
Borchers Andrea Ann (ed.) Handbook of Signs & Symptoms 2015
.pdf
Spinal neoplasms. Disrupting upper neuron control of the bladder, spinal neoplasms cause neurogenic bladder and resultant distention. Associated signs and symptoms include a sense of pelvic fullness, continuous overflow dribbling, back pain that typically mimics sciatica pain, constipation, tender vertebral processes, sensory deficits, and muscle weakness, flaccidity, and atrophy. Signs and symptoms of urinary tract infection (dysuria, urinary frequency and urgency, nocturia, tenesmus, hematuria, and weakness) may also occur.
Urethral calculi. With urethral calculi, urethral obstruction leads to bladder distention. The patient experiences interrupted urine flow. The obstruction causes pain radiating to the penis or vulva and referred to the perineum or rectum. It may also produce a palpable stone and urethral discharge.
Urethral stricture. Urethral stricture results in urine retention and bladder distention with chronic urethral discharge (most common sign), urinary frequency (also common), dysuria, urgency, decreased force and diameter of the urine stream, and pyuria. Urinoma and urosepsis may also develop.
Other Causes
Catheterization. Using an indwelling urinary catheter can result in urine retention and bladder distention. While the catheter is in place, inadequate drainage due to kinked tubing or an occluded lumen may lead to urine retention. In addition, a misplaced urinary catheter or

irritation with catheter removal may cause edema or spasms of the detrusor muscle and the external urethral sphincter, thereby blocking urine outflow.
Drugs. Parasympatholytics, anticholinergics, ganglionic blockers, sedatives, anesthetics, and opiates can produce urine retention and bladder distention.
Special Considerations
Monitor the patient’s vital signs and the extent of bladder distention. Encourage the patient to change positions to alleviate discomfort. He may require an analgesic.
Prepare the patient for diagnostic tests (such as endoscopy and radiologic studies) to determine the cause of bladder distention. You may need to prepare him for surgery if interventions fail to relieve bladder distention and obstruction prevents catheterization.
Patient Counseling
Teach the patient to use Valsalva’s maneuver or Credé’s method to empty the bladder. Explain how to stimulate voiding.
Pediatric Pointers
Look for urine retention and bladder distention in infants who fail to void normal amounts. (In the first 48 hours of life, infants excrete about 60 mL of urine; during the next week, they excrete about 300 mL of urine daily.) In males, posterior urethral valves, meatal stenosis, phimosis, spinal cord anomalies, bladder diverticula, and other congenital defects may cause urinary obstruction and resultant bladder distention.
REFERENCES
James, N., Hussain, S., Hall, E., et al. (2010). Results of a 2 × 2 phase III randomized trial of synchronous chemoradiotherapy (CRT) compared to radiotherapy (RT) alone and standard vs. reduced high volume RT in muscle invasive bladder cancer (MIBC) (BC2001 CRUK/01/004). International Journal of Radiation Oncology, Biology, Physics, 78(3), S2–S3.
James, N. D., Hussain, S. A., Hall, E., et al. (2012). Radiotherapy with or without chemotherapy in muscle-invasive bladder cancer. New England Journal of Medicine, 366(16), 1477–1488.
Blood Pressure Decrease[Hypotension]
Low blood pressure refers to inadequate intravascular pressure to maintain the oxygen requirements of the body’s tissues. Although commonly linked to shock, this sign may also result from a cardiovascular, respiratory, neurologic, or metabolic disorder. Hypoperfusion states especially affect the kidneys, brain, and heart and may lead to renal failure, a change in the patient’s level of consciousness (LOC), or myocardial ischemia. Low blood pressure may be drug induced or may accompany diagnostic tests — most commonly those using contrast media. It may stem from stress or change of position — specifically, rising abruptly from a supine or sitting position to a standing position (orthostatic hypotension).
Normal blood pressure varies considerably; what qualifies as low blood pressure for one person may be normal for another. Consequently, every blood pressure reading must be compared against the patient’s baseline. Typically, a reading below 90/60 mm Hg, or a drop of 30 mm Hg from the baseline, is considered low blood pressure.

