
Книги по МРТ КТ на английском языке / Advanced Imaging of the Abdomen - Jovitas Skucas
.pdf
874
Mesenteric stranding, often in association with adjacent blood, suggests mesenteric injury, although laceration of an adjacent loop of bowel results in similar findings.
With rare exceptions, the presence of extraluminal gas (either pneumoperitoneum or extraperitoneal gas) is diagnostic of bowel perforation. Extraluminal gas is readily detected with both conventional radiography and CT. The inability to reliably and consistently detect a pneumoperitoneum is a limitation of US.
The small bowel normally contains little gas, and a number of bowel perforations manifest later as an intraabdominal abscess rather than as an immediate pneumoperitoneum. Colonic perforation, on the other hand, commonly results in a pneumoperitoneum, which is readily detected. Other indirect signs for perforation include intraperitoneal fluid, bowel wall thickening, bowel wall contrast enhancement, and bowel lumen dilation. None of the latter signs is specific for a perforation.
Bleeding
Bleeding leads to mesenteric or bowel hematomas, identified by CT as hazy streaking in mesenteric fat, or results in peritoneal or extraperitoneal fluid. Computed tomography scans of direct extravasation of IV contrast is evidence of active bleeding, and such bleeding in a setting of trauma is assumed to represent an injury to the involved viscera. Diffuse extravasation is implied by detecting extravasated contrast material, keeping in mind that extravasated contrast usually has a lower attenuation than the aorta. Not all intraor extraperitoneal bleeding is due to trauma; a ruptured aneurysm, a vessel weakened by tumor, anticoagulation therapy, or even venous obstruction and superimposed ischemia lead to bleeding and hematoma formation. Other rare causes of hemorrhage include severe pancreatitis or even an intraabdominal pregnancy.
Intraperitoneal blood pools in dependent spaces. Thus with upper abdominal bleeding a common site is Morison’s pouch and subphrenic spaces. More inferior locations include paracolic gutters and pouch of Douglas.
Computed tomography attenuation of intraperitoneal blood varies with age; initially it is isodense to intravascular blood. Hemoglobin concentration when blood clots, occurring
ADVANCED IMAGING OF THE ABDOMEN
within several hours, raises the attenuation to over 50 Hounsfield units (HU). Subsequent clot lysis, in a matter of days, gradually leads to an attenuation decrease, and in several weeks may approach the attenuation of water. Lower CT attenuation values are found in patients with preexisting anemia or if blood mixes with ascites or other fluid; thus fluid having a low attenuation does not exclude acute bleeding.
A hematoma often is not homogeneous in appearance. The rate of clot lysis in a hematoma varies, and a lower attenuation may be present at the periphery. Likewise, intermittent bleeding leads to simultaneous clotting and lysis and results in regions containing different attenuation values. If contrast-enhanced CT is performed during active arterial bleeding, the extravasating blood is isodense to adjacent arterial blood. Invariably an associated hematoma is present. A recent bleed can be denser than the rest of a hematoma, and such a sentinel clot tends to be located close to the site of bleeding.
At times nonhemorrhagic ascites also enhances with CT IV contrast.
The MR appearance of a hematoma (and intraperitoneal blood) also varies depending on clot age. Within a day or so of bleeding a hematoma is hypointense on both T1and T2weighted images. Then within several days it gradually becomes isointense to hyperintense on T1but remains hypointense on T2-weighted images. This prominent hypointensity on T2weighted images allows differentiation of blood from ascites, which is very hyperintense on T2weighted images. A pneumoperitoneum is also hypointense on T2-weighted images, but other MR sequences and the relative location of gas versus fluid in the peritoneal cavity allow differentiation. Within a week or so a hematoma becomes hyperintense on both T1and T2weighted images,but while evolving to this stage some hematomas reveal a hyperintense rim surrounding a hypointense central portion on T1weighted images. Eventually, if fibrosis develops around a prior hematoma, a hypointense rim on both T1and T2-weighted images encloses this region.
Diaphragmatic Injury
Diaphragmatic injury is one cause of visceral herniation into the chest. A majority of hemidiaphragmatic ruptures occur on the left side.

