
Borchers Andrea Ann (ed.) Handbook of Signs & Symptoms 2015
.pdf
Cerebellar hemorrhage. With cerebellar hemorrhage, a life-threatening disorder, ataxia is usually acute but transient. Unilateral or bilateral ataxia affects the trunk, gait, or limbs. The patient initially experiences repeated vomiting, occipital headache, vertigo, oculomotor palsy, dysphagia, and dysarthria. Later signs, such as a decreased LOC or coma, signal impending herniation.
Creutzfeldt-Jakob disease. Creutzfeldt-Jakob disease is a rapidly progressive dementia accompanied by neurologic signs and symptoms, such as myoclonic jerking, ataxia, aphasia, visual disturbances, and paralysis. It generally affects adults ages 40 to 65.
Diabetic neuropathy. Peripheral nerve damage due to diabetes mellitus may cause sensory ataxia, extremity pain, slight leg weakness, skin changes, and bowel and bladder dysfunction. Diphtheria. Within 4 to 8 weeks of the onset of symptoms, a life-threatening neuropathy can produce sensory ataxia. Diphtheria can be accompanied by fever, paresthesia, and paralysis of the limbs and, sometimes, the respiratory muscles.
Encephalomyelitis. Encephalomyelitis is a complication of measles, smallpox, chickenpox, or rubella, or of rabies or smallpox vaccination that may damage cerebrospinal white matter. Rarely, it’s accompanied by cerebellar ataxia. Other signs and symptoms include headache, fever, vomiting, an altered LOC, paralysis, seizures, oculomotor palsy, and pupillary changes.
Friedreich’s ataxia. A progressive familial disorder, Friedreich’s ataxia affects the spinal cord and cerebellum. It causes gait ataxia, followed by truncal, limb, and speech ataxia. Other signs and symptoms include pes cavus, kyphoscoliosis, cranial nerve palsy, and motor and sensory deficits. A positive Babinski’s reflex may appear.
Guillain-Barré syndrome. Peripheral nerve involvement usually follows a mild viral infection, rarely leading to sensory ataxia. Guillain-Barré syndrome also causes ascending paralysis and possibly respiratory distress.
Hepatocerebral degeneration. Patients who survive hepatic coma are occasionally left with residual neurologic defects, including mild cerebellar ataxia with a wide-based, unsteady gait. Ataxia may be accompanied by an altered LOC, dysarthria, rhythmic arm tremors, and choreoathetosis of the face, neck, and shoulders.
Multiple sclerosis (MS). Nystagmus and cerebellar ataxia commonly occur in MS, but they aren’t always accompanied by limb weakness and spasticity. Speech ataxia (especially scanning) may occur as well as sensory ataxia from spinal cord involvement. During remissions, ataxia may subside or may even disappear. During exacerbations, it may reappear, worsen, or even become permanent. MS also causes optic neuritis, optic atrophy, numbness and weakness, diplopia, dizziness, and bladder dysfunction.
Olivopontocerebellar atrophy. Olivopontocerebellar atrophy produces gait ataxia and, later, limb and speech ataxia. Rarely, it produces an intention tremor. It’s accompanied by choreiform movements, dysphagia, and loss of sphincter tone.
Poisoning. Chronic arsenic poisoning may cause sensory ataxia, along with headache, seizures, an altered LOC, motor deficits, and muscle aching. Chronic mercury poisoning causes gait and limb ataxia, principally of the arms. It also causes tremors of the extremities, tongue, and lips, mental confusion, mood changes, and dysarthria.
Polyneuropathy. Carcinomatous and myelomatous polyneuropathy may occur before detection of the primary tumor in cancer, multiple myeloma, or Hodgkin’s disease. Signs and symptoms include ataxia, severe motor weakness, muscle atrophy, and sensory loss in the limbs. Pain and

skin changes may also occur.
Porphyria. Porphyria affects the sensory and, more frequently, the motor nerves, possibly leading to ataxia. It also causes abdominal pain, mental disturbances, vomiting, headache, focal neurologic defects, an altered LOC, generalized seizures, and skin lesions.