Low blood pressure can reflect an expanded intravascular space (as in severe infections, allergic reactions, or adrenal insufficiency), reduced intravascular volume (as in dehydration and hemorrhage), or decreased cardiac output (as in impaired cardiac muscle contractility). Because the body’s pressure-regulating mechanisms are complex and interrelated, a combination of these factors usually contributes to low blood pressure.
 EMERGENCY INTERVENTIONS
EMERGENCY INTERVENTIONS
If the patient’s systolic pressure is less than 80 mm Hg, or 30 mm Hg below his baseline, suspect shock. Quickly evaluate the patient for a decreased LOC. Check his apical pulse for tachycardia and his respirations for tachypnea. Also, inspect the patient for cool, clammy skin. Elevate the patient’s legs above the level of his heart, or place him in Trendelenburg’s position if the bed can be adjusted. Then, start an I.V. line using a large-bore needle to replace fluids and blood or to administer drugs. Prepare to administer oxygen with mechanical ventilation, if necessary. Monitor the patient’s intake and output, and insert an indwelling urinary catheter to accurately measure urine output. The patient may also need a central venous line or a pulmonary artery catheter to facilitate monitoring his fluid status. Prepare for cardiac monitoring to evaluate cardiac rhythm. Be ready to insert a nasogastric tube to prevent aspiration in the comatose patient. Throughout emergency interventions, keep the patient’s spinal column immobile until spinal cord trauma is ruled out.
History and Physical Examination
If the patient is conscious, ask him about associated symptoms. For example, does he feel unusually weak or fatigued? Has he had nausea, vomiting, or dark or bloody stools? Is his vision blurred? Is his gait unsteady? Does he have palpitations? Does he have chest or abdominal pain or difficulty breathing? Has he had episodes of dizziness or fainting? Do these episodes occur when he stands up suddenly? If so, take the patient’s blood pressure while he’s lying down, sitting, and then standing; compare readings. (See Ensuring Accurate Blood Pressure Measurement, page 96.) A drop in systolic or diastolic pressure of 10 to 20 mm Hg or more and an increase in heart rate of more than 15 beats/minute between position changes suggest orthostatic hypotension.
Next, continue with a physical examination. Inspect the skin for pallor, sweating, and clamminess. Palpate peripheral pulses. Note paradoxical pulse — an accentuated fall in systolic pressure during inspiration — which suggests pericardial tamponade. Then, auscultate for abnormal heart sounds (gallops, murmurs), rate (bradycardia, tachycardia), or rhythm. Auscultate the lungs for abnormal breath sounds (diminished sounds, crackles, wheezing), rate (bradypnea, tachypnea), or rhythm (agonal or Cheyne-Stokes respirations). Look for signs of hemorrhage, including visible bleeding and palpable masses, bruising, and tenderness. Assess the patient for abdominal rigidity and rebound tenderness; auscultate for abnormal bowel sounds. Also, carefully assess the patient for possible sources of infection such as open wounds.
Medical Causes
Acute adrenal insufficiency. Orthostatic hypotension is characteristic with acute adrenal insufficiency, accompanied by fatigue, weakness, nausea, vomiting, abdominal discomfort,
weight loss, fever, and tachycardia. The patient may also have hyperpigmentation of fingers, nails, nipples, scars, and body folds; pale, cool, clammy skin; restlessness; decreased urine output; tachypnea; and coma.
Alcohol toxicity. Low blood pressure occurs infrequently; more commonly, alcohol toxicity produces distinct alcohol breath odor, tachycardia, bradypnea, hypothermia, a decreased LOC, seizures, a staggering gait, nausea, vomiting, diuresis, and slow, stertorous breathing.