875
PERITONEUM, MESENTERY, AND EXTRAPERITONEAL SOFT TISSUES
Figure 14.2. Traumatic rupture of left hemidiaphragm. A scout view localizer prior to computed tomography (CT) reveals mediastinal shift to the right, partial left lung atelectasis and an elevated stomach. (Courtesy of Patrick Fultz, M.D., University of Rochester.)
The most common site for rupture is at the diaphragmatic dome, and the least common is at the rib muscular insertions (15). A number of these posttraumatic diaphragmatic ruptures are not initially apparent; herniation increases in size with time, and thus delayed imaging is nec-
essary. Some of these hernias are detected only months later. Intubation appears to hinder the detection of diaphragmatic rupture. Thus an initial chest radiograph or CT detects only about half of diaphragmatic ruptures (Fig. 14.2). These hernias became clinically symptomatic from days to years after trauma, and either conventional chest radiographs or upper gastrointestinal studies are diagnostic (Fig. 14.3). Strangulation of intestinal content has developed, including delayed gastric perforation into the pleural cavity.
A rare cause of diaphragmatic rupture is cardiopulmonary resuscitation.
Computed tomography detection sensitivities for diaphragmatic rupture are disappointing, especially for right hemidiaphragmatic rupture, and are of limited use; keep in mind that detection rates vary with time after trauma. Diaphragmatic crura are not thickened in patients with an injured diaphragm (16); coronal and sagittal reconstructions are also of limited value in detecting subtle diaphragmatic injury. Computed tomography usually does not reveal diaphragmatic discontinuity even with thin sectioning (except in the rare diaphragmatic avulsion); rather, intestinal content not confined by the diaphragm but spilling into the thorax is diagnostic of a hernia, and in the appropriate clinical setting provides indirect
A B
Figure 14.3. Traumatic left hemidiaphragm rupture. A: Chest radiograph reveals gas and fluid at the left lung base. B: A barium study performed through a nasogastric tube identifies part of the stomach in the chest. This study was performed several hours after that in part A, and now considerably more abdominal content has herniated into the chest.

876
evidence for diaphragmatic rupture. A waistlike intestinal constriction at the site of herniation is occasionally detected if rupture is limited in scope. These traumatic hernias need to be distinguished from congenital diaphragmatic hernias and from hernias through the esophageal hiatus.
Ultrasonography findings in patients with diaphragmatic rupture due to blunt trauma range from diaphragmatic disruption to a nonvisualized diaphragm. Occasionally detected is a diaphragm surrounded by fluid or abdominal content herniating through a diaphragmatic defect.
Preliminary reports suggest that MRI is reliable in detecting diaphragmatic injury; coronal and sagittal MRI reveal the site of a diaphragmatic tear and detect abdominal visceral herniating into the thorax, but keep in mind the limitation on early detection, as discussed previously.
Scintigraphy using intraperitoneally instilled Tc-99m–macroaggregated albumin (MAA) detects a diaphragmatic rupture but is rarely necessary.
Arecdotal reports describe spontaneous diaphragmatic rupture.
ADVANCED IMAGING OF THE ABDOMEN
requiring surgical intervention. Less common etiologies for an acute abdomen include lymphoma infiltrating the bowel and resulting in perforation, a perforating primary small bowel neoplasm, and a perforated bowel duplication cyst with spill of the contents into the peritoneal cavity.
In pediatrics, perforation is more common in neonates than in older children. Among neonates with gastrointestinal perforation, most common etiologies are necrotizing enterocolitis, isolated ileal perforations, a combination and sequella of malrotation/volvulus. Etiologic factors in children are trauma, Meckel’s diverticula complications, intussusception, pseudomembranous colitis, and post-operative complications.
In children, screening US detects an abdominal abnormality in about half of those with acute or subacute abdominal pain.
Past teaching has been to study an acute abdomen with conventional radiographs, an approach supplanted by CT, generally without IV contrast. At times images with and without IV contrast are useful (Fig. 14.4). Computed tomography has had a major impact in the diag-
Barotrauma
A pneumoperitoneum is a rare complication of mechanical ventilation. Detection of free gas in these generally rather sick patients leads to a diagnostic dilemma—Is the pneumoperitoneum secondary to an unsuspected bowel perforation? A number of these patients undergo surgical exploration.