Posterior fossa tumor. Gait, truncal, or limb ataxia is an early sign and may worsen as the tumor enlarges. It’s accompanied by vomiting, headache, papilledema, vertigo, oculomotor palsy, a decreased LOC, and motor and sensory impairments on the same side as the lesion.
Spinocerebellar ataxia. With spinocerebellar ataxia, the patient may initially experience fatigue, followed by stiff-legged gait ataxia. Eventually, limb ataxia, dysarthria, static tremor, nystagmus, cramps, paresthesia, and sensory deficits occur.
Stroke. In stroke, occlusions in the vertebrobasilar arteries halt blood flow to cause infarction in the medulla, pons, or cerebellum that may lead to ataxia. Ataxia may occur at the onset of stroke and remain as a residual deficit. Worsening ataxia during the acute phase may indicate extension of the stroke or severe swelling. Ataxia may be accompanied by unilateral or bilateral motor weakness, a possible altered LOC, sensory loss, vertigo, nausea, vomiting, oculomotor palsy, and dysphagia.
Wernicke’s disease. The result of thiamine deficiency, Wernicke’s disease produces gait ataxia and, rarely, intention tremor or speech ataxia. With severe ataxia, the patient may be unable to stand or walk. Ataxia decreases with thiamine therapy. Associated signs and symptoms include nystagmus, diplopia, ocular palsies, confusion, tachycardia, exertional dyspnea, and orthostatic hypotension.
Other Causes
Drugs. Toxic levels of anticonvulsants, especially phenytoin, may result in gait ataxia. Toxic levels of anticholinergics and tricyclic antidepressants may also result in ataxia. Aminoglutethimide causes ataxia in about 10% of patients; however, this effect usually disappears 4 to 6 weeks after drug therapy is discontinued.
Special Considerations
Prepare the patient for laboratory studies, such as blood tests for toxic drug levels and radiologic tests. Then, focus on helping the patient adapt to his condition. Promote rehabilitation goals, and help ensure the patient’s safety. For example, instruct the patient with sensory ataxia to move slowly, especially when turning or getting up from a chair. Provide a cane or walker for extra support. Ask the patient’s family to check his home for hazards, such as uneven surfaces or the absence of handrails on stairs. If appropriate, refer the patient with progressive disease for counseling.
Patient Counseling
Help the patient to identify rehabilitation goals, stress safety measures, and discuss the use of assistive devices. Refer the patient to counseling as needed.
Pediatric Pointers
In children, ataxia occurs in acute and chronic forms and results from congenital or acquired disease.
Acute ataxia may stem from febrile infection, brain tumors, mumps, and other disorders. Chronic ataxia may stem from Gaucher’s disease, Refsum’s disease, and other inborn errors of metabolism.
When assessing a child for ataxia, consider his level of motor skills and emotional state. Your examination may be limited to observing the child in spontaneous activity and carefully questioning his parents about changes in his motor activity, such as increased unsteadiness or falling. If you suspect ataxia, refer the child for a neurologic evaluation to rule out a brain tumor.
REFERENCES
Williams, G., Schache, A., & McCulloch, K. (2010). Evaluation of a conceptual framework for retraining high-level mobility following traumatic brain injury: Two case reports. Journal of Head Trauma Rehabilitation, 25(3), 164–172.
Zahr, N. M., Kaufman, K. L., & Harper, C. G. (2011) . Clinical and pathological features of alcohol-related brain damage. National Review of Neurology, 7, 284–294.
Aura
An aura is a sensory or motor phenomenon, idea, or emotion that marks the initial stage of a seizure or the approach of a classic migraine headache. Auras may be classified as cognitive, affective, psychosensory, or psychomotor. (See Recognizing Types of Auras.)
