
Книги по МРТ КТ на английском языке / Advanced Imaging of the Abdomen - Jovitas Skucas
.pdf
17
Abdominal Vasculature
Technique
Computed Tomography
Contrast-enhanced computed tomography (CT) can visualize the major aortic branches on early-phase and venous branches on late-phase images. Late images also evaluate the portal phase. Most radiologists use a nonionic contrast agent, with a typical intravenous (IV) injection consisting of 150mL at a rate of about 4 to 5mL/sec. A faster injection rate produces earlier and greater vascular enhancement than a slower rate. A test bolus injection or automatic bolus triggering optimizes contrast enhancement (more details on CT angiography are in Chapter 7).
Three-dimensional (3D) image reconstruction is helpful in evaluating overlapping arteries and veins; the aorta, main arterial branches, as well as vena cava and portal vein branches are usually identified. Preoperative reconstructed 3D CT angiography is useful to surgeons in planning complex intraabdominal procedures, especially if unusual vascular paths are present. Reconstruction techniques include surface rendering, maximum intensity projection (MIP) and volume rendering; the latter utilizes more of the available data and generally is more accurate. A multiple threshold display technique decreases artifacts and allows better small vessel depiction than a shaded surface display technique. Each technique has its advantages and disadvantages (Fig. 17.1).
Similar to virtual colonoscopy, virtual CT arterial endoscopy is also feasible. In theory, a stenosis, aneurysm, or stent could be evaluated from its endoluminal surface. In practice, such applications are still being developed.
Computed tomography arterial portography and CT hepatic arteriography are discussed in Chapter 7. These techniques are of value primarily in the study of the liver blood supply. Evaluation of CT arterial portography images is not always straightforward, most often due to flow artifacts caused by nonopacified blood.
Ultrasonography
Doppler ultrasonography (US) measures blood flow velocity in larger vessels. Superior mesenteric artery and renal artery blood flow velocities can be measured even in neonates.
The use of intravascular contrast agents enhances portal vein and collateral blood flow during Doppler US studies. One IV US contrast agent is Perflenapent emulsion (EchoGen, Sonus Pharmaceuticals, Bothell, WA), providing enhancement lasting 5 to 15 minutes. Continuous infusion, rather than bolus injection, prolongs enhancement and decreases saturation artifacts.
Transesophageal echocardiography has evolved into a valuable thoracic aortic study, especially in a setting of suspected aortic dissection, postoperative repair, and follow-up. Echocardiography also evaluates the extent
975

976
ADVANCED IMAGING OF THE ABDOMEN
A |
B |
|
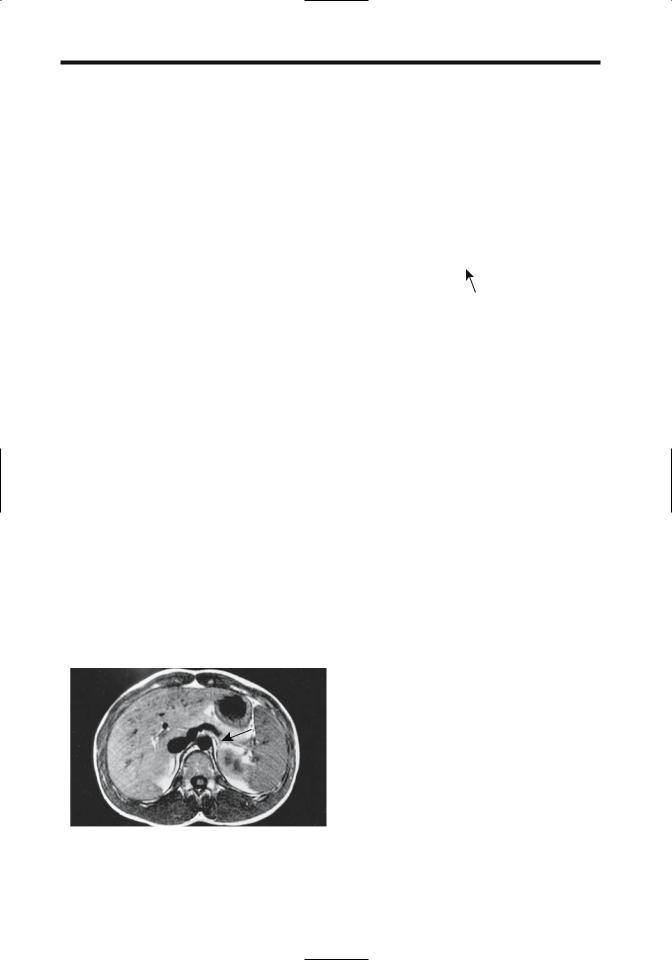
Figure 17.1. Computed tomography (CT) portal vein techniques. |
|
A: Maximum intensity projection. B: Shaded surface display. C: |
|
Volume-rendered CT portal venography. Dilated left gastric vein |
|
(arrow) is seen in A. The maximum intensity projection technique |
|
provided best visualization of collateral vessels. (Source: Kang HK, |
|
Jeong YY, Choi JH, et al. Three-D Multi-detector Row CT Portal |
|
Venography in Evaluation of Portosystemic Collateral Vessels in |
|
Liver Cirrhosis. RadioGraphics 2002;22:1053–1061, with permis- |
C |
sion from the Radiological Society of North America.) |
of atherosclerosis, aortic ulcers, intramural |
