
Borchers Andrea Ann (ed.) Handbook of Signs & Symptoms 2015
.pdf
palpating or stroking the skin produces a crackling sound called subcutaneous crepitation or subcutaneous emphysema. The bubbles feel like small, unstable nodules and aren’t painful, even though subcutaneous crepitation is commonly associated with painful disorders. Usually, the affected tissue is visibly edematous; this can lead to life-threatening airway occlusion if the edema affects the neck or upper chest.
The air or gas bubbles enter the tissues through open wounds from the action of anaerobic microorganisms or from traumatic or spontaneous rupture or perforation of pulmonary or GI organs.
History and Physical Examination
Because subcutaneous crepitation can indicate a life-threatening disorder, you’ll need to perform a rapid initial evaluation and intervene if necessary. (See Managing Subcutaneous Crepitation.)
When the patient’s condition permits, palpate the affected skin to evaluate the location and extent of subcutaneous crepitation and to obtain baseline information. Delineate the borders of the area of crepitus with a marker. Palpate the area frequently to determine if the subcutaneous crepitation is increasing. Ask the patient if he’s experiencing pain or having difficulty breathing. If he’s in pain, find out where the pain is located, how severe it is, and when it began. Ask about recent thoracic surgery, diagnostic tests, and respiratory therapy or a history of trauma or chronic pulmonary disease.
EMERGENCY INTERVENTIONS Managing Subcutaneous
Crepitation
Subcutaneous crepitation occurs when air or gas bubbles escape into tissues. It may signal life-threatening rupture of an air-filled or gas-producing organ or a fulminating anaerobic infection.
ORGAN RUPTURE
If the patient shows signs of respiratory distress — such as severe dyspnea, tachypnea, accessory muscle use, nasal flaring, air hunger, or tachycardia — quickly test for Hamman’s sign to detect trapped air bubbles in the mediastinum.
To test for Hamman’s sign, help the patient assume a left-lateral recumbent position. Then, place your stethoscope over the precordium. If you hear a loud crunching sound that synchronizes with his heartbeat, the patient has a positive Hamman’s sign.
Depending on which organ is ruptured, be prepared for endotracheal intubation, an emergency tracheotomy, or chest tube insertion. Start administering supplemental oxygen immediately. Start an I.V. to administer fluids and medication, and connect the patient to a cardiac monitor.
ANAEROBIC INFECTION
If the patient has an open wound with a foul odor and local swelling and discoloration, you must act quickly. Take the patient’s vital signs, checking especially for fever, tachycardia, hypotension, and tachypnea. Next, start an I.V. line to administer fluids and medication, and
provide supplemental oxygen.
In addition, be prepared for emergency surgery to drain and debride the wound. If the patient’s condition is life threatening, you may need to prepare him for transfer to a facility with a hyperbaric chamber.
Medical Causes
Gas gangrene. Subcutaneous crepitation is the hallmark of gas gangrene, a rare but commonly fatal infection that’s caused by anaerobic microorganisms. It’s accompanied by local pain, swelling, and discoloration, with the formation of bullae and necrosis. The skin over the wound may rupture, revealing dark red or black necrotic muscle and producing foul-smelling, watery, or frothy discharge. Related findings include tachycardia, tachypnea, a moderate fever, cyanosis, and lassitude.
Orbital fracture. An orbital fracture allows air from the nasal sinuses to escape into subcutaneous tissue, causing subcutaneous crepitation of the eyelid and orbit. The most common sign of this fracture is periorbital ecchymosis. Visual acuity is usually normal, although a swollen lid may prevent accurate testing. The patient has facial edema, diplopia, a hyphema, and, occasionally, a dilated or unreactive pupil on the affected side. Extraocular movements may also be affected.
Pneumothorax. Severe pneumothorax produces subcutaneous crepitation in the upper chest and neck. In many cases, the patient has chest pain that’s unilateral, rarely localized initially, and increased on inspiration. Dyspnea, anxiety, restlessness, tachypnea, cyanosis, tachycardia, accessory muscle use, asymmetrical chest expansion, and a nonproductive cough can also occur. On the affected side, breath sounds are absent or decreased, hyperresonance or tympany may be heard, and decreased vocal fremitus may be present.