When associated with a seizure, an aura stems from an irritable focus in the brain that spreads throughout the cortex. Although an aura was once considered a sign of impending seizure, it’s now considered the first stage of a seizure. Typically, it occurs seconds to minutes before the ictal phase. Its intensity, duration, and type depend on the origin of the irritable focus. For example, an aura of bitter taste commonly accompanies a frontal lobe lesion. Unfortunately, an aura is difficult to describe because the postictal phase of a seizure temporarily alters the patient’s level of consciousness, impairing his memory of the event.
The aura associated with a classic migraine headache results from cranial vasoconstriction. Diagnostically important, it helps distinguish a classic migraine from other types of headaches.
Typically, an aura develops over 10 to 30 minutes and varies in intensity and duration. If the patient recognizes the aura as a warning sign, he may be able to prevent the headache by taking appropriate drugs.
 EMERGENCY INTERVENTIONS
EMERGENCY INTERVENTIONS
When an aura rapidly progresses to the ictal phase of a seizure, quickly evaluate the seizure and be alert for life-threatening complications such as apnea. When an aura heralds a classic migraine, make the patient as comfortable as possible. Place him in a dark, quiet room, and administer drugs to prevent the headache, if necessary.
History and Physical Examination
Obtain a thorough history of the patient’s headaches or seizure history, asking him to describe any sensory or motor phenomena that precede each headache or seizure. Find out how long each headache or seizure typically lasts. Does anything make it worse, such as bright lights, noise, or caffeine? Does anything make it better? Ask the patient about drugs he takes for pain relief.
Recognizing Types of Auras
Determining whether an aura marks the patient’s thought processes, emotions, or sensory or motor function usually requires keen observation. An aura is typically difficult to describe and is only dimly remembered when associated with seizure activity. Below, you’ll find the types of auras the patient may experience.
AFFECTIVE AURAS
Fear
Paranoia
Other emotions
COGNITIVE AURAS
Déjà vu (familiarity with unfamiliar events or environments)
Flashback of past events
Jamais vu (unfamiliarity with a known event)
Time standing still
PSYCHOMOTOR AURAS
Automatisms (inappropriate, repetitive movements): lip smacking, chewing, swallowing, grimacing, picking at clothes, climbing stairs
PSYCHOSENSORY AURAS
Auditory: buzzing or ringing in the ears
Gustatory: acidic, metallic, or bitter tastes
Olfactory: foul odors
Tactile: numbness or tingling
Vertigo
Visual: flashes of light (scintillations)
Medical Causes
Classic migraine headache. A migraine is preceded by a vague premonition and then, usually, a visual aura involving flashes of light. The aura lasts 10 to 30 minutes and may intensify until it completely obscures the patient’s vision. A classic migraine may cause numbness or tingling of the lips, face, or hands, slight confusion, and dizziness before the characteristic unilateral, throbbing headache appears. It slowly intensifies; when it peaks, it may cause photophobia, nausea, and vomiting.
Seizure, generalized tonic-clonic. A generalized tonic-clonic seizure may begin with or
without an aura. The patient loses consciousness and falls to the ground. His body stiffens (tonic phase), and then he experiences rapid, synchronous muscle jerking and hyperventilation (clonic phase). The seizure usually lasts 2 to 5 minutes.
Special Considerations
Advise the patient to keep a diary of factors that precipitate each headache as well as associated symptoms to help you evaluate the effectiveness of drug therapy, and recommend lifestyle changes. Stress reduction measures usually play a role here.
Patient Counseling
Teach the patient stress reduction measures. If the patient recognizes the aura as a warning sign, tell him to prevent the headache by taking the appropriate medications. Explain the underlying disorder and any diagnostic tests or procedures. If the patient has a seizure disorder, emphasize the importance of taking anticonvulsants as directed. Stress the importance of regular follow-up appointments for blood studies.
Pediatric Pointers
Watch for nonverbal clues possibly associated with aura, such as rubbing the eyes, coughing, and spitting. When taking the seizure history, recognize that children — like adults — tend to forget the aura. Ask simple, direct questions, such as “Do you see anything funny before the seizure?” and “Do you get a bad taste in your mouth?” Give the child ample time to respond because he may have difficulty describing the aura.
