--- ---s--- --!----l---+- |
|
|
-- |
l |
------ - ----- |
|
-- -- -- |
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
- |
|
- |
|
|
|
- - |
|
- |
|
|
|
|
|
|
|
- - |
|
|
|
|
- |
|
|
|
|
|
|
|
|
|
r"'"' |
- |
|
|
- |
- |
|
|
- |
|
|
|
|
1 0 |
|
||||||||||||||||||||||||||
l |
|
-l |
|
|
|
|
-+ |
|
|
|
|
|
|
|
|
|
-+ |
|
|
+ |
|
t |
|
|
|
-+- |
-+ |
|
|
|
-+ |
|
+ |
|
|
-t |
4 |
|
|
|||||||||||||||||||||||||||||||||||
|
|
|
-+ |
|
t-- |
|
|
|
|
+ |
|
|
+ |
-- |
|
|
|
|
|
|
|
|
|
|
----,!-:;._,....'"'r'-- |
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||
1- ,--- |
--1-- |
- |
|
|
- |
|
|
-- |
1- |
|
|
- |
+- |
|
|
-- |
1--- |
|
-- |
|
1--..==L -:::;;;;; ,<-- |
|
-===-==-- |
|
=-') |
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
,_ |
|
|
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
----"r |
--- |
|
|
|
|
|
- |
-- |
|
..........._ |
|
i---- |
|
|
|
|
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
t |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
-f- - |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||
--f |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
1- I--- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
- |
|
|
|
|
|
|
|
|
|
|
- |
|
|
|
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
110 |
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
f----- --- |
|
|
|
------ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||
|
|
|
|
--- |
|
|
|
- |
-- |
|
|
|
|
|
|
|
|
-- |
|
|
|
- |
---- |
|
|
- ------- f- |
|
|
- |
|
|
- |
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||
|
|
|
|
-+- |
_-t-_-_::.::.=+-_ |
+- |
|
|
|
- - |
|
|
|
==-=-+ |
|
- |
|
|
- |
|
- |
--l |
-- |
-- |
t- |
-t- |
|
|
|
|
|
00 |
|
|||||||||||||||||||||||||||||||||||||||||
J. -:_':__':_-f |
__ |
|
|
--1 |
_ |
|
|
|
|
-+- |
|
_ -+-- |
|
|
__:t |
|
___::-_:=_-+- |
|
|
|
|
-t- |
|
|
|
|
|
|
|
---t 1 |
|
|
|
|||||||||||||||||||||||||||||||||||||||||
.. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|
|
|
+ |
|
|
|
|
|
|
|
|
|
|
|
|
|
t- -- --- --- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
1-- |
|
|
- |
;--- |
|
--- |
|
|
|
|
·-1---- |
|
|
|
|
|
|
|
|
|
|
|
|
-- |
|
|
- |
-- |
|
|
|
- |
|
--- |
|
|
|
|
|
|
|
|
|
|
|
+90 |
|
|
||||||||||||||||||||||||||
l--- |
|
|
+-- |
|
|
-+ --+ -+----- |
|
|
|
l- |
|
|
-- |
|
t- |
- |
|
-- |
ll-- |
-- |
t--- |
|
|
-t --+-- |
|
+--- |
|
|
|
+-- |
+--- |
|
|
|
+--- |
|
|
|
t--- |
|
|
|
|
|
||||||||||||||||||||||||||||||
,--- -------1 |
|
|
|
- |
|
|
- |
I- |
-- |
|
|
•-- |
|
|
|
|
|
|
------ |
|
|
--+-- |
|
|
|
1 - |
|
|
|
- - |
- |
- |
--- -- |
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||
|
-- |
|
1-- |
|
- |
- |
+- |
-- |
|
|
-+- |
- |
|
|
|
|
|
|
1 |
-- |
---;---1---i---+ |
|
- -+--+----t---+----t-80 |
|
||||||||||||||||||||||||||||||||||||||||||||||||||
t-- |
---t---+----+--+-----1---t----1 |
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
2 |
|
|
3 |
|
|
|
4 |
|
|
|
5 |
|
|
|
6 |
|
|
7 |
|
|
|
8 |
|
|
9 |
10 |
|
|
11 |
12 |
|
|
|
13 |
14 |
|
|
|
15 |
|
|
16 |
|
|
17 |
|
|
|
||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Age (yr) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
A |
|
|
|
|
|
|
|
|
|
|
|
+ 90th percentile --o- 95th percentile |
|
--1::r- |
99th percentile + 5 mm |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Diastolic blood pressure In boys |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
|
----------- |
|
--1 |
1 |
|
|
|
|
|
|
|
|
- -- -------- |
|
|
|
|
|
|
|
|
|
|
-- - -- ----- |
|
|
|
|
|
|
, |
120 |
|
|||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
- |
|
|
|
|
|
-- |
|
|
|
|
|
|
|
___, |
|
--1 |
|
|
|
|
|
|
_ |
|
|
|
|
|
|
- |
|
|
|
, |
|
|
|
|
|
_ |
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|
- |
|
|
|
|
- - |
|
|
|
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
-- -- |
|
|
|
-1- |
|
|
|
--- |
|
|
|
|
|
|
|
|
|
|
+110 |
|
|||||||||||||||||||