Rupture of the esophagus. A ruptured esophagus usually produces subcutaneous crepitation in the neck, chest wall, or supraclavicular fossa, although this sign doesn’t always occur. With a rupture of the cervical esophagus, the patient has excruciating pain in the neck or supraclavicular area, his neck is resistant to passive motion, and he has local tenderness, soft tissue swelling, dysphagia, odynophagia, and orthostatic vertigo.
Life-threatening rupture of the intrathoracic esophagus can produce mediastinal emphysema confirmed by a positive Hamman’s sign. The patient has severe retrosternal, epigastric, neck, or scapular pain, and edema of the chest wall and neck. He may also display dyspnea, tachypnea, asymmetrical chest expansion, nasal flaring, cyanosis, diaphoresis, tachycardia, hypotension, dysphagia, and a fever.
Rupture of the trachea or major bronchus. Rupture of the trachea or major bronchus is a lifethreatening injury that produces abrupt subcutaneous crepitation of the neck and anterior chest wall. The patient has severe dyspnea with nasal flaring, tachycardia, accessory muscle use, hypotension, cyanosis, extreme anxiety, and, possibly, hemoptysis and mediastinal emphysema, with a positive Hamman’s sign.
Other Causes
Diagnostic tests. Endoscopic tests, such as bronchoscopy and upper GI tract endoscopy, can

cause rupture or perforation of respiratory or GI organs, producing subcutaneous crepitation. Respiratory treatments. Mechanical ventilation and intermittent positive-pressure breathing can rupture alveoli, producing subcutaneous crepitation.
Thoracic surgery. If air escapes into the tissue in the area of the incision, subcutaneous crepitation can occur.
Special Considerations
Monitor the patient’s vital signs frequently, especially respirations. Because excessive edema from subcutaneous crepitation in the neck and upper chest can cause airway obstruction, be alert for signs of respiratory distress such as dyspnea. Tell the patient that the affected tissues will eventually absorb the air or gas bubbles and the subcutaneous crepitation will decrease.
Patient Counseling
Explain diagnostic tests and procedures the patient needs and the signs and symptoms of subcutaneous crepitation to report.
Pediatric Pointers
Children may develop subcutaneous crepitation in the neck from ingestion of corrosive substances that perforate the esophagus.
REFERENCES
Rezende-Neto, J. B., Hoffmann, J. , Al Mahroos, M. , Tien, H. , Hsee, L. C., Spencer Netto, F., … Rizoli, S. B. (2010) . Occult pneumomediastinum in blunt chest trauma: Clinical significance. Injury, 41(1), 40–43.
Zhao, D. Y. , Zhang, G. L. (2009) . Clinical analysis on 38 cases of pneumothorax induced by acupuncture or acupoint injection.
Zhongguo Zhen Jiu, 29(3), 239–242.
Cry, High-Pitched[Cerebral cry]
A high-pitched cry is a brief, sharp, piercing vocal sound produced by a neonate or infant. Whether acute or chronic, this cry is a late sign of increased intracranial pressure (ICP). The acute onset of a high-pitched cry demands emergency treatment to prevent permanent brain damage or death.
A change in the volume of one of the brain’s components — brain tissue, cerebrospinal fluid, and blood — may cause increased ICP. In neonates, increased ICP may result from intracranial bleeding associated with birth trauma or from congenital malformations, such as craniostenosis and ArnoldChiari deformity. In fact, a high-pitched cry may be an early sign of a congenital malformation. In infants, increased ICP may result from meningitis, head trauma, or child abuse.
History and Physical Examination
Take the infant’s vital signs, and then obtain a brief history. Did the infant fall recently or experience even minor head trauma? Make sure to ask the mother about changes in the infant’s behavior during the past 24 hours. Has he been vomiting? Has he seemed restless or unlike himself? Has his sucking reflex diminished? Does he cry when he’s moved? Suspect child abuse if the infant’s history is inconsistent with physical findings.