shortening effect of IV contrast, contrast- |
hematomas, and blood flow. |
enhanced MRA sequences result in flowing |
Intravascular US holds promise in evaluating |
blood being bright while stationary objects are |
vessel wall morphology. It has been called a |
saturated and appear “dark.” A further |
technology in search of an application and is |
refinement of this technique is subtraction of |
gradually finding a role in endovascular inter- |
precontrast images from postcontrast ones, |
vention procedures. |
improving vessel contrast resolution. |
|
Compared to digital subtraction angiography |
Magnetic Resonance |
(DSA), the sensitivity and specificity percents |
|
of MRA in detecting major vessel stenoses or |
Currently magnetic resonance angiography |
occlusions are in the high 90% range. Currently, |
(MRA) is an alternate vascular imaging modal- |
the major constraints of abdominal vessel MRA |
ity in patients with a contraindication to iodi- |
include the pulsatile nature of blood flow, |
nated contrast agents. Its future indications will |
respiratory motion, and peristalsis. The use of |
undoubtedly increase considerably, mostly at |
heavily T2-weighted fast turbo spin echo |
the expense of invasive angiography. |
sequences instead of conventional T2-weighted |
Intraluminal blood has a varied MR appear- |
SE sequences improves image quality. Fast GRE |
ance depending on the technique used; it ranges |
sequences allow dynamic contrast-enhanced |
from a signal void on spin echo (SE) sequences |
vascular studies using single breath-hold image |
to being hyperintense on gradient-recalled echo |
acquisition and result in few motion artifacts. |
(GRE) sequences. Conventional T1and T2- |
Useful techniques include time of flight and |
weighted SE techniques result in flowing blood |
phase contrast. The former consists of a varia- |
appearing dark. An exception is with slow- |
tion in signal intensity with time due to proton |
flowing blood, which tends to mimic a |
motion within a magnetic field, while the latter |
thrombus and appears bright. Due to the T1- |
monitors phase variations; each has certain |

977
ABDOMINAL VASCULATURE
advantages and limitations. A 2D time-of-flight technique permits 3D reconstruction images. The phase-contrast technique is useful in evaluating portal vein blood; it measures flow direction and velocity.
The relative merits of MRA versus computed tomography angiography (CTA) are still evolving. Mention of angiography in CT implies the use of an intravascular contrast agent. This is not necessarily true with MRA, because MRA without contrast enhancement is feasible. Flowing fluid can be made to produce a signal void and thus appear black (black blood technique) or appear bright. Limitations of MRA without contrast include the presence of slow flow and spin-dephasing signal voids induced by turbulence. In general, contrastenhanced MRA of abdominal vessels is superior to noncontrast time-of-flight or phase-contrast MRA.
A T1-weighted 3D MRA technique using gradient-echo [fast imaging with steady-state precision (FISP)] with ultrashort echo and repetition times obtained during the arterial phase after IV contrast overcomes a number of limitations of no-contrast techniques; images are obtained within 20 to 40 seconds during a breath-hold. At times a subtraction technique using precontrast images is helpful. Contrastenhanced MRA of the portal vein is hampered by slow flow, and in this situation a time-of- flight technique is more appropriate.