 EXAMINATION TIP Ensuring Accurate Blood Pressure
EXAMINATION TIP Ensuring Accurate Blood Pressure
Measurement
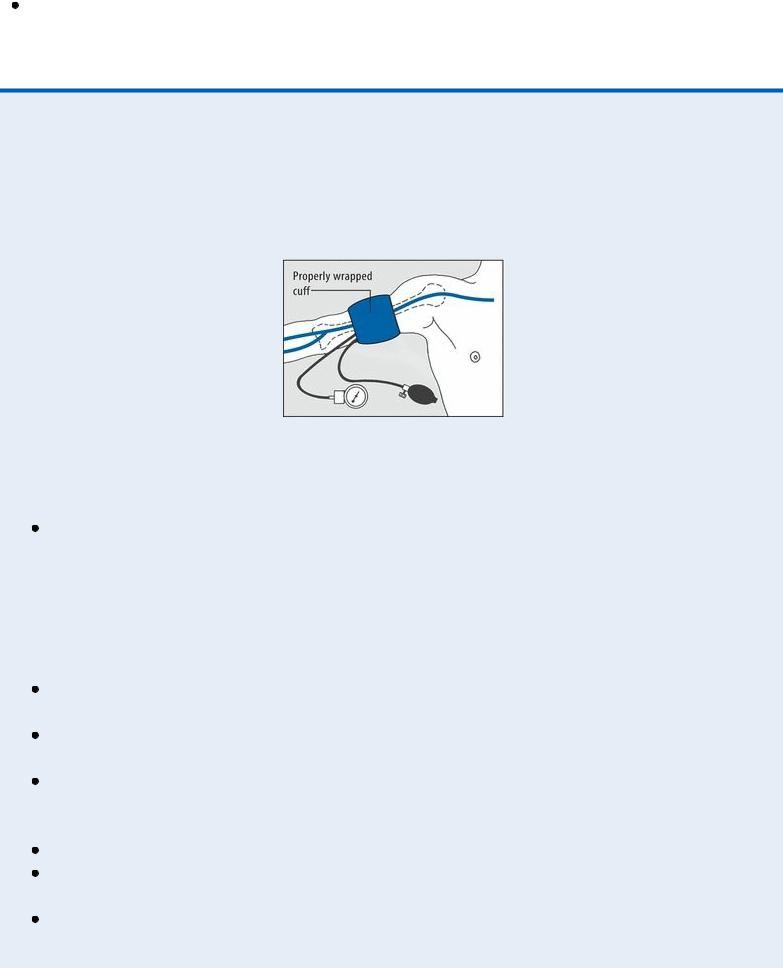
When taking the patient’s blood pressure, begin by applying the cuff properly, as shown here.
Then, be alert for these common pitfalls to avoid recording an inaccurate blood pressure measurement.
Wrong-sized cuff. Select the appropriate-sized cuff for the patient. This ensures that adequate pressure is applied to compress the brachial artery during cuff inflation. If the cuff bladder is too narrow, a false-high reading will be obtained; too wide, a false-low reading. The cuff bladder width should be about 40% of the circumference of the midpoint of the limb; bladder length should be twice the width. If the arm circumference is less than 13” (33 cm), select a regular-sized cuff; if it’s between 13” and 16” (33 to 40.5 cm), a largesized cuff; if it’s more than 16”, a thigh cuff. Pediatric cuffs are also available.
Slow cuff deflation, causing venous congestion in the extremity. Don’t deflate the cuff more slowly than 2 mm Hg/heartbeat because you’ll get a false-high reading.
Cuff wrapped too loosely, reducing its effective width. Tighten the cuff to avoid a falsehigh reading.
Mercury column not read at eye level. Read the mercury column at eye level. If the column is below eye level, you may record a false-low reading; if it’s above eye level, a false-high reading.
Tilted mercury column. Keep the mercury column vertical to avoid a false-high reading. Poorly timed measurement. Don’t take the patient’s blood pressure if he appears anxious or has just eaten or ambulated; you’ll get a false-high reading.
Incorrect position of the arm. Keep the patient’s arm level with his heart to avoid a falselow reading.
Cuff overinflation, causing venospasm or pain. Don’t overinflate the cuff because you’ll get a false-high reading.
Failure to notice an auscultatory gap (sound fades out for 10 to 15 mm Hg, then returns). To avoid missing the top Korotkoff sound, estimate systolic pressure by palpation first. Then, inflate the cuff rapidly — at a rate of 2 to 3 mm Hg/second — to about 30 mm Hg above the palpable systolic pressure.