Acute Abdomen
The causes of an acute abdomen are legion, including infection, bowel perforation, inflammation, obstruction, ischemia, volvulus of various structures, gynecologic abnormalities, and tumor infiltration; these conditions are discussed in their respective chapters. At times the first evidence of a serious underlying disease is an acute abdomen, such as Crohn’s disease manifesting as bowel perforation. Colonic epiploic appendagitis, a condition diagnosable by imaging, is an example of an acute abdomen not
Figure 14.4. Acute abdomen secondary to jejunal perforation. Oral and intravenous (IV) contrast-enhanced CT reveals ascites and pneumoperitoneum. Higher density material is present within this fluid adjacent the liver (arrow) and also in the left upper quadroon (curved arrow). Although angiography revealed patent vessels, surgery suggested emboli and ischemia for the patient’s perforation. (Courtesy of Patrick Fultz, M.D., University of Rochester.)

877
PERITONEUM, MESENTERY, AND EXTRAPERITONEAL SOFT TISSUES
nosis and subsequent management of patients presenting with an acute abdomen. Some studies suggest that CT is superior to clinical evaluation in diagnosing a cause for an acute abdomen. Such an approach appears to hold up regardless of the duration of signs and symptoms and in patients with no prior disease. Nevertheless, rather than use CT in a shotgun approach for all patients presenting with an acute abdomen, a more selective choice of imaging studies often establishes a diagnosis more quickly. For instance, with suspected cholecystitis, US should be the initial imaging modality; suspected acute uncomplicated pancreatitis generally requires little or no imaging, except possibly endoscopic retrograde cholangiopancreatography (ERCP), while pancreatic necrosis calls for contrast-enhanced CT or MR. Ultrasonography is more commonly employed in pediatric patients. CT is especially useful in obese patients, nondiagnostic US, or with suspected bowel obstruction.
In some centers US is used liberally for the initial study of patients with an acute abdomen. It is readily performed and detects a number of acute conditions. One limitation is the presence of dilated bowel. Also, while in experienced hands such diagnoses as appendicitis are readily made, a normal US examination does not exclude appendicitis, pyelonephritis, and other disorders. Likewise, early pancreatitis and bowel ischemia do not have specific US findings.
Laparoscopy is still preferred by some as a diagnostic and therapeutic modality in patients presenting with an acute abdomen. Even if conversion to an open laparotomy is necessary, laparoscopic findings are useful as a guide for the subsequent incision.
Infection/Inflammation
Abscess
Intraperitoneal
Clinical
Some abscesses develop spontaneously, although most are secondary to postoperative complications or spread from a source in an adjacent structure, such as diverticular disease, appendicitis, cholecystitis, and so on. Fluid collections communicating with bowel can become
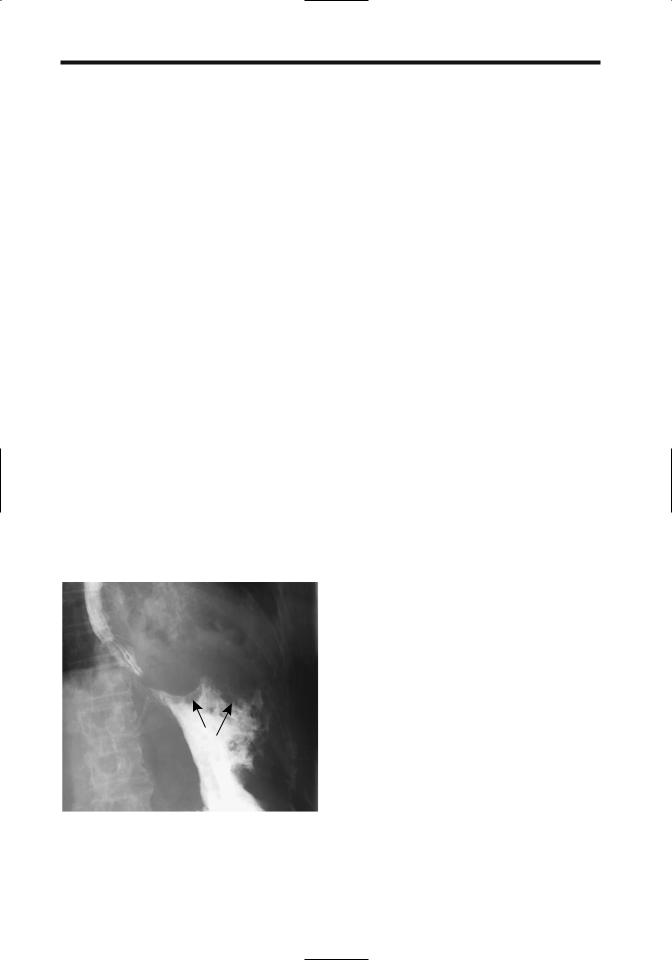
Figure 14.5. Postoperative abscess extending from the left hemidiaphragm inferiorly into left lower quadrant (arrows), communicating with the stomach. Barium sulfate was the contrast material used; it does not affect abscess healing.