REFERENCES
Hellier, S. (2013). Hormonal contraception and headaches: What are the prescriber’s options? The Nurse Practitioner: The American Journal of Primary Health Care, 38(12), 32–37.
Pestka, E. & Nash, V. (2012). Decoding genetics: Genetic aspects of migraine headaches. Nursing 2014 Critical Care, 7(2), 16–18.

B
Babinski’s Reflex
[Extensor plantar reflex]
Babinski’s reflex — dorsiflexion of the great toe with extension and fanning of the other toes — is an abnormal reflex elicited by firmly stroking the lateral aspect of the sole of the foot with a moderately sharp object. (See How to Elicit Babinski’s Reflex , page 80.) In some patients, this reflex can be triggered by noxious stimuli, such as pain, noise, or even bumping the bed. An indicator of corticospinal damage, Babinski’s reflex may occur unilaterally or bilaterally and may be temporary or permanent. A temporary Babinski’s reflex commonly occurs during the postictal phase of a seizure, whereas a permanent Babinski’s reflex occurs with corticospinal damage. A positive Babinski’s reflex is normal in neonates and in infants up to 24 months old.
History and Physical Examination
After eliciting a positive Babinski’s reflex, evaluate the patient for other neurologic signs. Evaluate muscle strength in each extremity by having the patient push or pull against your resistance. Passively flex and extend the extremity to assess muscle tone. Intermittent resistance to flexion and extension indicates spasticity, and a lack of resistance indicates flaccidity.
Next, check for evidence of incoordination by asking the patient to perform a repetitive activity. Test deep tendon reflexes (DTRs) in the patient’s elbow, antecubital area, wrist, knee, and ankle by striking the tendon with a reflex hammer. An exaggerated muscle response indicates hyperactive DTRs; little or no muscle response indicates hypoactivity.
Then, evaluate pain sensation and proprioception in the feet. As you move the patient’s toes up and down, ask the patient to identify the direction in which the toes have been moved without looking at his feet.
Medical Causes
Amyotrophic lateral sclerosis (ALS). With this progressive motor neuron disorder, bilateral Babinski’s reflex may occur with hyperactive DTRs and spasticity. Typically, ALS produces fasciculations accompanied by muscle atrophy and weakness. Incoordination makes carrying out activities of daily living difficult for the patient. Associated signs and symptoms include impaired speech; difficulty chewing, swallowing, and breathing; urinary frequency and urgency; and, occasionally, choking and excessive drooling. Although his mental status remains intact, the patient’s poor prognosis may cause periodic depression. Progressive bulbar palsy involves the brain stem and may cause episodes of crying or inappropriate laughter.
Brain tumor. A brain tumor that involves the corticospinal tract may produce Babinski’s reflex. The reflex may be accompanied by hyperactive DTRs (unilateral or bilateral), spasticity,
seizures, cranial nerve dysfunction, hemiparesis or hemiplegia, decreased pain sensation, an unsteady gait, incoordination, headache, emotional lability, and a decreased level of consciousness (LOC).