Inaudibility of feeble sounds. Before reinflating the cuff, have the patient raise his arm to reduce venous pressure and amplify low-volume sounds. After inflating the cuff, lower the patient’s arm; then, deflate the cuff and listen. Alternatively, with the patient’s arm positioned at heart level, inflate the cuff and have the patient make a fist. Have him rapidly open and close his hand 10 times before you begin to deflate the cuff, and then listen. Make sure to document that the blood pressure reading was augmented.
Anaphylactic shock. Following exposure to an allergen, such as penicillin or insect venom, a dramatic fall in blood pressure and narrowed pulse pressure signal anaphylactic reaction. Initially, anaphylactic shock causes anxiety, restlessness, a feeling of doom, intense itching (especially of the hands and feet), and pounding headache. Later, it may also produce weakness, sweating, nasal congestion, coughing, difficulty breathing, nausea, abdominal cramps, involuntary defecation, seizures, flushing, change or loss of voice due to laryngeal edema, urinary incontinence, and tachycardia.
Anthrax (inhalation). Anthrax is an acute infectious disease that’s caused by the gram-positive, spore-forming bacterium Bacillus anthracis. Although the disease most commonly occurs in wild and domestic grazing animals, such as cattle, sheep, and goats, the spores can live in the soil for many years. The disease can occur in humans exposed to infected animals, tissue from infected animals, or biological warfare. Most natural cases occur in agricultural regions worldwide. Anthrax may occur in the cutaneous, inhalation, or GI form.
Inhalation anthrax is caused by inhalation of aerosolized spores. Initial signs and symptoms are flulike and include fever, chills, weakness, cough, and chest pain. The disease generally occurs in two stages with a period of recovery after the initial signs and symptoms. The second stage develops abruptly with rapid deterioration marked by fever, dyspnea, stridor, and hypotension, generally leading to death within 24 hours. Radiologic findings include mediastinitis and symmetric mediastinal widening.
Cardiac arrhythmias. With an arrhythmia, blood pressure may fluctuate between normal and low readings. Dizziness, chest pain, difficulty breathing, light-headedness, weakness, fatigue, and palpitations may also occur. Auscultation typically reveals an irregular rhythm and a pulse rate greater than 100 beats/minute or less than 60 beats/minute.
Cardiac contusion. With cardiac contusion, low blood pressure occurs along with tachycardia and, at times, anginal pain and dyspnea.
Cardiac tamponade. An accentuated fall in systolic pressure (more than 10 mm Hg) during inspiration, known as paradoxical pulse, is characteristic in patients with cardiac tamponade. This disorder also causes restlessness, cyanosis, tachycardia, jugular vein distention, muffled heart sounds, dyspnea, and Kussmaul’s sign (increased venous distention with inspiration).
Cardiogenic shock. A fall in systolic pressure to less than 80 mm Hg or to 30 mm Hg less than

the patient’s baseline because of decreased cardiac contractility is characteristic in patients with cardiogenic shock. Accompanying low blood pressure are tachycardia, narrowed pulse pressure, diminished Korotkoff sounds, peripheral cyanosis, and pale, cool, clammy skin. Cardiogenic shock also causes restlessness and anxiety, which may progress to disorientation and confusion. Associated signs and symptoms include angina, dyspnea, jugular vein distention, oliguria, ventricular gallop, tachypnea, and a weak, rapid pulse.
Cholera. This acute infection, caused by the bacterium Vibrio cholerae , may be mild with uncomplicated diarrhea or severe and life threatening. Cholera is spread by ingesting contaminated water or food, especially shellfish. Signs include abrupt watery diarrhea and vomiting. Severe fluid and electrolyte loss leads to thirst, weakness, muscle cramps, decreased skin turgor, oliguria, tachycardia, and hypotension. Without treatment, death can occur within hours.
Diabetic ketoacidosis. Hypovolemia triggered by osmotic diuresis in hyperglycemia is responsible for the low blood pressure associated with diabetic ketoacidosis, which is usually present in patients with type 1 diabetes mellitus. It also commonly produces polydipsia, polyuria, polyphagia, dehydration, weight loss, abdominal pain, nausea, vomiting, breath with fruity odor, Kussmaul’s respirations, tachycardia, seizures, confusion, and stupor that may progress to coma.