huge, and patients have few symptoms due to the internal drainage (Fig. 14.5). At times an abscess and peritonitis coexist, and the initial inciting event is difficult to identify.
A gallstone falling into the peritoneal cavity during laparoscopic cholecystectomy may not be readily retrievable. Although many of these intraperitoneal gallstones are innocuous, they do serve as a potential nidus for abscess formation, with some of these abscesses manifesting years later. An occasional dropped appendicolith, occurring mostly during laparoscopic appendectomy, results in a similar finding. At times the specific etiology for such an abscess is suggested by CT or US.
Imaging
Computed tomography, US, MRI, or scintigraphy should detect and localize most intraabdominal abscesses, and most can then be drained percutaneously, generally under US guidance. Numerous comparison studies have shown CT and US accuracies of over 90% in detecting intraabdominal abscesses. Whether the greater resolution of CT or the greater portability of US determine the modality used, clinically the availability is the deciding factor.
878
A note about subphrenic abscesses. It is almost unheard of to have a subphrenic abscess without an associated pleural effusion. Even a chest radiograph should detect such an effusion, and the absence of effusion essentially excludes a subphrenic abscess. If imaging identifies a suspicious abscess beneath the right hemidiaphragm but no pleural effusion is detected, an intrahepatic rather than a subphrenic abscess is more likely.
Gas in a fluid collection generally implies an abscess,but gas bubbles are also seen in retained surgical sponges even without an abscess. Large amounts of gas suggest bowel communication, a finding seen with other benign and malignant conditions (Fig. 14.6).
Computed tomography of a typical abscess shows a fluid-filled structure surrounded by a contrast-enhancing rim. Such a finding is not limited to abscesses and is also seen with some necrotic tumors and other benign conditions such as a hematoma and various cystic structures. Also, not all abscesses have this appearance. Differentiation of an abscess and a benign fluid collection is difficult, especially if the wall is thick. Loculated fluid after abdominal surgery tends to develop primarily in the abdomen and
Figure 14.6. Left subphrenic abscess secondary to a perforated gastric fundal adenocarcinoma. The entire fundus is amputated by tumor and abscess (arrows). The study was performed primarily for unexplained weight loss.
ADVANCED IMAGING OF THE ABDOMEN
after pelvic surgery loculated fluid is mostly in the pelvis, but this is of limited use in differentiating benign fluid from an abscess.
Abscesses are hypointense on T1and hyperintense on T2-weighted MR images; about half are homogeneous in appearance. Gadoli- nium-enhanced T1-weighted fat-suppressed images identify abscesses as fluid collections surrounded by a contrast-enhancing rim. Gas within an abscess appears as a signal void on both T1and T2-weighted images. Coronal and sagittal reconstruction aids in differentiating an abscess from bowel. Fluid layering occurs in some abscesses, with hypointense material, presumably representing protein, being dependent on T2-weighted images, and such a finding in the peritoneal cavity is strong presumptive evidence of an abscess. Overall, MR sensitivity in detecting abscesses is close to 100%.
Scintigraphy detects most abdominal abscesses. Useful radiopharmaceuticals include gallium-67 citrate, indium-111 leukocytes, and Tc-99m leukocytes. A major limitation of Ga-67 citrate scintigraphy is the prolonged time required to perform the study.