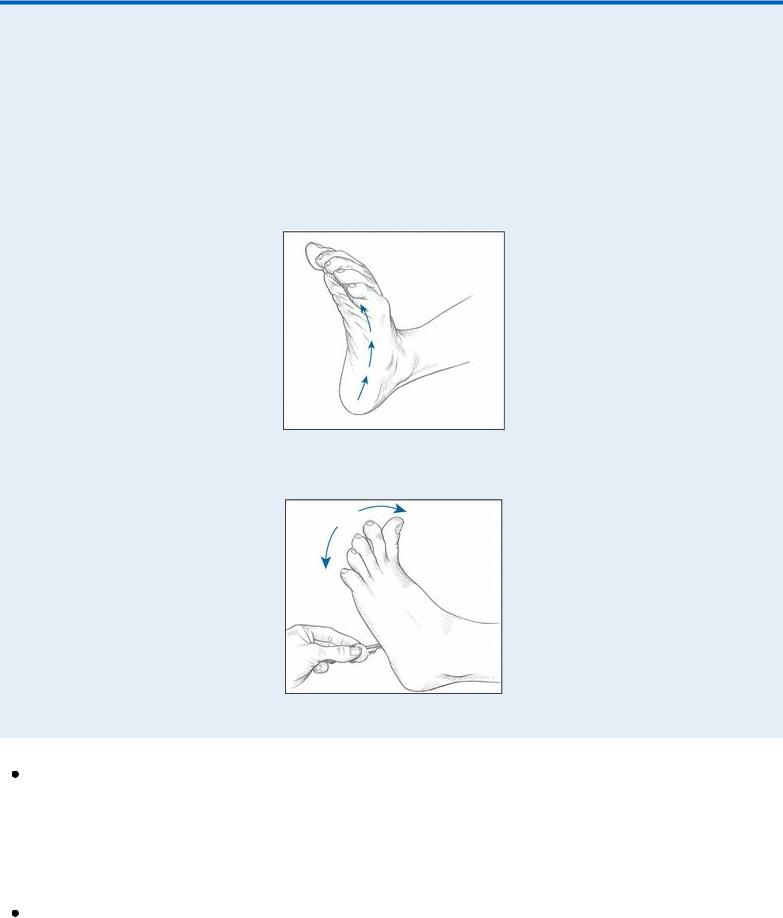
 EXAMINATION TIP How to Elicit Babinski’s Reflex
EXAMINATION TIP How to Elicit Babinski’s Reflex
To elicit Babinski’s reflex, stroke the lateral aspect of the sole of the patient’s foot with your thumbnail or another moderately sharp object. Normally, this elicits flexion of all toes (a negative Babinski’s reflex), as shown below in the left illustration. With a positive Babinski’s reflex, the great toe dorsiflexes and the other toes fan out, as shown in the right illustration.
NORMAL TOE FLEXION
POSITIVE BABINSKI’S REFLEX
Head trauma. Unilateral or bilateral Babinski’s reflex may occur as the result of primary corticospinal damage or secondary injury associated with increased intracranial pressure. Hyperactive DTRs and spasticity commonly occur with Babinski’s reflex. The patient may also have weakness and incoordination. Other signs and symptoms vary with the type of head trauma and include headache, vomiting, behavior changes, altered vital signs, and decreased LOC with abnormal pupillary size and response to light.
Hepatic encephalopathy. Babinski’s reflex occurs late in hepatic encephalopathy when the patient slips into a coma. It’s accompanied by hyperactive DTRs and fetor hepaticus.

Meningitis. With meningitis, bilateral Babinski’s reflex commonly follows fever, chills, and malaise and is accompanied by nausea and vomiting. As meningitis progresses, it also causes decreased LOC, nuchal rigidity, positive Brudzinski’s and Kernig’s signs, hyperactive DTRs, and opisthotonos. Associated signs and symptoms include irritability, photophobia, diplopia, delirium, and deep stupor that may progress to coma.
Rabies. Bilateral Babinski’s reflex — possibly elicited by nonspecific noxious stimuli alone — appears in the excitation phase of rabies. This phase occurs 2 to 10 days after the onset of prodromal signs and symptoms, such as fever, malaise, and irritability (which occur 30 to 40 days after a bite from an infected animal). Rabies is characterized by marked restlessness and extremely painful pharyngeal muscle spasms. Difficulty swallowing causes excessive drooling and hydrophobia in about 50% of affected patients. Seizures and hyperactive DTRs may also occur.
Spinal cord injury. With acute injury, spinal shock temporarily erases all reflexes. As shock resolves, Babinski’s reflex occurs — unilaterally when injury affects only one side of the spinal cord (Brown-Séquard syndrome) and bilaterally when injury affects both sides. Rather than signaling the return of neurologic function, this reflex confirms corticospinal damage. It’s accompanied by hyperactive DTRs, spasticity, and variable or total loss of pain and temperature sensation, proprioception, and motor function. Horner’s syndrome, marked by unilateral ptosis, pupillary constriction, and facial anhidrosis, may occur with lower cervical cord injury.