Heart failure. With heart failure, blood pressure may fluctuate between normal and low readings. However, a precipitous drop in blood pressure may signal cardiogenic shock. Other signs and symptoms of heart failure include exertional dyspnea, dyspnea of abrupt or gradual onset, paroxysmal nocturnal dyspnea or difficulty breathing in the supine position (orthopnea), fatigue, weight gain, pallor or cyanosis, sweating, and anxiety. Auscultation reveals ventricular gallop, tachycardia, bilateral crackles, and tachypnea. Dependent edema, jugular vein distention, increased capillary refill time, and hepatomegaly may also occur.
Hyperosmolar hyperglycemic nonketotic syndrome (HHNS). HHNS, which is common in the patient with type 2 diabetes mellitus, decreases blood pressure — at times dramatically — if he loses significant fluid from diuresis due to severe hyperglycemia and hyperosmolarity. It also produces dry mouth, poor skin turgor, tachycardia, confusion progressing to coma, and, occasionally, generalized tonic-clonic seizure.
Hypovolemic shock. A fall in systolic pressure to less than 80 mm Hg or 30 mm Hg less than the patient’s baseline, secondary to acute blood loss or dehydration, is characteristic in hypovolemic shock. Accompanying it are diminished Korotkoff sounds, a narrowed pulse pressure, and a rapid, weak, and irregular pulse. Peripheral vasoconstriction causes cyanosis of the extremities and pale, cool, clammy skin. Other signs and symptoms include oliguria, confusion, disorientation, restlessness, and anxiety.
Hypoxemia. Initially, blood pressure may be normal or slightly elevated, but as hypoxemia becomes more pronounced, blood pressure drops. The patient may also display tachycardia, tachypnea, dyspnea, and confusion and may progress from stupor to coma.
Myocardial infarction (MI). With MI, a life-threatening disorder, blood pressure may be low or high. However, a precipitous drop in blood pressure may signal cardiogenic shock. Associated signs and symptoms include chest pain that may radiate to the jaw, shoulder, arm, or epigastrium; dyspnea; anxiety; nausea or vomiting; sweating; and cool, pale, or cyanotic skin. Auscultation may reveal an atrial gallop, a murmur and, occasionally, an irregular pulse.
Neurogenic shock. The result of sympathetic denervation due to cervical injury or anesthesia,
neurogenic shock produces low blood pressure and bradycardia. However, the patient’s skin remains warm and dry because of cutaneous vasodilation and sweat gland denervation. Depending on the cause of shock, there may also be motor weakness of the limbs or diaphragm.
Pulmonary embolism. Pulmonary embolism causes sudden, sharp chest pain and dyspnea accompanied by a cough and, occasionally, a low-grade fever. Low blood pressure occurs with a narrowed pulse pressure and diminished Korotkoff sounds. Associated signs include tachycardia, tachypnea, a paradoxical pulse, jugular vein distention, and hemoptysis.
Septic shock. Initially, septic shock produces fever and chills. Low blood pressure, tachycardia, and tachypnea may also develop early, but the patient’s skin remains warm. Later, low blood pressure becomes increasingly severe — less than 80 mm Hg or 30 mm Hg less than the patient’s baseline — and is accompanied by narrowed pulse pressure. Other late signs and symptoms include pale skin, cyanotic extremities, apprehension, thirst, oliguria, and coma.
Vasovagal syncope. Vasovagal syncope is the transient loss or near loss of consciousness following stressful, painful, or claustrophobic experiences. It’s characterized by low blood pressure, pallor, cold sweats, nausea, palpitations or slowed heart rate, and weakness.
Other Causes
Diagnostic tests. Diagnostic tests include the gastric acid stimulation test using histamine and X-ray studies using contrast media. The latter may trigger an allergic reaction, which causes low blood pressure.