Therapy
Percutaneous abdominal abscess drainage is an established technique, and almost all welldefined unilocular abscesses can be successfully drained. A majority of abscesses are cured with initial drainage. Recurrent abscesses can be drained percutaneously in most patients and surgery avoided in about half (17). Complex abscesses consisting of loculated, poorly confined, or multiple abscesses or those associated with a fistula have a lower success rate and often require several drains. A single abscess is often drained using US guidance, but multiple abscesses are easier to drain with CT guidance. Distinguishing an abscess from necrotic tissue can be difficult. At times aspirate cytology is helpful. Similar to surgical drainage, attempts to drain infected necrotic tumors percutaneously are rarely successful. Conversion to surgical drainage (and often associated resection) is required with the presence of unhealing abscesses or fistulas and bowel or pancreatic necrosis. Catheter-induced bleeding is an occasional complication requiring surgical correction.

879
PERITONEUM, MESENTERY, AND EXTRAPERITONEAL SOFT TISSUES
Crohn’s disease abscesses can be drained percutaneously using image guidance, and the patient is thus stabilized. These abscesses tend not to resolve completely, especially if they involve an enteric fistula.
Some left subphrenic abscesses cannot be readily drained using a transabdominal approach, and a transpleural approach is necessary. At times a drainage catheter is inserted through the pleura. Regardless of catheter position, most abscesses are successfully drained, although a transpleural approach risks a pneumothorax, requiring its own therapy.
Abscess drainage using a transrectal or transvaginal approach with a combination of endoluminal US and fluoroscopy for needle advancement, tract dilation, and catheter insertion, combined with appropriate antibiotics, is effective therapy for most pelvic abscesses. Patients undergoing transrectal aspiration or drainage have less procedure-related pain and catheter pain than those with a transvaginal approach (18). A viable option for some pelvic abscesses is US-guided transperineal catheter drainage.
Pelvic abscesses are readily drained in children and adolescents. The average hospital stay for children after image-guided transrectal drainage of pelvic abscesses tends to be shorter than after open surgical drainage. Surgical drainage is associated with more complications than percutaneous drainage, but comparison studies often have a built-in bias against surgery—patients undergoing surgical drainage tend to be sicker.
Computed tomography–guided transgluteal percutaneous drainage of deep pelvic abscesses through the greater sciatic foramen is an option in both adults and children (19).
A majority of vancomycin-resistant enterococcal abscesses can be drained percutaneously, although the rate of successful therapy is lower than with more conventional abscesses (20); at times drainage provides a first clue to the presence of vancomycin-resistant enterococci.
Abdominal Wall Abscess
Occasionally diverticulitis or cholecystitis evolves into an abdominal wall abscess. Likewise, an occasional biliary or other neoplasm leads to an abdominal wall abscess. Imaging
readily differentiates those abscesses involving the rectus abdominis muscle from intraabdominal conditions.
Psoas Muscle Abscess
An abnormal fluid collection in the psoas muscle region most often is an abscess, and less often a hematoma. In a setting of pancreatitis, a pseudocyst is also in the differential. A primary iliopsoas abscess is not common; a number of these occur in IV drug users and those positive for human immunodeficiency virus. More often these abscesses develop from a gastrointestinal, genitourinary, or spinal source. Some retroperitoneal abscesses involve not only the psoas muscles but also spread along soft tissue planes into adjacent compartments. Psoas abscesses develop in Crohn’s patients with disease.
Gram stain and a culture of the abscess contents should establish the responsible organism. Blood cultures are less often helpful. Both grampositive and gram-negative organisms are involved. In some parts of the world a tuberculous psoas abscess is more common than a pyogenic abscess; a tuberculous abscess tends to involve the adjacent vertebrae. Tuberculous psoas abscesses can be successfully drained percutaneously, although abscess recurrence often requires repeat drainage.
The clinical triad of fever, flank or thigh pain, and limitation of hip movement is found only in about half or fewer patients with a psoas abscess. Sepsis is common.
Computed tomography readily detects psoas abscesses; however, differentiation from a tumor purely on CT criteria is problematic (Fig. 14.7). A hematoma is also often in the differential. Image-guided needle aspiration should be diagnostic and percutaneous catheter drainage therapeutic.
Magnetic resonance imaging is very useful in evaluating psoas muscles. Normal psoas muscle is hypointense on T2-weighted images, while abscesses and the occasional psoas muscle tumor are hyperintense. Contrast-enhanced MR of a psoas abscess reveals a signal void surrounded by intense enhancement.
