
Книги по МРТ КТ на английском языке / Advanced Imaging of the Abdomen - Jovitas Skucas
.pdf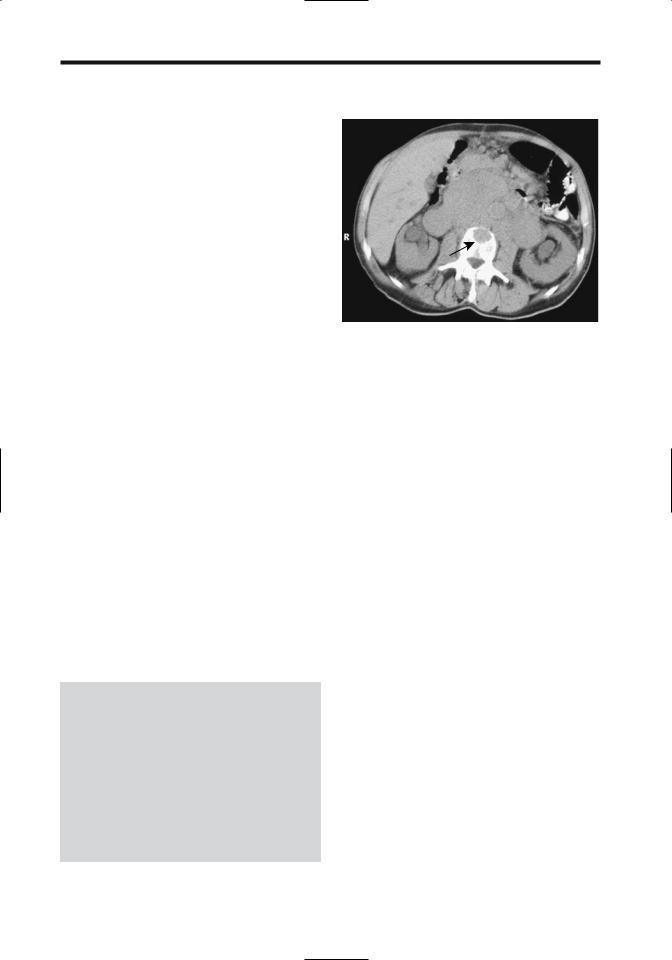







922
ADVANCED IMAGING OF THE ABDOMEN
|
B |
|
|
Figure 14.32. A: Abdominal wall hernia containing stomach. The |
|
|
gastric body and antrum extend anteriorly through a hiatus |
|
|
(arrow). B: Ventral hernia identified with CT (arrow). The hernia |
|
|
had been growing and an adenocarcinoma was found during |
|
|
hernia repair, believed to be secondary to a previously resected |
|
A |
colon cancer. |
|
wide hiatus. A barium study detects bowel |
others are detected with a small bowel barium |
|
herniation. |
study. A retrograde barium study through the |
|
These hernias are somewhat difficult to |
stoma is often helpful in outlining these hernias. |
|
repair because of their wide hiatus and because |
|
|
the surrounding structures tend to be weak. At |
|
|
times extraperitoneal fixation of a prosthetic |
Internal Hernia |
|
mesh to the 12th rib superiorly and iliac crest |
|
|
inferiorly is necessary. |
Patients with an internal hernia range from |
|
|
those who are asymptomatic, to those who have |
|
Sciatic Foramen Hernia |
intermittent nonspecific symptoms, to those |
|
|
who have small bowel obstruction. Especially |
|
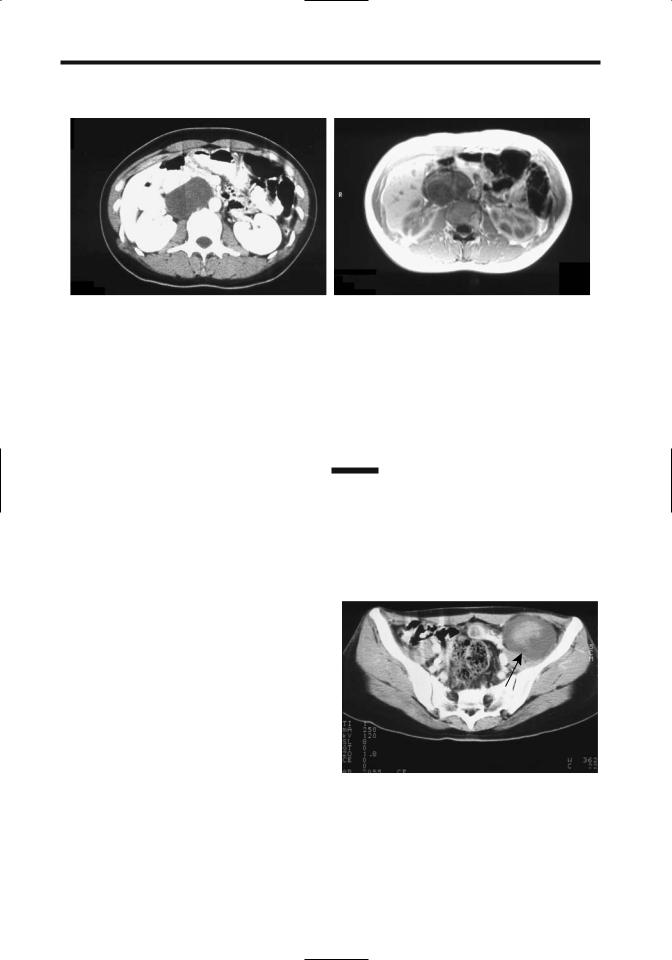
In a sciatic foramen hernia a loop of bowel or |
when intermittent, these hernias are difficult to |
|
adjacent tissue herniates through one of the |
diagnose with either barium studies or CT. |
|
sciatic foramina posteriorly. Bowel obstruction |
At times only a vague point of obstruction, |
|
and strangulation ensue. These hernias are |
either partial or complete, is identified with |
|
rare. |
imaging, but the etiology of obstruction is not |
|
Sciatic hernias are a cause of chronic pelvic |
evident. |
|
pain in women; most are left sided, and a rare |
Computed tomography findings of sympto- |
|
one can even contain an ovary and fallopian |
matic internal hernias consist of small bowel |
|
tube. Computed tomography or MRI should |
obstruction, a focal collection of dilated bowel |
|
identify the hernial content. |
displacing adjacent bowel, and stretched and |
|
|
displaced mesenteric vessels. |
|
Incisional Hernia |
Peritoneoceles and enteroceles are discussed |
|
|
in Chapter 5. Cystoceles are discussed in |
|
Either omentum or part of the stomach or bowel |
Chapter 11. |
|
can be part of an incisional hernia (Fig. 14.32). |
|
|
CT should detect these hernias, except that |
Transmesenteric Hernia |
|
some hernias reduce with the patient supine. A |
||
|
||
barium study detects herniation if it includes |
A transmesenteric hernia is the most common |
|
stomach or bowel. |
internal hernia. Although its appearance varies |
|
A parastomal hernia is a type of incisional |
considerably, the presence of dilated small |
|
hernia occurring alongside an intestinal stoma |
bowel loops close to the abdominal wall without |
|
on the abdominal wall. Some of these hernias |
overlying omental fat should suggest this diag- |
|
are evident on physical examination while |
nosis (73). Associated small bowel volvulus and |



 D
D B
B