Next, perform a neurologic examination. Remember that neurologic responses in a neonate or young infant are primarily reflex responses. Determine the infant’s level of consciousness (LOC). Is he awake, irritable, or lethargic? Does he reach for an attractive object or turn toward the sound of a rattle? Observe his posture. Is he in the normal flexed position or in extension or opisthotonos? Examine muscle tone and observe the infant for signs of seizure, such as tremors and twitching.
Examine the size and shape of the infant’s head. Is the anterior fontanel bulging? Measure the infant’s head circumference, and check pupillary size and response to light. Unilateral or bilateral dilation and a sluggish response to light may accompany increased ICP. Finally, test the infant’s reflexes; expect Moro’s reflex to be diminished.
After completing your examination, elevate the infant’s head to promote cerebral venous drainage and decrease ICP. Start an I.V. line, and give a diuretic and a corticosteroid to decrease ICP. Be sure to keep endotracheal (ET) intubation equipment close by to secure an airway.
Medical Causes
Increased ICP. A high-pitched cry is a late sign of increased ICP. Typically, the infant also displays bulging fontanels, increased head circumference, and widened sutures. Earlier signs and symptoms of increasing ICP include seizures, bradycardia, possible vomiting, dilated pupils, decreased LOC, increased systolic blood pressure, a widened pulse pressure, and an altered respiratory pattern.
Special Considerations
The infant with increased ICP requires specialized care and monitoring in the intensive care unit. For example, you’ll need to monitor his vital signs and neurologic status to detect subtle changes in his condition. Also, monitor his intake and output. Monitor ICP, restrict fluids, and administer a diuretic. Increase the head of the bed 30 degrees, if the condition permits, and keep the head midline. Perform nursing care judiciously because procedures may cause a further increase in ICP. For an infant with severely increased ICP, ET intubation and mechanical hyperventilation may be needed to decrease serum carbon dioxide levels and constrict cerebral blood vessels. Hyperventilation is used for acute increases in ICP, the risks and benefits of which must be carefully weighed. Alternatively, barbiturate coma or hypothermia therapy may be needed to decrease the infant’s metabolic rate.
Remember to avoid jostling the infant, which may aggravate increased ICP. Comfort him and maintain a calm, quiet environment because the infant’s crying or exposure to environmental stimuli may also worsen increased ICP.
Patient Counseling
Explain the infant’s diagnosis and treatment plan to the parents. Orient the parents to the intensive care unit and show them how to comfort the infant and maintain a calm environment to avoid increasing ICP.
REFERENCES
Tiskumara, R., Fakharee, S. H., Liu, C-Q., Nuntnarumit, P., Lui, K-M., Hammoud, M., Nuntnarumit, P., Lui, K. M., Hammoud, M., … Isaacs, D.; Asia-Pacific Neonatal Infections Study. (2009). Neonatal infections in Asia. Archives of Disease in Child Fetal and Neonatal Education, 94, 144–148.
Zaidi, A. K., Thaver, D., Ali, S. A., & Khan, T. A. (2009). Pathogens associated with sepsis in newborns and young infants in developing countries. Pediatric Infectious Disease Journal, 28, S10–S18.
Cyanosis
Cyanosis — a bluish or bluish black discoloration of the skin and mucous membranes — results from excessive concentration of unoxygenated hemoglobin in the blood. This common sign may develop abruptly or gradually. It can be classified as central or peripheral, although the two types may coexist.
Central cyanosis reflects inadequate oxygenation of systemic arterial blood caused by right-to- left cardiac shunting, pulmonary disease, or hematologic disorders. It may occur anywhere on the skin and also on the mucous membranes of the mouth, lips, and conjunctiva.
Peripheral cyanosis reflects sluggish peripheral circulation caused by vasoconstriction, reduced cardiac output, or vascular occlusion. It may be widespread or may occur locally in one extremity; however, it doesn’t affect mucous membranes. Typically, peripheral cyanosis appears on exposed areas, such as the fingers, nail beds, feet, nose, and ears.
Although cyanosis is an important sign of cardiovascular and pulmonary disorders, it isn’t always an accurate gauge of oxygenation. Several factors contribute to its development: hemoglobin concentration and oxygen saturation, cardiac output, and partial pressure of arterial oxygen (PaO2). Cyanosis is usually undetectable until the oxygen saturation of hemoglobin falls below 80%. Severe cyanosis is quite obvious, whereas mild cyanosis is more difficult to detect, even in natural, bright light. In dark-skinned patients, cyanosis is most apparent in the mucous membranes and nail beds.