Both 2D and 3D gadolinium-enhanced MRA evaluate major vessels. Thus MRA performed with four 3D acquisitions (at 0, 30, 60, and 90 seconds after IV gadolinium) provides an arteriogram (without veins) in most patients during the second or third acquisitions and a venogram by subtracting the arterial phase from an arteriovenous phase (third or fourth acquisition) (1); all major vessels, including portal vein and superior mesenteric vein, can be visualized, but secondary branches are better shown by conventional angiography. Veins <5mm in diameter are often not well seen with MRA.
Using gadolinium-enhanced MRA, MIP postprocessing provides vascular phase images that can then be reformatted into 3D images viewed along a 360-degree axis. The use of gadolinium results in arterial phase images without the need for subtraction, but a subtraction technique is necessary for venous-phase imaging. The entire intraabdominal aorta can be visualized with 3D
gadolinium-enhanced MRA, and this technique appears useful in studying aortic aneurysms and dissections. Virtual MR intraarterial endoscopy is feasible using gadoliniumenhanced gradient echo MRI and a postprocessing algorithm to obtain aortic and renal artery images; the clinical usefulness of such a technique remains to be established. Combining gadolinium-enhanced MRA with 3D phase contrast MRA provides additional information than is possible with each technique separately. Both the aorta and renal arteries can be evaluated; the former results in images similar to a contrast arteriogram, while the latter is based on flow characteristics and is useful to identify vascular stenoses.
Similar to CT, either a test dose or an assumed time interval establish a delay between the start of contrast injection and initial image acquisition for optimal arterial enhancement. Another approach is to monitor a single voxel within the aorta and use an increase in signal within this voxel (corresponding to the arrival of injected gadolinium) to trigger MR angiography. Such automatic triggering improves arterial enhancement compared to manual triggering; venous enhancement is also less than with manual triggering. The advantages of such automatic triggering can be used two ways—either to obtain increased arterial enhancement or a similar enhancement to manual triggering but using a reduced contrast dose.
Magnetic resonance contrast agents are discussed in more detail in Chapter 7. Ultrasmall superparamagnetic iron oxide (SPIO) particles shorten both T1 and T2 relaxation times, have a blood half-life measured in hours, and thus are known as blood-pool MR contrast agents. Equi- librium-phase 3D MRA using SPIO readily evaluates abdominal and pelvic arteries, but venous overlap limits their use. They also depict the portal vein and its major branches. These small iron oxide particles pass through capillaries and are eventually cleared by lymph nodes.
Contrast enhanced 3D MR portography identifies the main portal vein and right and left intrahepatic portal veins with their main branches (2); MR portography also detects varices and portosystemic shunts. In a setting of liver tumors it can confuse vein occlusion with narrowing.
Magnetic resonance venography is also feasible. An electrocardiogram (ECG)-triggered

978
black-blood half-Fourier acquisition singleshot turbo spin echo (HASTE) sequence assesses the vena cava and major veins. Good quality pelvic and abdominal vein images are obtained by using a 2D fast low-angle shot (FLASH) time-of-flight technique without breath-hold but with arterial presaturation (3). Major venous obstructions, thrombi, and intravascular tumors can be detected. Contrastenhanced 3D MRA is necessary for more detailed study.
Contrast enhanced MR lymphography, performed after interstitial or iv injection is theoretically feasible and undoubtedly will be performed in the future once appropriate contrast agents are available.
Scintigraphy
An estimate of portal blood shunting can be obtained with perrectal portal scintigraphy. A solution of technetium–99m (Tc-99m) pertechnetate is instilled into the rectum, and serial liver and heart scintigrams are obtained and a portal shunt index calculated. In a longitudinal study of patients with liver disease ranging from chronic hepatitis to cirrhosis and varices, the shunt index initially increased gradually as the patient’s disease progressed to cirrhosis and then increased rapidly as varices developed (4). The clinical role of this test is not clear.
Angiography
Systemic Circulation
Catheter-based DSA is an often-used gold standard when evaluating other imaging modalities. Although DSA is often supplanted in this role by CTA and MRA, conventional angiography continues to serve as a framework for angioplasty, stent placement, and various embolization techniques.