Spinal cord tumor. With spinal cord tumor, bilateral Babinski’s reflex occurs with variable loss of pain and temperature sensation, proprioception, and motor function. Spasticity, hyperactive DTRs, absent abdominal reflexes, and incontinence are also characteristic. Diffuse pain may occur at the level of the tumor.
Spinal paralytic poliomyelitis. Unilateral or bilateral Babinski’s reflex occurs 5 to 7 days after the onset of fever. It’s accompanied by progressive weakness, paresthesia, muscle tenderness, spasticity, irritability and, later, atrophy. Resistance to neck flexion is characteristic, as are Hoyne’s, Kernig’s, and Brudzinski’s signs.
Spinal tuberculosis. Spinal tuberculosis may produce bilateral Babinski’s reflex accompanied by variable loss of pain and temperature sensation, proprioception, and motor function. It also causes spasticity, hyperactive DTRs, bladder incontinence, and absent abdominal reflexes.
Stroke. Babinski’s reflex varies with the site of the stroke. If it involves the cerebrum, it produces unilateral Babinski’s reflex accompanied by hemiplegia or hemiparesis, unilateral hyperactive DTRs, hemianopsia, and aphasia. If it involves the brain stem, it produces bilateral Babinski’s reflex accompanied by bilateral weakness or paralysis, bilateral hyperactive DTRs, cranial nerve dysfunction, incoordination, and an unsteady gait. Generalized signs and symptoms of stroke include headache, vomiting, fever, disorientation, nuchal rigidity, seizures, and coma.
Syringomyelia. With syringomyelia, bilateral Babinski’s reflex occurs with muscle atrophy and weakness that may progress to paralysis. It’s accompanied by spasticity, ataxia and, occasionally, deep pain. DTRs may be hypoactive or hyperactive. Cranial nerve dysfunction, such as dysphagia and dysarthria, commonly appears late in the disorder.
Special Considerations
Babinski’s reflex usually occurs with incoordination, weakness, and spasticity, all of which increase the patient’s risk of injury. To prevent injury, assist the patient with activity and keep his environment
free from obstructions.
Diagnostic tests may include a computed tomography scan or magnetic resonance imaging of the brain or spine, angiography or myelography and, possibly, a lumbar puncture to clarify or confirm the cause of Babinski’s reflex. Prepare the patient as necessary.
Patient Counseling
Caution the patient about the need to call for assistance when getting out of bed and discuss ways to maintain a safe environment. Instruct the patient in the use of adaptive devices.
Pediatric Pointers
Babinski’s reflex occurs normally in infants ages 18 to 24 months, reflecting immaturity of the corticospinal tract. After age 2, Babinski’s reflex is pathologic and may result from hydrocephalus or any of the causes more commonly seen in adults.
REFERENCES
Caranci, F., Briganti, F., Cirillo, L., Leonardi, M., & Muto, M. (2013). Epidemiology and genetics of intracranial aneurysms. European Journal of Radiology, 82, 1598–1605.
Hetts, S. W. , English, J. D., Dowd, C. F., Higashida, R. T., Scanlon, J. T., & Halbach, V. V. (2011). Pediatric intracranial aneurysms: New and enlarging aneurysms after index aneurysm treatment or observation. American Journal of Neuroradiology , 32, 2017–2022.
Back Pain
Back pain affects an estimated 80% of the population; in fact, it’s the second leading reason — after the common cold — for lost time from work. Although this symptom may herald a spondylogenic disorder, it may also result from a genitourinary, GI, cardiovascular, or neoplastic disorder. Postural imbalance associated with pregnancy may also cause back pain.
The onset, location, and distribution of pain and its response to activity and rest provide important clues about the cause. Pain may be acute or chronic, constant or intermittent. It may remain localized in the back, radiate along the spine or down one or both legs, or be widespread. Pain may be exacerbated by activity — usually bending, stooping, lifting, or exercising — and alleviated by rest, or it may be unaffected by either.