Conventional therapy of these abscesses is surgical drainage, although percutaneous drainage using CT or US guidance is becoming

880
ADVANCED IMAGING OF THE ABDOMEN
Figure 14.7. Psoas abscess. Transverse CT image reveals an enlarged, mostly hypodense right psoas muscle (arrow) displacing kidney anterior. (Source: Paley M, Sidhu PS, Evans RA, Karani JB. Retroperitoneal collections—aetiology and radiological implications. Clin Radiol 1997;52:290–294, with permission from the Royal Collage of Radiologists.)
more common. In distinction to intraabdominal abscesses, surgical psoas abscess drainage appears to result in a shorter patient hospitalization than with percutaneous drainage. On the other hand, serious complications are more common after surgical drainage than after percutaneous drainage (21). Imaging confirms abscess resolution.
Peritonitis
Peritonitis either is primary or develops secondary to an infected adjacent structure. It ranges from localized to diffuse. In the elderly, peritonitis tends to manifest initially in a more advanced or severe form than in a younger patient. At times both peritonitis and ascites coexist. Conditions presenting primarily with ascites are discussed in a later section.
Gastrointestinal perforation is a common cause of acute peritonitis and occurs both in the very young and very old. Peritonitis can develop after inadvertent gallbladder puncture during a liver biopsy or percutaneous nephrostomy. Occasionally encountered is aseptic peritonitis, usually in association with a peritoneal malignancy.
Primary peritonitis is rare in children, but more common in girls. Some of these
children are clinically suspected to have appendicitis, and the diagnosis is made only during surgery.
Imaging has a limited role in detecting acute peritonitis. Some degree of ascites is common. Contrast-enhanced CT and MR reveal increased peritoneal enhancement.
Infectious Peritonitis
Discussed here are only some of the more unusual organisms associated with infectious peritonitis.
Patients undergoing peritoneal dialysis are at increased risk of cryptococcal peritonitis. Cryptococcal peritonitis also occurs in patients with cirrhosis and end-stage renal disease.
Listeria is a rare cause of spontaneous bacterial peritonitis. About two thirds of reported patients have chronic liver disease or an underlying malignancy, or the patient was undergoing peritoneal dialysis.
Actinomycosis is a chronic infection by an anaerobic gram-positive commensal bacterium present in body orifices. Typically involved are the genitourinary tract and occasionally bowel. Rarely, it involves the peritoneum or greater omentum. Needle biopsies do not always provide a diagnosis; at times only inflammatory tissue is obtained and only an open biopsy provides the organisms.
Fitz-Hugh–Curtis syndrome, or venereal perihepatitis, is a complication of genital gonococcal or chlamydial infection. In Europe and the United States infection by Chlamydia trachomatis is more frequent. A majority of patients are women. Clinically, acute right upper quadrant symptoms mimic those of biliary disease, but liver function tests are normal. Likewise, US of the gallbladder and bile ducts is normal yet gallbladder wall thickening develops in some and multislice CT can detect transient liver attenuation abnormalities (22). Pathologically, perihepatitis consists of adhesions and peritoneal inflammation. Perihepatic fluid is often present. A biopsy should be diagnostic. The diagnosis is confirmed by finding Neisseria gonorrhoeae or
C. trachomatis organisms in perihepatic tissues. Some of these patients have undergone laparoscopy before the true diagnosis is suspected.
A rare cause of peritonitis is acute ascaris peritonitis due to bowel perforation. This con-

881
PERITONEUM, MESENTERY, AND EXTRAPERITONEAL SOFT TISSUES
dition, more common in children and occurring mostly in China, has a high mortality; on a more chronic basis, ascaris peritonitis leads to peritoneal granuloma formation.
Vernix Caseosa–Induced Peritonitis
An occasional woman develops unexplained abdominal pain after a cesarean section. An exploratory laparotomy reveals an organizing peritonitis, which includes a foreign-body granulomatous reaction. It is believed that this peritonitis most likely is induced by spillage of keratinous material (vernix caseosa) derived from amniotic fluid during the cesarean section.
In Cirrhosis
Most spontaneous bacterial peritonitis is encountered in patients with cirrhosis and ascites. Antecedent gastrointestinal bleeding is common in these patients. The clinical presentation is often subtle, and thus evaluation of ascitic fluid should be performed promptly, realizing that ascitic fluid culture is positive only in about half. Most common organisms involved are Enterobacteriaceae species and Gram positive cocci. Detection of these and other, less common infectious agents should lead to a search for either underlying cirrhosis or AIDS. Rarely, Streptococcus pneumoniae results in primary peritonitis without underlying disease.