Drugs. Calcium channel blockers, diuretics, vasodilators, alphaand beta-adrenergic blockers, general anesthetics, opioid analgesics, monoamine oxidase inhibitors, anxiolytics (such as benzodiazepines), tranquilizers, and most I.V. antiarrhythmics (especially bretylium tosylate) can cause low blood pressure.
Special Considerations
Check the patient’s vital signs frequently to determine if low blood pressure is constant or intermittent. If blood pressure is extremely low, an arterial catheter may be inserted to allow close monitoring of pressures. Alternatively, a Doppler flowmeter may be used.
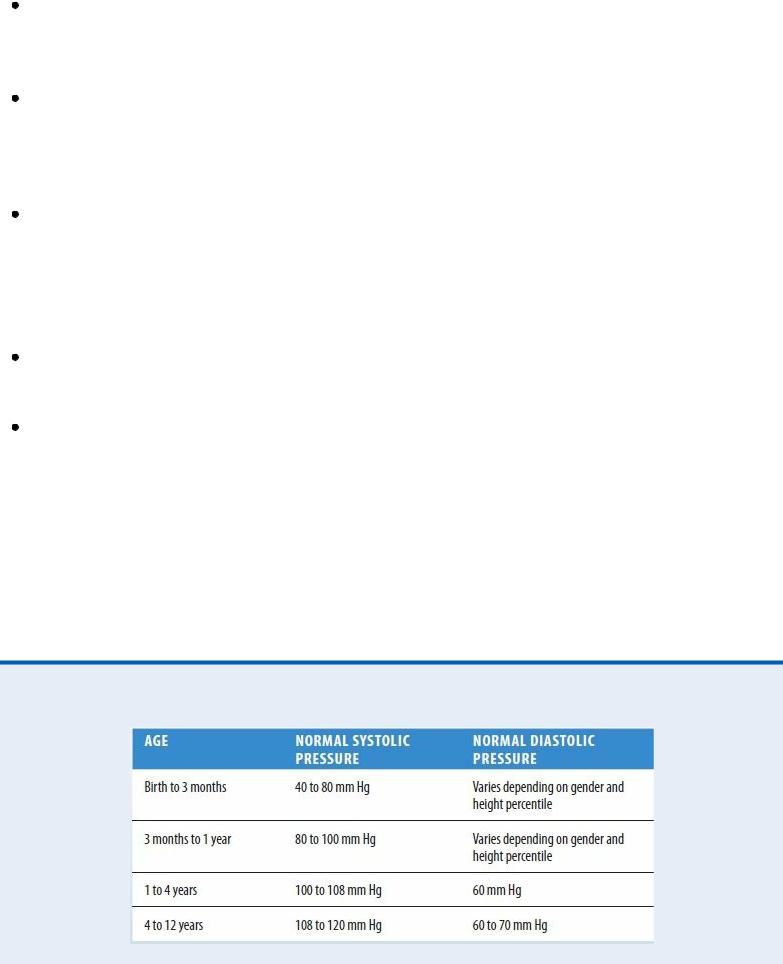
Normal Pediatric Blood Pressure
If the patient is symptomatic, place him on bed rest and keep the side rails of the bed up. If the patient is asymptomatic and ambulatory, assist him as necessary. To avoid falls, don’t leave a hypotensive patient unattended when he’s sitting or walking.
Prepare the patient for laboratory tests, which may include urinalysis, routine blood studies, an electrocardiogram, and chest, cervical, and abdominal X-rays.
Patient Counseling
Advise the patient with orthostatic hypotension to stand up slowly from a sitting or lying position, and emphasize the importance of dangling the feet and rising slowly when getting out of bed. For patients with vasovagal syncope, discuss how to avoid triggers. Also, discuss the need for a cane or a walker.
Pediatric Pointers
Normal blood pressure in children is lower than that in adults. (See Normal Pediatric Blood Pressure.)
Because accidents occur frequently in children, suspect trauma or shock first as a possible cause of low blood pressure. Remember that low blood pressure typically doesn’t accompany head injury in adults because intracranial hemorrhage is insufficient to cause hypovolemia. However, it does accompany head injury in infants and young children; their expandable cranial vaults allow significant blood loss into the cranial space, resulting in hypovolemia.