Compared to conventional DSA, 3D images obtained with subtraction angiography performed by rotating the x-ray tube during contrast injection (digital rotational subtraction angiography) tend to be superior in most patients (5).
Percutaneous arterial puncture and catheter manipulation should be performed with caution in patients with Behçet’s disease. These
ADVANCED IMAGING OF THE ABDOMEN
patients have a higher than normal prevalence of aneurysms and are at increased risk of (pseudo)aneurysm formation and thrombophlebitis at a puncture site. If feasible, either CTA or MRA is a viable alternate study.
Diagnostic renal angiography and percutaneous renal intervention procedures using carbon dioxide are options in patients with renal insufficiency.
Although gadolinium contrast has been occasionally used for angiographic studies and CT imaging in patients with renal insufficiency or prior severe reaction to an iodinated agent (6), one should keep in mind that the pharmacokinetic properties of Gd-DTPA, with only one gadolinium ion, are similar to iodinated agents containing 3 to 6 iodine atoms. Toxicity of gadolinium agents, at doses achieving equivalent x-ray stopping power, is greater than with nonionic iodinated agents (7). This is in distinction to the use of approved lower gadolinium MR doses, which are insufficient for useful x-ray contrast, but which have negligible nephrotoxicity (8). The European Society of Urogenital Radiology position is that gadolinium-based contrast agents are more nephrotoxic than iodinated contrast agents in equivalent x-ray attenuation doses (9) and their use for angiography and CT is not recommended.
Gelatin sponge is often used as an embolic material. Being inherently radiolucent, contrast agents are often mixed with it if visualization is desired. Some investigators find Lipiodol more useful than a water-soluble contrast material.
Portal System
Direct portography is performed either by injecting an intrahepatic portal vein branch or via splenic pulp injection (splenoportography). A transjugular approach through an intrahepatic portosystem shunt is an option in select patients. Indirect portography is an arteriographic procedure consisting of contrast injection into either the superior mesenteric or splenic arteries.
Direct transhepatic portography is useful to evaluate and treat some portosystemic collateral pathways in patients with portal hypertension; although this technique has been supplanted by newer procedures, in selected patients it pro-

979
ABDOMINAL VASCULATURE
vides excellent opacification of the portal vein and its branches. Selective superior mesenteric vein catheterization permits dynamic portal venous blood flow studies. Direct splenoportography enjoyed its golden age in the early 1970s, being supplanted initially by other angiographic procedures and then by CT arterial portography. It is currently little used, although an occasional investigator rediscovers it as a “new procedure.” Computed tomographic portography performed by direct intrasplenic contrast injection using a needle-catheter assembly is a simple procedure having a role in an occasional patient when other access to the portal vein is impractical. Direct splenoportography using carbon dioxide through a small needle fills a useful but rather select niche (10).
Hepatic venography is performed by selective hepatic vein catheterization. If needed,a balloon occludes hepatic vein outflow, thus permitting contrast opacification of hepatic parenchyma, an aid in detecting intrahepatic venous collaterals.
Wedge hepatic venography using carbon dioxide is little used but at times is an adjunct to study the portal venous system. Carbon dioxide hepatic venography can visualize the portal vein in most patients and splenic and superior mesenteric veins in over half of patients.
Congenital Abnormalities
Aorta
Isolated congenital abdominal aortic abnormalities are uncommon; most are associated with other anomalies and are discussed in Chapter 14 under the heading Heterotaxy Syndrome.
Congenital abdominal aortic coarctation is uncommon. Symptoms in these patients range from hypertension, to intermittent claudication, and abdominal pain. A patient with Alagille’s syndrome and abdominal aortic coarctation also had an aberrant splanchnic blood supply (11).
Vena Cava
Most inferior vena caval abnormalities occur inferior to the renal veins. The absence of the infrarenal portion is rare; more often, mention
of an absent vena cava describes azygous continuation of a patent infrarenal segment, with hepatic veins draining directly into the right atrium. Such azygos inferior vena cava continuation is associated with cardiac and situs anomalies. In these patients the renal artery is located ventral to the azygos vein, a finding detectable by abdominal US. Azygous continuation of the vena cava is common in patients with polysplenia. Occasionally, indirect azygous continuation is associated with an inferior vena caval aneurysm. Hemiazygous continuation is rare.