Lupus
Acute lupus peritonitis is a rare manifestation of systemic lupus erythematosus. Imaging detects marked bowel wall thickening, intraluminal fluid, and ascites.
Meconium
Meconium peritonitis is a result of intra-utero bowel perforation, spill of meconium, and a resultant sterile chemical peritonitis. These perforations are often associated with congenital bowel obstruction such as small bowel atresia, volvulus, or meconium ileus. At times peritoni- tis-induced adhesions result in further obstruction. Although usually considered a benign condition, meconium peritonitis can be associated with infarcts secondary to intravascular dissemination of meconium emboli. Meconium
in the peritoneal cavity induces an exuberant fibrosis,leading to a multiseptate ascites appearance, which eventually calcifies. In some infants these calcifications are detected as an incidental finding, with the intra-utero bowel perforation having healed.
Imaging shows characteristic calcifications in the peritoneal cavity. These calcifications can extend into the scrotum through an intact processus vaginalis. Ultrasonography identifies these calcifications as hyperechoic linear or irregular abdominal foci, suggesting a cystic appearance.
Sclerosing Peritonitis/Mesenteritis
Clinical
Some authors treat mesenteritis and sclerosing peritonitis as separate entities, although recent thought suggests that these represent different manifestations of the same condition—an acute form (generally a mesenteritis or panniculitis) and a chronic form (often called sclerosing peritonitis). Diffuse mesenteric infiltration consists of inflammation (mesenteritis and panniculitis), fatty dystrophy, fluid, neoplasms, fibrosis, or even amyloid. Some patients develop a combination of inflammation, fatty dystrophy, and fibrosis, although usually one of these predominates. The terminology for this condition(s) is inconsistent and includes mesenteric panniculitis, mesenteric fibromatosis, retractile mesenteritis, sclerosing mesenteritis, mesenteric lipodystrophy, mesenteric WeberChristian disease, and inflammatory pseudotumor. The terms mesenteritis and sclerosing peritonitis are used here only for description of the primary sites involved. In some patients a sclerosing peritonitis appearance develops during peritoneal dialysis or use of certain drugs, such as practolol and beta-blocking agents. Occasionally mesenteritis is associated with estrogen use. Interestingly, retractile mesenteritis has resolved with progesterone therapy. Intraperitoneal hemorrhage is suggested as a possible link in forming sclerosing peritonitis. The older literature ascribed this condition in some patients to chronic repetitive abdominal trauma caused by vibrations of a pneumatic jackhammer. Mesenteritis has developed in a setting of Crohn’s disease, realizing that the clinical and radiologic features of both

882
are similar. A role for ischemia is occasionally postulated. Its relationship to extraperitoneal fibrosis (discussed below) is uncertain. Retractile mesenteric is associated with a number of neoplasms and immunosuppression therapy. Numerous reports describe sclerosing peritonitis developing in association with a luteinizing thecoma. A rare association exists between retractile mesenteritis and a mesothelioma.
Excessive fatty infiltration of the mesentery, or lipomatosis, may be idiopathic, part of generalized obesity, or associated with steroid therapy. Most lipomatosis is diffuse and tends to infiltrate rather than displace adjacent structures. It is the occasional focal collections of fat that suggest a fat-containing neoplasm in the differential diagnosis.
Mesenteritis presents either as an acute abdomen or, more often, evolves as a chronic condition of diffuse abdominal pain, at times intermittent. Large fibrofatty tumors develop in the abdomen. Histology reveals a fibrofatty infiltrate containing inflammation, fat necrosis, and fibrosis. Multiple mesenteric lymphatic cysts develop in this entity. Mesenteric fat necrosis, or lipodystrophy, also occurs with pancreatitis and some infections. Mesenteric infiltration has led to a protein-losing enteropathy; in fact, enteropathy can be the first manifestation of this condition.
Exuberant small bowel mesenteric fibrosis predominates in some individuals. This variant, often called retractile mesenteritis, also leads to some degree of inflammation, but the primary finding is mesenteric foreshortening and resultant mesenteric and small bowel distortion. Less often the mesocolon or sigmoid mesentery are affected. Normally little omental involvement is found. Rarely, a similar inflammatory process involves primarily the omentum rather than mesentery.