Another common cause of low blood pressure in children is dehydration, which results from failure to thrive or from persistent diarrhea and vomiting for as little as 24 hours.
Geriatric Pointers
In elderly patients, low blood pressure commonly results from the use of multiple drugs with this potential adverse effect, a problem that needs to be addressed. Orthostatic hypotension due to autonomic dysfunction is another common cause.
REFERENCES
Fan, C. W. , Walsh, C., & Cunningham, C. J. (2011) . The effect of sleeping with the head of the bed elevated six inches on elderly patients with orthostatic hypotension: An open randomised controlled trial. Age and Ageing, 40, 187–192.
Freeman, R., Wieling, W., Axelrod, F. B., Benditt, D. G., Benarroch, E., Biaggioni, I., … van Dijk, J. G. (2011). Consensus statement on the definition of orthostatic hypotension, neurally medicated syncope and the postural tachycardia syndrome. Clinical Autonomic Research, 21, 69–72.
Blood Pressure Increase[Hypertension]
Elevated blood pressure — an intermittent or sustained increase in blood pressure exceeding 140/90 mm Hg — strikes more men than women and twice as many Blacks as Whites. By itself, this common sign is easily ignored by the patient; after all, he can’t see or feel it. However, its causes can be life threatening.
 GENDER CUE
GENDER CUE
Hypertension has been reported to be two to three times more common in women taking hormonal contraceptives than those not taking them. Women age 35 and older who smoke cigarettes should be strongly encouraged to stop; if they continue to smoke, they should be discouraged from using hormonal contraceptives.
Elevated blood pressure may develop suddenly or gradually. A sudden, severe rise in pressure (exceeding 180/110 mm Hg) may indicate life-threatening hypertensive crisis. However, even a less dramatic rise may be equally significant if it heralds a dissecting aortic aneurysm, increased intracranial pressure, myocardial infarction, eclampsia, or thyrotoxicosis.
Usually associated with essential hypertension, elevated blood pressure may also result from a renal or endocrine disorder; a treatment that affects fluid status, such as dialysis; or a drug’s adverse effect. Ingestion of large amounts of certain foods, such as black licorice and cheddar cheese, may temporarily elevate blood pressure. (See Pathophysiology of Elevated Blood Pressure.)
Sometimes, elevated blood pressure may simply reflect inaccurate blood pressure measurement. (See Ensuring Accurate Blood Pressure Measurement , page 96.) However, careful measurement alone doesn’t ensure a clinically useful reading. To be useful, each blood pressure reading must be compared with the patient’s baseline. Also, serial readings may be necessary to establish elevated blood pressure.
Pathophysiology of Elevated Blood Pressure
Blood pressure — the force blood exerts on vessels as it flows through them — depends on cardiac output, peripheral resistance, and blood volume. A brief review of its regulating mechanisms — nervous system control, capillary fluid shifts, kidney excretion, and hormonal changes — will help you understand how elevated blood pressure develops.
Nervous system control involves the sympathetic system, chiefly baroreceptors and chemoreceptors, which promotes moderate vasoconstriction to maintain normal blood pressure. When this system responds inappropriately, increased vasoconstriction enhances peripheral resistance, resulting in elevated blood pressure.
Capillary fluid shifts regulate blood volume by responding to arterial pressure. Increased pressure forces fluid into the interstitial space; decreased pressure allows it to be drawn back into the arteries by osmosis. However, this fluid shift may take several hours to adjust blood pressure.
Kidney excretion also helps regulate blood volume by increasing or decreasing urine formation. Normally, an arterial pressure of about 60 mm Hg maintains urine output. When pressure drops below this reading, urine formation ceases, thereby increasing blood volume. Conversely, when arterial pressure exceeds this reading, urine formation increases, thereby reducing blood volume. Like capillary fluid shifts, this mechanism may take several hours to adjust blood pressure.
Hormonal changes reflect stimulation of the kidney’s renin-angiotensin-aldosterone system in response to low arterial pressure. This system affects vasoconstriction, which increases arterial pressure, and stimulates aldosterone release, which regulates sodium retention — a key determinant of blood volume.