Transient, nonpathologic cyanosis may result from environmental factors. For example, peripheral cyanosis may result from cutaneous vasoconstriction following a brief exposure to cold air or water. Central cyanosis may result from reduced PaO2 at high altitudes.
 EMERGENCY INTERVENTIONS
EMERGENCY INTERVENTIONS
If the patient displays sudden, localized cyanosis and other signs of arterial occlusion, place the affected limb in a dependent position and protect it from injury; however, don’t massage the limb. If you see central cyanosis stemming from a pulmonary disorder or shock, perform a rapid evaluation. Take immediate steps to maintain an airway, assist breathing, and monitor circulation.
History and Physical Examination
If cyanosis accompanies less acute conditions, perform a thorough examination. Begin with a history, focusing on cardiac, pulmonary, and hematologic disorders. Ask about previous surgery, prescribed and other drug use, and smoking history. Then, begin the physical examination by taking the patient’s vital signs. Inspect the skin and mucous membranes to determine the extent of cyanosis. Ask the patient when he first noticed the cyanosis. Does it subside and recur? Is it aggravated by cold, smoking, or stress? Is it alleviated by massage or rewarming? Check the skin for coolness, pallor, redness, pain, and ulceration. Also, note clubbing.
Next, evaluate the patient’s level of consciousness. Ask about headaches, dizziness, or blurred vision. Then, test his motor strength. Ask about pain in the arms and legs (especially with walking)

and about abnormal sensations, such as numbness, tingling, and coldness.
Ask about chest pain and its severity. Can the patient identify aggravating and alleviating factors? Palpate peripheral pulses, and test the capillary refill time. Also, note edema. Auscultate heart rate and rhythm, especially noting gallops and murmurs. Also, auscultate the abdominal aorta and femoral arteries to detect any bruits.
Does the patient have a cough? Is it productive? If so, have the patient describe the sputum. Evaluate his respiratory rate and rhythm. Check for nasal flaring and use of accessory muscles. Ask about sleep apnea. Does the patient sleep with his head propped up on pillows? Inspect the patient for asymmetrical chest expansion or barrel chest. Percuss the lungs for dullness or hyperresonance, and auscultate for decreased or adventitious breath sounds.
Inspect the abdomen for ascites, and test for shifting dullness or fluid wave. Percuss and palpate for liver enlargement and tenderness. Also, ask about nausea, anorexia, and weight loss.
Medical Causes
Arteriosclerotic occlusive disease (chronic). With arteriosclerotic occlusive disease, peripheral cyanosis occurs in the legs whenever they’re in a dependent position. Associated signs and symptoms include intermittent claudication and burning pain at rest, paresthesia, pallor, muscle atrophy, weak leg pulses, and impotence. Late signs are leg ulcers and gangrene.
Bronchiectasis. Bronchiectasis produces chronic central cyanosis. Its classic sign, however, is a chronic productive cough with copious, foul-smelling, mucopurulent sputum or hemoptysis. Auscultation reveals rhonchi and coarse crackles during inspiration. Other signs and symptoms include dyspnea, recurrent fever and chills, weight loss, malaise, clubbing, and signs of anemia. Buerger’s disease. With Buerger’s disease, exposure to cold initially causes the feet to become cold, cyanotic, and numb; later, they redden, become hot, and tingle. Intermittent claudication of the instep is characteristic; it’s aggravated by exercise and smoking and relieved by rest. Associated signs and symptoms include weak peripheral pulses and, in later stages, ulceration, muscle atrophy, and gangrene.
Chronic obstructive pulmonary disease (COPD). Chronic central cyanosis occurs in advanced stages of COPD and may be aggravated by exertion. Associated signs and symptoms include exertional dyspnea, a productive cough with thick sputum, anorexia, weight loss, pursed-lip breathing, tachypnea, and the use of accessory muscles. Examination reveals wheezing and hyperresonant lung fields. Barrel chest and clubbing are late signs. Tachycardia, diaphoresis, and flushing may also accompany COPD.