Intrinsic back pain results from muscle spasm, nerve root irritation, fracture, or a combination of these mechanisms. It usually occurs in the lower back, or lumbosacral area. Back pain may also be referred from the abdomen or flank, possibly signaling a life-threatening perforated ulcer, acute pancreatitis, or a dissecting abdominal aortic aneurysm.
 EMERGENCY INTERVENTIONS
EMERGENCY INTERVENTIONS
If the patient reports acute, severe back pain, quickly take his vital signs and then perform a rapid evaluation to rule out life-threatening causes. Ask him when the pain began. Can he relate it to any causes? For example, did the pain occur after eating? After falling on the ice? Have the patient describe the pain. Is it burning, stabbing, throbbing, or aching? Is it constant or intermittent? Does it radiate to the buttocks, legs, or toes? Does he have leg
weakness or footdrop? Does the pain seem to originate in the abdomen and radiate to the back? Has he had a pain like this before? What makes it better or worse? Is it affected by activity or rest? Is it worse in the morning or evening? Does it wake him up? Typically, visceral-referred back pain is unaffected by activity and rest. In contrast, spondylogenicreferred back pain worsens with activity and improves with rest. Pain of neoplastic origin is usually relieved by walking and worsens at night.
If the patient describes deep lumbar pain unaffected by activity, palpate for a pulsating epigastric mass. If this sign is present, suspect a dissecting abdominal aortic aneurysm. Withhold food and fluid in anticipation of emergency surgery. Prepare for I.V. fluid replacement and oxygen administration. Monitor the patient’s vital signs and peripheral pulses closely.
If the patient describes severe epigastric pain that radiates through the abdomen to the back, assess him for absent bowel sounds and for abdominal rigidity and tenderness. If these occur, suspect a perforated ulcer or acute pancreatitis. Start an I.V. for fluids and drugs, administer oxygen, and insert a nasogastric tube while withholding food.
History and Physical Examination
If life-threatening causes of back pain are ruled out, continue with a complete history and physical examination. Be aware of the patient’s expressions of pain as you do so. Obtain a medical history, including past injuries and illnesses, and a family history. Ask about diet and alcohol intake. Also, take a drug history, including past and present prescriptions and over-the-counter drugs.
Next, perform a thorough physical examination. Observe skin color, especially in the patient’s legs, and palpate skin temperature. Palpate femoral, popliteal, posterior tibial, and pedal pulses. Ask about unusual sensations in the legs, such as numbness and tingling. Observe the patient’s posture if pain doesn’t prohibit standing. Does he stand erect or tend to lean toward one side? Observe the level of the shoulders and pelvis and the curvature of the back. Ask the patient to bend forward, backward, and from side to side while you palpate for paravertebral muscle spasms. Note rotation of the spine on the trunk. Palpate the dorsolumbar spine for point tenderness. Then, ask the patient to walk — first on his heels and then on his toes — protect him from falling as he does so. Weakness may reflect a muscular disorder or spinal nerve root irritation. Place the patient in a sitting position to evaluate and compare patellar tendon (knee), Achilles tendon, and Babinski’s reflexes. Evaluate the strength of the extensor hallucis longus by asking the patient to hold up his big toe against resistance. Measure leg length and hamstring and quadriceps muscles bilaterally. Note a difference of more than ⅜" (1 cm) in muscle size, especially in the calf.
To reproduce leg and back pain, position the patient in a supine position on the examining table. Grasp his heel and slowly lift his leg. If he feels pain, note its exact location and the angle between the table and his leg when it occurs. Repeat this maneuver with the opposite leg. Pain along the sciatic nerve may indicate disk herniation or sciatica. Also, note the range of motion of the hip and knee.
Palpate the flanks and percuss with the fingertips or perform fist percussion to elicit costovertebral angle tenderness.
Medical Causes