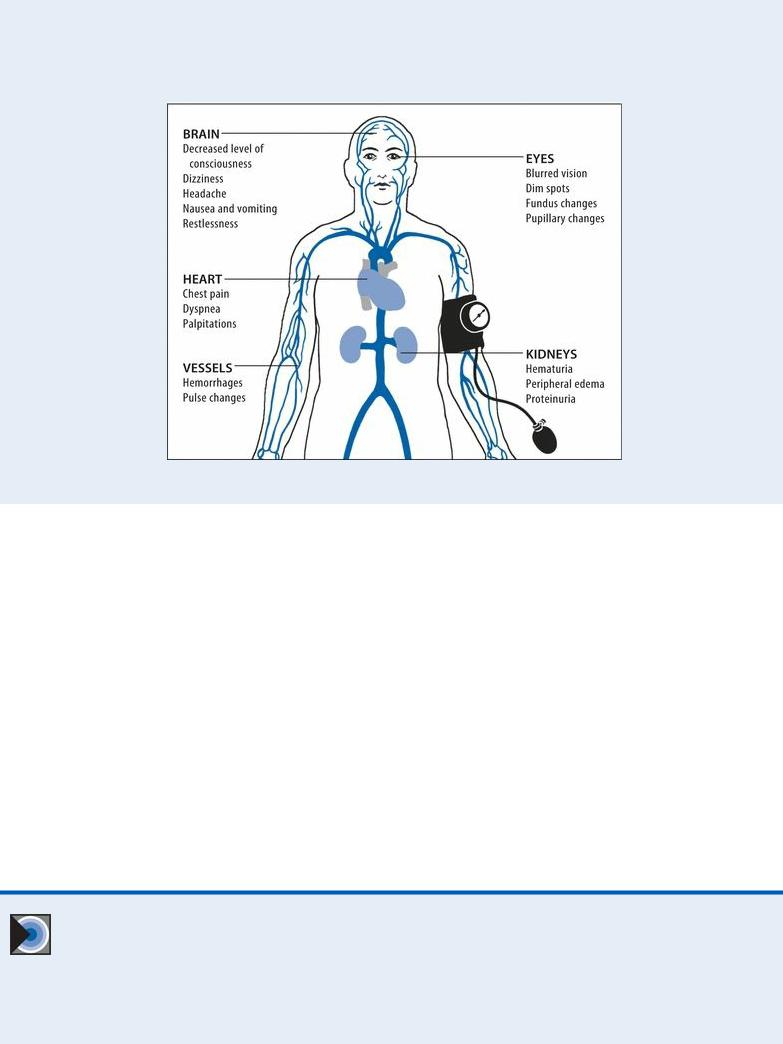
Elevated blood pressure signals the breakdown or inappropriate response of these pressureregulating mechanisms. Its associated signs and symptoms concentrate in the target organs and tissues illustrated below.
History and Physical Examination
If you detect sharply elevated blood pressure, quickly rule out possible life-threatening causes. (See
Managing Elevated Blood Pressure.)
After ruling out life-threatening causes, complete a more leisurely history and physical examination. Determine if the patient has a history of cardiovascular or cerebrovascular disease, diabetes, or renal disease. Ask about a family history of high blood pressure — a likely finding with essential hypertension, pheochromocytoma, or polycystic kidney disease. Then, ask about its onset. Did high blood pressure appear abruptly? Ask the patient’s age. The sudden onset of high blood pressure in middle-aged or elderly patients suggests renovascular stenosis. Although essential hypertension may begin in childhood, it typically isn’t diagnosed until near age 35. Pheochromocytoma and primary aldosteronism usually occur between ages 40 and 60. If you suspect either, check for orthostatic hypotension. Take the patient’s blood pressure with him lying down, sitting, and then standing. Normally, systolic pressure falls and diastolic pressure rises on standing. With orthostatic hypotension, both pressures fall.
EMERGENCY INTERVENTIONS Managing Elevated Blood
Pressure
Elevated blood pressure can signal various life-threatening disorders. However, if pressure
