
Книги по МРТ КТ на английском языке / Advanced Imaging of the Abdomen - Jovitas Skucas
.pdf



907
PERITONEUM, MESENTERY, AND EXTRAPERITONEAL SOFT TISSUES
Table 14.4. Computed tomography differentiation of tuberculous peritonitis and peritoneal carcinomatosis
|
Tuberculous peritonitis |
|
Peritoneal carcinomatosis |
|
Reference |
(62) |
(63) |
(62) |
(63) |
|
|
|
|
|
Number of patients |
42 |
19 |
93 |
19 |
Peritoneal thickening |
|
|
|
|
Slight, smooth |
|
79% |
|
26% |
Irregular |
|
0% |
|
47% |
Peritoneal nodules |
|
0% |
|
37% |
Mesenteric nodules |
|
26% |
|
16% |
<5 mm in diameter |
52% |
|
52% |
|
≥5 mm |
52% |
|
12% |
|
Omental cakes |
8% |
21% |
20% |
37% |
Splenomegaly |
93% |
|
50% |
|
Ascites |
64% |
100% |
84% |
100% |
|
|
|
|
|
toneum. In general, a malignant mesenchymal |
a sarcoma. Two types of mesothelioma exist: the |
|||
neoplasm is more common than its benign |
more common malignant variety and a less |
|||
counterpart. Some poorly differentiated sarco- |
common relatively benign form. Whether these |
|||
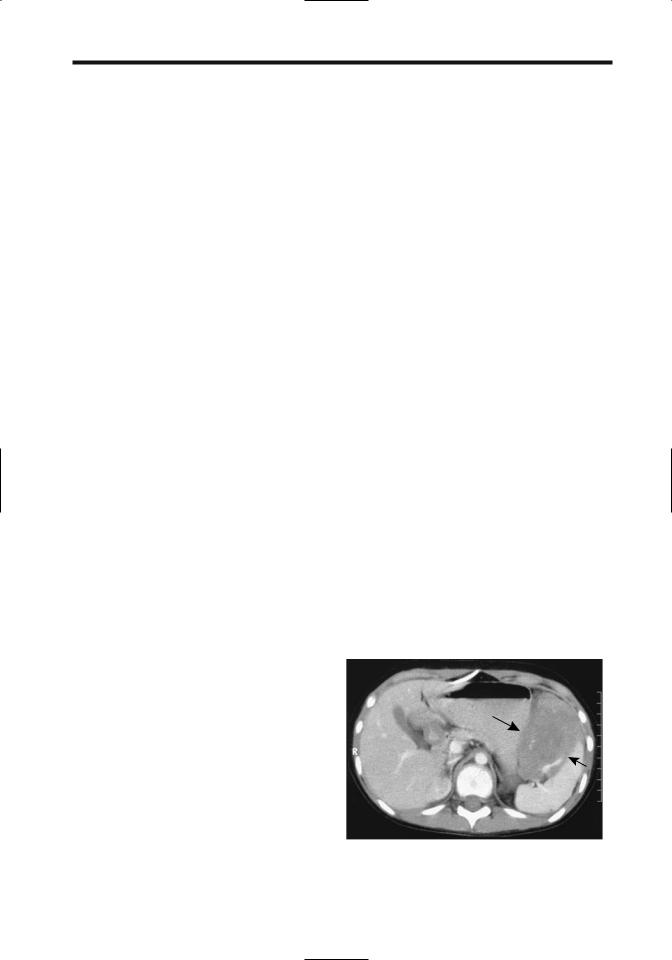
mas are difficult to classify (Fig. 14.18). The rare |
represent a variation of the same entity or are |
|||
peritoneal adenosarcoma probably originates |
different conditions is conjecture. One hypoth- |
|||
from regions of endometriosis. |
esis is that the benign variety simply represents |
|||
Both malignant and benign fibrous tumors |
a proliferation of mesothelioma cells due to a |
|||
develop in the retroperitoneum and peritoneal |
reaction to an insult. In either case, even the |
|||
cavity. Diffuse fibrosis/desmoid tumors have |
benign mesotheliomas tend to recur unless |
|||
been discussed earlier. |
completely resected. |
|||
|
|
|
Both the benign and malignant forms have |
|
Mesothelioma |
similar imaging findings, although some benign |
|||
peritoneal mesotheliomas have a multicystic |
||||
|
|
|
||
A number of authors list mesothelioma as a sep- |
imaging appearance and thus mimic other |
|||
arate type of neoplasm, although it is of mes- |
cystic tumors. These tumors range from small |
|||
enchymal origin, and the most common form is |
peritoneal nodules,large tumors,to diffuse peri- |
|||
|
|
|
|
|
A B
Figure 14.18. Poorly differentiated mesenteric sarcoma. A,B: Two CT images show a homogeneous midabdominal tumor (arrows) displacing contrast-filled small bowel loops. (Courtesy of Algidas Basevicius, M.D., Kaunas Medical University, Kaunas, Lithuania.)







 B
B B
B