Deep vein thrombosis. With deep vein thrombosis, acute peripheral cyanosis occurs in the affected extremity associated with tenderness, painful movement, edema, warmth, and prominent superficial veins. Homans’ sign can also be elicited.
Heart failure. Acute or chronic cyanosis may occur in patients with heart failure. Typically, it’s a late sign and may be central, peripheral, or both. With left-sided heart failure, central cyanosis occurs with tachycardia, fatigue, dyspnea, cold intolerance, orthopnea, a cough, a ventricular or an atrial gallop, bibasilar crackles, and a diffuse apical impulse. With right-sided heart failure, peripheral cyanosis occurs with fatigue, peripheral edema, ascites, jugular vein distention, and hepatomegaly.
Lung cancer. Lung cancer causes chronic central cyanosis accompanied by a fever, weakness, weight loss, anorexia, dyspnea, chest pain, hemoptysis, and wheezing. Atelectasis causes

mediastinal shift, decreased diaphragmatic excursion, asymmetrical chest expansion, a dull percussion note, and diminished breath sounds.
Peripheral arterial occlusion (acute). Peripheral arterial occlusion produces acute cyanosis of one arm or leg or, occasionally, both legs. The cyanosis is accompanied by sharp or aching pain that worsens when the patient moves. The affected extremity also exhibits paresthesia, weakness, and pale, cool skin. Examination reveals a decreased or an absent pulse and increased capillary refill.
Pneumonia. With pneumonia, acute central cyanosis is usually preceded by a fever, shaking chills, a cough with purulent sputum, crackles, rhonchi, and pleuritic chest pain that’s exacerbated by deep inspiration. Associated signs and symptoms include tachycardia, dyspnea, tachypnea, diminished breath sounds, diaphoresis, myalgia, fatigue, a headache, and anorexia.
Pneumothorax. A cardinal sign of pneumothorax, acute central cyanosis is accompanied by sharp chest pain that’s exacerbated by movement, deep breathing, and coughing; asymmetrical chest wall expansion; and shortness of breath. The patient may also exhibit rapid, shallow respirations; a weak, rapid pulse; pallor; jugular vein distention; anxiety; and the absence of breath sounds over the affected lobe.
Polycythemia vera. A ruddy complexion that can appear cyanotic is characteristic in polycythemia vera, which is a chronic myeloproliferative disorder. Other findings include hepatosplenomegaly, a headache, dizziness, fatigue, aquagenic pruritus, blurred vision, chest pain, intermittent claudication, and coagulation defects.
Pulmonary edema. With pulmonary edema, acute central cyanosis occurs with dyspnea; orthopnea; frothy, blood-tinged sputum; tachycardia; tachypnea; dependent crackles; a ventricular gallop; cold, clammy skin; hypotension; a weak, thready pulse; and confusion.
Pulmonary embolism. Acute central cyanosis occurs when a large embolus causes significant obstruction of the pulmonary circulation. Syncope and jugular vein distention may also occur. Other common signs and symptoms include dyspnea, chest pain, tachycardia, a paradoxical pulse, a dry or productive cough with blood-tinged sputum, a low-grade fever, restlessness, and diaphoresis.
Raynaud’s disease. With Raynaud’s disease, exposure to cold or stress causes the fingers or hands first to blanch and turn cold, then become cyanotic, and finally to redden with a return to a normal temperature. Numbness and tingling may also occur. Raynaud’s phenomenon describes the same presentation when associated with other disorders, such as rheumatoid arthritis, scleroderma, or lupus erythematosus.
Shock. With shock, acute peripheral cyanosis develops in the hands and feet, which may also be cold, clammy, and pale. Other characteristic signs and symptoms include lethargy, confusion, an increased capillary refill time, and a rapid, weak pulse. Tachypnea, hyperpnea, and hypotension may also be present.
Sleep apnea. When chronic and severe, sleep apnea causes pulmonary hypertension and cor pulmonale (right-sided heart failure), which can produce chronic cyanosis.