Agenesis of other inferior vena cava segments is rare. One patient with agenesis of the hepatic segment had the infrahepatic vena cava draining into the portal vein and hepatic veins draining into a suprahepatic inferior vena cava (12). Hypoplasia of the inferior vena cava is also rare; these patients tend to have an extensive collateral circulation.
In inferior vena caval transposition a single vein ascends on the left, crosses the midline at the renal vein level, and continues its ascent to the right atrium. A duplicated left vena cava is rare; when present, the two vena cavae join at the renal vein level. A left vena cava can be differentiated from a dilated gonadal vein by tracing its cranial and caudal extensions. As expected, thrombophlebitis of a left vena cava is difficult to detect; CT and MR tend to suggest adenopathy, and aspiration biopsy or surgical exploration are often performed.
Arteries
An independent hepatic and splenic artery origin from the abdominal aorta occurs in approximately 1% of the population, an anomaly detected with contrast-enhanced CT and angiography. A common origin of the celiac, superior mesenteric, and inferior mesenteric arteries is very rare (13). A middle mesenteric artery, originating from the aorta, also a rare anomaly, usually supplies the right and transverse portions of the colon.
A hepatic artery identified by US in the portacaval space is often believed to have a superior mesenteric artery origin, yet one originating from the celiac artery can also be detected in this space.
980
ADVANCED IMAGING OF THE ABDOMEN
A 
 B
B
Figure 17.2. Retroaortic left renal vein. Frontal (A) and oblique (B) 3D CT reconstructions reveal the left renal vein (arrows) posterior to a tortuous aorta. (Courtesy of Patrick Fultz, M.D., University of Rochester.)
Veins
Systemic Veins
A retroaortic left renal vein, located either at the same level as a normal renal vein or more caudally, occurs in about 5% of the population (Fig. 17.2). Circumaortic left renal veins consist of a true vascular ring and also occur roughly in about 5%, findings detected with contrast enhanced CT. Gadolinium enhanced 3D MRA detects a retroaortic and circumaortic left renal veins with roughly the same frequency.
An abdominal aortic aneurysm can compress a retroaortic left renal vein and result in renal vascular congestion and induce hematuria (14). Although at times called a nutcracker phenomenon, this term is best avoided to prevent confusion with other similarly named conditions.
Portal Venous System
Congenital portal venous absence is rare; most occur in females and tend to be associated with liver tumors and other congenital abnormalities (Fig. 17.3). With an absent portal vein, intestinal
A  B
B
Figure 17.3. Congenital absence of portal vein in an 11-year-old boy. A: Transverse magnetic resonance (MR) imaging shows the splenic vein (arrows) joining the superior mesenteric vein and emptying into the inferior vena cava. B: An MR angiogram identifies the superior mesenteric vein (arrow) draining into inferior vena cava. (Source: Kohda E, Saeki M, Nakano M, et al. Congenital absence of the portal vein in a boy. Pediatric Radiology 1999;29:235–237, with permission from Springer-Verlag.)

981
ABDOMINAL VASCULATURE
and splenic venous blood bypasses the liver and drains directly into systemic veins. Some of these patients develop hepatofugal drainage of a large inferior mesenteric vein into systemic veins.
Congenital portal vein duplication or an accessory portal vein is also rare. Some of these mimic a liver hilar tumor. At times direct portography shows an accessory smaller vein located parallel to the main portal vein and draining into the right liver lobe; some of these accessory portal veins drain the coronary veins, thus modifying results obtained after a transjugular intrahepatic portosystemic shunt (TIPS) and preventing coronary vein embolization.
A portal vein located cranial to the gallbladder bed and feeding the right anterior segment is associated with rightward deviation of the ligamentum teres. A portal vein located anterior to the duodenum (and thus prepancreatic in location) is associated with malrotation and polysplenia. Computed tomography and magnetic resonance imaging (MRI) reveal a vascular structure anterior to the head of the pancreas.
Aberrant gastric venous drainage is common and accounts for some of the unusual liver enhancement patterns detected.Veins of Retzius are intestinal veins draining directly into vena cava or its branches—usually the gonadal or renal veins—rather than into portal vein branches. Whether they represent a normal variant or should be considered congenital anomalies is conjecture. These veins can be identified if searched for, including with CT arterial portography.