l--- |
|
|
+--- |
|
|
|
+--- |
+-- |
|
|
+--- |
|
|
+--- |
|
|
|
|
+--- |
|
|
+--- |
|
|
|
|
+-- |
--11---- |
|
|
|
t--- |
l |
--- |
|
+---- |
--- |
t |
|
|
|
+-- |
|
|
|
+---- |
|
|
|
|||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
t----+ |
|
i |
|
|
|
l |
|
|
|
+ |
|
|
,.100 |
|
||||||||||||||||||||||||
|
t--- |
|
|
--+- |
-- |
|
|
+-- |
--+-- |
|
|
- |
+--- |
|
- |
+-- |
|
|
- |
|
+-- |
|
|
--+---- |
|
|
|
|
1--------- |
|
1--- |
|
|
+--- |
---- |
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
-,____I----- |
|
|
|
I- |
90 |
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
_ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
,_ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
---' |
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
- :c:: ___ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||
,--- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
80 |
|
0> |
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
E |
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
:I: |
k., --"" |
+--- |
|
|
|
|
t--- |
,,.,.....=-- |
-t---- |
|
:::-4 -t--- |
|
|
|
|
t--- |
|
|
|
t--- |
|
+--- |
|
|
+--- |
|
+---- |
|
|
|
|
+- |
- --- |
|
|
|
+--- |
|
|
|
+--- |
|
|
+70 |
|
E |
|||||||||||||||||||||||||||||
..,.._,,_____,_-:a- f--_,,_--=•= |
-- |
|
|
|
t---+---·l---t---1---1---,-- ---,----- |
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
-z:::J:;:::;z ::::=1=::::::t.==::::::l ==t::::==t=:::::j:::::::t:=:::::::J:::::::::j::::::=l=::::::j::::::::::j:::::=j:::::=t 60 |
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
./ |
|
|
|
|
|
l |
|
|
+ |
|
|
|
|
|
l |
|
|
|
|
- |
--1 |
|
|
|
|
1 |
|
1 |
|
|
---- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||
|
Y-'.=,c_- - |
|
- |
|
|
|
|
- |
|
|
|
-- |
|
|
|
|
|
|
|
|
|
|
|
- |
|
|
|
-------- - --1---- |
|
- |
|
-- |
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||
......... |
+ |
|
|
+ |
+ |
|
|
+ |
|
|
|
|
|
l |
|
|
|
|
t |
|
|
1 |
|
|
|
|
t |
|
|
l |
|
|
|
+ |
t |
|
|
t |
|
|
|
|
|
+ |
|
|
|
+ |
|
|
+50 |
|
|
|||||||||||||||||||||
l---- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|
|
|
|
|
---- |
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||
1---- |
|
|
l- |
-- |
|
|
i- |
- |
--t-- |
|
- |
|
l- |
-- |
- |
|
|
l- |
---- |
|
+- |
|
---- |
+-- |
|
|
|
|
+- |
-- |
--- |
- |
1- - |
- |
- - |
-- |
|
|
|
1- |
-- |
|
|
|
|
- |
|
- |
|
- |
|
|
|
|
|
|
|
|
|
|
||||||||||||||
--1- |
|
--- -- |
|
|
|
|
|
|
|
|
|
1- |
--1-- |
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||
|
1 |
|
+ |
|
|
+ |
|
|
-1- |
|
-1-- |
|
|
|
|
|
|
|
|
|
|
- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
-- |
|
|
|
|
|
|
|
|
|
|
|
|
--+ |
|
|
|
|
t |
|
1 |
|
|
|
|
1 |
|
t |
|
|
|
l |
|
|
|
|
|
1 |
|
|
|
1 |
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
-- |
|
- |
|
|
- |
--- |
|
|
--- |
|
|
|
|
|
|
|
--- |
|
|
|
|
|
|
|
|
|
||||||||||||||
t |
|
---t |
|
|
|
|
+ |
+ |
|
|
+ |
|
|
+ |
|
|
+ |
|
|
+ |
--•--- |
|
1- |
-- |
|
|
|
1,---1---- |
|
|
|
11- |
-- ------- |
|
|
|
|
+ |
|
|
|
+- |
|
40 |
|
|||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
+----- |
|
1---- |
|
|
|
|
|
;---- |
11----- |
|
|
|
;--- |
--- |
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||
1 |
|
|
2 |
|
|
|
3 |
|
4 |
|
|
5 |
|
|
|
|
|
6 |
|
7 |
|
|
8 |
|
|
|
|
9 |
|
10 |
|
11 |
12 |
|
13 |
|
14 |
|
|
|
15 |
|
|
|
16 |
|
17 |
|
|
|
||||||||||||||||||||||||
B |
Age (yr) |
|
Figs 15.46A and B: Blood pressure levels for boys at 50th precentile for height. Chart depicting 90th (closed diamonds), 95th (open squares) and 99th + 5 mm (open triangles) percentile values for (A) systolic and (B) diastolic blood pressures, representing cut off values for the
diagnosis of pre-hypertension, stage I and stage II hypertension, respectively, in boys (based on the Fourth US Task Force Report on Hypertension).
With permission from Indian Pediatrics 2007;44: 103-21