Special Considerations
Provide supplemental oxygen to relieve shortness of breath, improve oxygenation, and decrease cyanosis. However, deliver small doses (2 L/minute) in the patient with COPD and in the patient with mild COPD exacerbations. These patients may retain carbon dioxide. However, for acute situations, a
high-flow oxygen rate may be needed initially. Simply remember to be attentive to the patient’s respiratory drive and adjust the amount of oxygen accordingly. Position the patient comfortably to ease breathing. Administer a diuretic, bronchodilator, antibiotic, or cardiac drug as needed. Make sure the patient gets sufficient rest between activities to prevent dyspnea.
Prepare the patient for such tests as arterial blood gas analysis and complete blood count to determine the cause of cyanosis.
Patient Counseling
Instruct the patient to seek medical attention if cyanosis occurs. Discuss the safe use of oxygen in the home.
Pediatric Pointers
Many pulmonary disorders responsible for cyanosis in adults also cause cyanosis in children. In addition, central cyanosis may result from cystic fibrosis, asthma, airway obstruction by a foreign body, acute laryngotracheobronchitis, or epiglottitis. It may also result from a congenital heart defect such as transposition of the great vessels that causes right-to-left intracardiac shunting.
In children, circumoral cyanosis may precede generalized cyanosis. Acrocyanosis (also called “glove and bootee” cyanosis) may occur in infants because of excessive crying or exposure to cold. Exercise and agitation enhance cyanosis, so provide comfort and regular rest periods. Also, administer supplemental oxygen during cyanotic episodes.
Geriatric Pointers
Because elderly patients have reduced tissue perfusion, peripheral cyanosis can present even with a slight decrease in cardiac output or systemic blood pressure.
REFERENCES
Khemani, R. G., Patel, N. R., Bart, R. D., & Newth, C. J. (2009) . Comparison of the pulse oximetric saturation/fraction of inspired oxygen ratio and the PaO2/fraction of inspired oxygen ratio in children. Chest, 135(3), 662–668.
Thomas, N. J., Shaffer, M. L., Willson, D. F. , Shih, M. C., & Curley, M. A. (2010). Defining acute lung disease in children with the oxygenation saturation index. Pediatric Critical Care Medicine, 11(1), 12–17.

D
Decerebrate Posture
(See Also Decorticate Posture) [Decerebrate rigidity, abnormal extensor reflex]
Decerebrate posture is characterized by adduction (internal rotation) and extension of the arms, with the wrists pronated and the fingers flexed. The legs are stiffly extended, with forced plantar flexion of the feet. In severe cases, the back is acutely arched (opisthotonos). This sign indicates upper brain stem damage, which may result from primary lesions, such as infarction, hemorrhage, or tumor; metabolic encephalopathy; a head injury; or brain stem compression associated with increased intracranial pressure (ICP).
Decerebrate posture may be elicited by noxious stimuli or may occur spontaneously. It may be unilateral or bilateral. With concurrent brain stem and cerebral damage, decerebrate posture may affect only the arms, with the legs remaining flaccid. Alternatively, decerebrate posture may affect one side of the body and decorticate posture the other. The two postures may also alternate as the patient’s neurologic status fluctuates. Generally, the duration of each posturing episode correlates with the severity of brain stem damage. (See Comparing Decerebrate and Decorticate Postures , page 216.)
 EMERGENCY INTERVENTIONS
EMERGENCY INTERVENTIONS
Your first priority is to ensure a patent airway. Insert an artificial airway, and institute measures to prevent aspiration. (Don't disrupt spinal alignment if you suspect spinal cord injury.) Suction the patient as necessary.
Next, examine spontaneous respirations. Give supplemental oxygen, and ventilate the patient with a handheld resuscitation bag, if necessary. Intubation and mechanical ventilation may be indicated. Keep emergency resuscitation equipment handy. Make sure to check the patient's chart for a do-not-resuscitate order.
History and Physical Examination
After taking the patient’s vital signs, determine his level of consciousness (LOC). Use the Glasgow Coma Scale as a reference. Then, evaluate the pupils for size, equality, and response to light. Test deep tendon reflexes and cranial nerve reflexes, and check for doll’s eye sign.