Ultrasonography can detect portocaval anastomoses in infants; these vessels probably represent continued ductus venosus patency.
Normally the superior mesenteric vein lies to the right and anterior to the superior mesenteric artery. A reversed position of these two vessels suggests but is not pathognomonic of midgut malrotation.
An aberrant right gastric vein supplies segment 4 of the liver and is a cause of a pseudolesion during contrast-enhanced CT or CT portography. An aberrant left gastric vein is less common and is identified on postcontrast CT along the hepatogastric ligament. These veins provide a partial collateral pathway for the portal system.
Trauma
Abdominal aortic injury is considerably less common than to the thoracic aorta. Nevertheless, abdominal aortic and inferior vena caval injuries are associated with a high morbidity and mortality. Unchecked bleeding, shock, and injury superior to the renal vessels all play a role in increased mortality.
On rare occasions intravascular gas is detected after trauma; portal venous gas, hepatic venous gas, and inferior vena cava gas in five patients cleared on follow-up studies and no cause was determined (15).
Aortic Injury
Thoracic aortic injuries are not discussed in this book, but mention should be made of delayed aortoesophageal fistulas developing after swallowing sharp objects or after gunshot wounds.
Abdominal aortic injury should be suspected with lumbar spine transverse process fractures. Handlebar injuries to the duodenum are well known to trauma physicians. Less well known is aortic injury due to a similar mechanism. Fatal delayed abdominal aortic ruptures have occurred after handlebar injury.
In the United States, contrast-enhanced CT is the current imaging modality used to evaluate suspected aortic trauma. A periaortic hematoma detected near the diaphragm level is an insensitive but specific sign of aortic injury (16).
Blunt abdominal aortic injury carries a high morbidity and mortality. Some traumatic inframesenteric abdominal aortic dissections can be successfully treated with implanted stents. In general, surgical repair is preferred for an unstable patient or those with threatened extremities, but angiographic endovascular stent placement appears to be an option in a stable patient with viable limbs.
Arterial Trauma
An arterial (pseudo)aneurysm is a known complication of trauma in both children and adults. The hepatic artery is a common location for these aneurysms, although any artery, even the inferior epigastric artery, can be involved. These aneurysms tend to remain silent until manifest-

982
ing by bleeding, often weeks or, rarely, even years later. Most such delayed bleeding is into the gastrointestinal tract,with an occasional one to respiratory or urinary tracts. At times bleeding is massive, stops spontaneously, but invariably recurs later.
Less common are posttraumatic arteriovenous fistulas; most are due to penetrating injury. Although CT is often useful in suggesting the diagnosis, arteriography is generally necessary to define the location and extent of these fistulas.
Many detected aneurysms are treated successfully by transcatheter embolization. An unresolved question is whether such embolization is indeed advantageous to the patient or whether conservative management achieves a similar end, especially with smaller, uncomplicated aneurysms. In patients with arterial injuries managed nonoperatively, follow-up arteriography reveals that some injuries heal spontaneously, some improve with residual deformity and others worsen; the dilemma is that pretherapy imaging is not accurate enough in selecting those who are expected to improve and those who progress.
Venous Trauma
Trauma to the inferior vena cava consists of contusion, laceration, transection, and, rarely, dissection. In particular, injury to the retrohepatic portion of the vena cava is associated with a poor prognosis.
Peritoneal lavage readily misses inferior vena cava injuries. Typically CT shows a hematoma surrounding the vena cava. Some hematomas are associated with an intraluminal thrombus. At times CT in patients with traumatic inferior vena cava rupture identifies contrast extravasation. Computed tomography detection of a collapsed inferior vena cava during a trauma study suggests hypovolemia.
Trauma is a rare cause of Budd-Chiari syndrome. Presumably bleeding and extrinsic compression of the intrahepatic inferior vena cava by a hematoma obstruct the hepatic veins or intrahepatic portion of the inferior vena cava, findings detectable by CT. Ascites is common and should be differentiated from intraperitoneal bile or blood, which suggest other etiologies for intraperitoneal fluid. An occasional patient develops traumatic Budd-Chiari syn-
ADVANCED IMAGING OF THE ABDOMEN
drome secondary to inferior vena cava thrombosis. On the other hand, with hepatic vein rupture generally not enough time elapses for Budd-Chiari syndrome to develop.
Bleeding
Active hemorrhage in a trauma setting is recognized as contrast extravasation during contrast-enhanced CT. Rapid infusion of a relatively large contrast bolus aids in detecting a site of arterial extravasation, less so with venous bleeding. Multislice CT appears to be superior to more conventional CT in detecting more subtle bleeds. Even if active extravasation is not detected, a high-density region, having a Hounsfield density close to that of adjacent arteries and surrounded by lower density clot, should suggest recent extravasation. These are often subtle findings requiring expertise in interpretation.
Occasionally Tc-99m–red blood cell scintigraphy locates a bleeding site; the radiotracer accumulates in one particular region, with no change in location during the study.
The appearance of a pseudoaneurysm is similar to that of arterial bleeding (Fig. 17.4). Some authors consider bleeding to represent a
Figure 17.4. Traumatic pseudoaneurysm secondary to gunshot wound. Computed tomography identifies the aneurysm (arrows) between the aorta and inferior vena cava. (Courtesy of Patrick Fultz, M.D., University of Rochester.)
983
ABDOMINAL VASCULATURE
pseudoaneurysm if it is contained, but this distinction is rather subtle. In either case, a pseudoaneurysm should be isodense to its connecting vessel and, being contained, should be sharply marginated.
Aorta
Atherosclerosis/Stenosis
For unknown reasons, smokers and patients with chronic pancreatitis have a higher prevalence of aortic calcifications than controls. Alagille syndrome includes arteriohepatic dysplasia; occasionally aortic calcifications develop even in teenagers with this syndrome.
High-resolution T2-weighted MRI aids in detecting and classifying atherosclerotic plaques (17).
Abdominal aortic stenosis is occasionally discovered in children. A majority of these consist of congenital malformations and a minority of inflammatory aortitis; associated renal and visceral artery involvement is common, together with arterial hypertension. Some stenoses in young adults are isolated, with the aortic bifurcation being a common site; some of these stenoses calcify, even in young patients. Atherosclerotic aortic stenoses are quite common in the elderly, although clinically they are often overshadowed by stenoses at the origin of great vessels.
MRA is useful in detecting and evaluating aortic stenoses.
Isolated stenoses are amenable to surgical correction. More common is diffuse involvement of the aorta, iliac arteries and distal vessels. Percutaneous transluminal balloon angioplasty and, if needed, intraluminal stent placement are the interventional modalities used to treat aortic stenosis. Although generally performed under angiographic guidance, intravascular US guidance is also feasible. Angiography alone probably underestimates vessel diameter in almost two-thirds of patients; incomplete stent deployment is also more readily identified by intravascular US than by angiography.
Aortic stent placement is feasible in patients with failure of percutaneous transluminal angioplasty or presence of ulcers, which increases risk of embolization with angioplasty.
In general,similar long-term restenosis rates are found for transluminal angioplasty and stent placement (18); a small aortic diameter is a predictive factor for restenosis.
Follow-up after percutaneous transluminal angioplasty of patients with infrarenal atherosclerotic aortic stenosis shows a clinical patency rate similar to open surgery.
Aneurysm
Atherosclerotic Aneurysm
Most abdominal aortic aneurysms are atherosclerotic in origin. An occasional mycotic one is encountered.
Screening for an abdominal aortic aneurysm is not widely practiced even in hypertensive patients. An abdominal aortic aneurysm in these patients is associated with claudication, and these patients appear to benefit from screening US. An occasional aortic aneurysm is associated with a coagulopathy, which often clears after aneurysm repair.
From a potential therapeutic perspective, an abdominal aortic aneurysm’s size and location are of obvious importance. One classification is into infrarenal, juxtarenal, and pararenal aneurysms. Most common are infrarenal ones, fusiform in shape. Pararenal aneurysms extend distal to the superior mesenteric artery and involve the renal arteries.
The role of imaging is to establish that an aortic aneurysm is indeed present, provide information about its size and shape, detect complications, and outline the preoperative anatomy.