Next, explore the history of the patient’s coma. If you can’t obtain this information, look for clues to the causative disorder, such as hepatomegaly, cyanosis, diabetic skin changes, needle tracks, or obvious trauma. If a family member is available, find out when the patient’s LOC began deteriorating. Did it occur abruptly? What did the patient complain of before he lost consciousness? Does he have a
history of diabetes, liver disease, cancer, blood clots, or aneurysm? Ask about any accident or trauma responsible for the coma.
Medical Causes
Brain stem infarction. When brain stem infarction produces a coma, decerebrate posture may be elicited. Associated signs and symptoms vary with the severity of the infarct and may include cranial nerve palsies, bilateral cerebellar ataxia, and sensory loss. With deep coma, all normal reflexes are usually lost, resulting in the absence of doll’s eye sign, a positive Babinski’s reflex, and flaccidity.
Cerebral lesion. Whether the cause is trauma, a tumor, an abscess, or an infarction, any cerebral lesion that increases ICP may also produce decerebrate posture. Typically, this posture is a late sign. Associated findings vary with the lesion’s site and extent, but commonly include coma, abnormal pupil size and response to light, and the classic triad of increased ICP — bradycardia, increasing systolic blood pressure, and a widening pulse pressure.
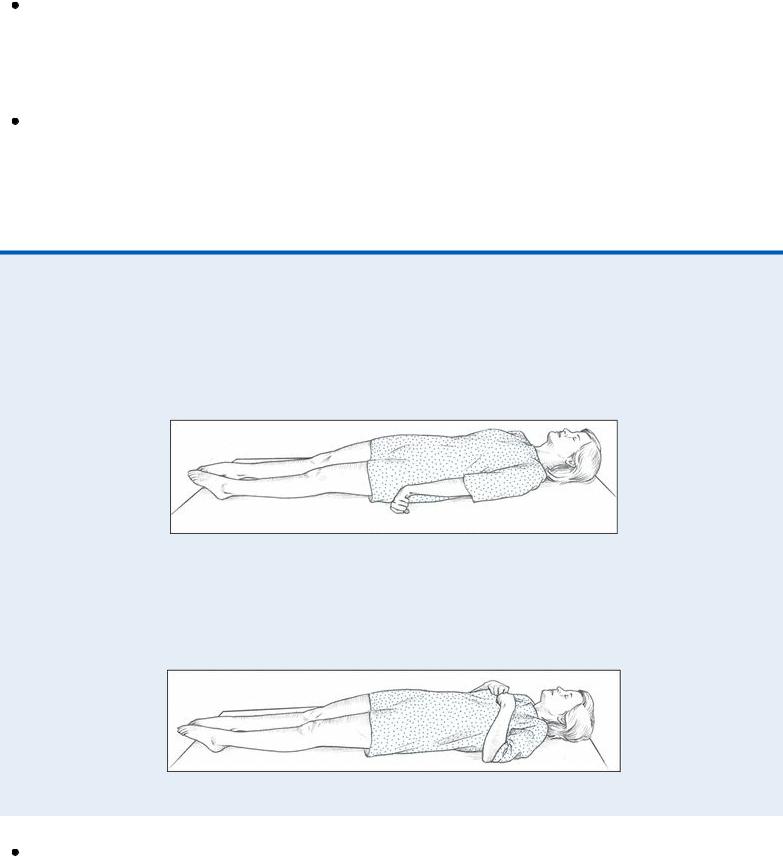
Comparing Decerebrate and Decorticate Postures
Decerebrate posture results from damage to the upper brain stem. In this posture, the arms are adducted and extended, with the wrists pronated and the fingers flexed. The legs are stiffly extended, with plantar flexion of the feet.
Decorticate posture results from damage to one or both corticospinal tracts. In this posture, the arms are adducted and flexed, with the wrists and fingers flexed on the chest. The legs are stiffly extended and internally rotated, with plantar flexion of the feet.
Hepatic encephalopathy. Hepatic encephalopathy, deterioration of the brain, occurs when the liver is not able to function normally to remove toxic substances, thus allowing them to enter the brain and nervous system. Decerebrate posturing and coma occur in the later stage of hepatic