Aneurysms vary in size considerably. Measurement of aneurysm dimensions before endovascular therapy is of obvious importance, yet DSA measurements of an aneurysm’s diameter and length are inaccurate by up to 15% (19); an indwelling catheter is the only available reference standard. Computed tomography, US, or MRA provides more reliable aneurysm dimensions.
Calcifications develop in long-standing aneurysms, but aortic calcifications do not imply that an aneurysm is present. An occasional aneurysm is suggested from a conventional abdominal radiograph, but this study is rarely employed when suspecting an aneurysm. In particular, measurement of a suspected

984
aneurysm’s diameter is notoriously inaccurate on conventional radiographs, but if such a measurement is necessary, a lateral projection rather than a frontal one should be chosen.
Computed tomography angiography is the current preoperative imaging study of choice. Numerous studies confirm accuracy of CT in measuring an aneurysm’s diameter. Multidetector CT in patients evaluated for aortoiliac aneurysms, performed with a 25-second delay after the start of IV contrast injection resulted in aortic enhancement of >200 Hounsfield units (HU) and no superimposed venous filling (20). A 3D shaded surface display is helpful in viewing aneurysms, with image rotation providing multidirectional images. In differentiating among suprarenal, juxtarenal, and infrarenal aneurysms, the use of narrrow collimation and overlapping axial reconstructions aids in correctly classifying most aneurysms and identifies main and accessory renal arteries.
Ultrasonography should identify an aortic aneurysm, outline its shape, and measure its width and rough length in most patients and is often the first screening examination obtained in a patient with a pulsatile abdominal mass. Involvement of other vessels is difficult to evaluate. Obesity and bowel gas limit the information obtained. Doppler US does provide additional information but is generally superfluous if subsequent angiography (CT or other) is obtained.
Magnetic resonance imaging and MRA are evolving into primary imaging modalities for preoperative aneurysm study, at times providing information superior to CT. Potentially 3D MRA can provide definitive pretherapy studies and replace both CT and DSA. Some studies achieve almost perfect agreement between conventional angiography and MRA interpretations of aortic disease. Conventional angiography is often considered the gold standard in aneurysm evaluation primarily because many surgeons are comfortable with its results and rely on its information. Nevertheless, the use of angiography is declining for this indication and is gradually being relegated to those situations where CT and MR are inconclusive.
Magnetic resonance imaging can identify an aneurysm’s size and shape. Transverse images tend to provide more information about the distal aorta and iliac vessels compared to coronal images, but sagittal images are helpful
ADVANCED IMAGING OF THE ABDOMEN
in identifying major vessel origins. Gadoliniumenhanced MRA achieves high sensitivity and specificity in determining whether the renal arteries and iliac arteries are involved by an aneurysm; also, gadolinium aids in differentiating between slow blood flow and a mural thrombus. A 3D gadolinium-enhanced MRA technique identifies an aneurysm and aids in establishing its relationship to renal and other major arteries. Stenosis of major vessels is also detected and atherosclerotic plaques and thrombi are evaluated.
One inherent limitation of MRI is its inability to visualize calcifications. Also, multiple sequences are generally necessary. Thus although arterial-phase MRA visualizes a patent aortic lumen, it does not outline the aortic wall or identify thrombi; for the latter axial imaging is necessary.
Inflammatory Aneurysm
An inflammatory abdominal aortic aneurysm is characterized by marked thickening and inflammation in the aneurysm wall. The etiology is unknown, although an immune response appears to be involved in some patients.
Many inflammatory aneurysms are associated with extensive surrounding extraperitoneal fibrosis. At times the ureters become encased and obstruct. The duodenum or inferior vena cava can also be entrapped. The inflammation often subsides after aneurysm repair and ureteric obstruction is relieved. Computed tomography performed several years after inflammatory aortic aneurysm repair reveals no or little persisting inflammatory tissue in most patients.
A MR study of an inflammatory aortic aneurysm reveals a complex, concentric, layered outline; homogeneous enhancement postcontrast distinguishes this condition from the more common atheromatous intima.
Dissecting Aneurysm
Most dissecting aortic aneurysms are thoracic in origin and dissect into the abdomen. These aneurysms are generally subdivided into those involving the ascending aorta and those originating distal to the great vessels. A dissection is diagnosed by detecting both true and false lumens and identifying an intimal flap. Most