The differential diagnosis of retractile mesenteritis includes mesenteric and other peritoneal neoplasms. In some patients an open biopsy is necessary for diagnosis and to exclude a malignancy.
Imaging
Usually the small bowel mesentery is involved and ranges from a diffuse infiltrate, a focal soft tissue tumor, to discrete inflammatory nodules. The infiltrate typically also involves adjacent small bowel and results in a spiculated, irregu-
ADVANCED IMAGING OF THE ABDOMEN
lar outline to contrast-filled bowel. Valvulae conniventes are thickened and distorted but not destroyed, thus differentiating this condition from most malignant infiltrations. At times the appearance mimics Crohn’s disease, which also results in mesenteric inflammation and fibrosis. Occasionally mesenteric calcifications develop, probably within necrotic tissue.
Primarily retractile mesenteritis and panniculitis have separate and distinct CT appearances (23): patients with retractile mesenteritis show a mostly homogeneous soft tissue infiltrate denser than fat that distorts bowel loops. Those with panniculitis have a heterogeneous fat-density infiltrate typically involving the mesenteric root but with preserved fat around the greater vessels (fat ring sign), and a loss of the usual sharp outline of enclosed arteries; at times soft-tissue nodules are evident.
Ultrasonography identifies hypoechoic mesenteric tumors, occasionally containing a cystic component.
Magnetic resonance of lipomatosis reveals a fat signal intensity with all imaging parameters. T1-weighted fat-suppressed SGE images are useful to confirm that a focal collection is indeed fat. T1-weighted images of panniculitis (inflammation) reveal hypointense stranding traversing the hyperintense fat.
Sclerosing peritonitis manifests by thickening of the peritoneal lining, diffuse or loculated fluid collections, peritonitis and resultant small bowel obstruction, or simply disordered small bowel motility. Dense adhesions develop. Extensive fibrosis can involve the liver capsule. Peritoneal calcifications develop eventually. Imaging of patients on chronic ambulatory peritoneal dialysis and sclerosing peritonitis detects peritoneal thickening and calcifications; most also have loculated fluid collections and small bowel tethering or dilation.
Aside from calcifications, the imaging appearance of sclerosing peritonitis is similar to that of ovarian carcinoma with carcinomatosis. Both tend to develop adnexal tumors. In carcinomatosis, however, only the peritoneal surface is involved and it has an irregular outline due to malignant nodules; in sclerosing peritonitis not only does the peritoneal thickening have a smooth outline, but also the small bowel and colon walls are thickened. The differential for sclerosing peritonitis also includes diffuse mesothelioma, some chronic infections, and primary and secondary amyloidosis.

883
PERITONEUM, MESENTERY, AND EXTRAPERITONEAL SOFT TISSUES
Abdominal Cocoon
An abdominal cocoon, also called sclerosing encapsulating peritonitis, is a descriptive term for a variant of sclerosing peritonitis consisting of the small bowel being encased by a membrane and displaced centrally. It is a rare condition. Associated soft tissue tumors are evident in some patients. It is not uncommon to see small bowel obstruction.
The etiology of this condition is unknown. Most reported patients have been from the tropics or subtropical zones, with only an occasional report from temperate zones. One group of patients consists of young adolescent girls. Another group includes cirrhotic patients treated with a peritoneovenous shunt for ascites; autopsy in some of these patients simply identifies generalized peritoneal fibrosis. It has developed in a liver transplant recipient (24). A diagnosis of an abdominal cocoon as a separate entity probably is not appropriate if an infectious organism is recognized; peritoneal tuberculosis has resulted in a similar appearance, and this diagnosis should be excluded if an idiopathic abdominal cocoon is encountered.
Once established, a barium small bowel study is diagnostic. Occasionally, a barium study shows the small bowel to have a cauliflower-like configuration. Computed tomography reveals most or all of the small bowel encased by a thick membrane. Obstruction tends to develop at the site where the proximal small bowel enters its cocoon. Superficially, the condition mimics a large paraduodenal hernia.
Tuberculosis
Clinical
An increasing prevalence is evident not only for pulmonary tuberculosis but also for its extrapulmonary manifestation. Isolated abdominal involvement is not uncommon in endemic regions. Fatigue, prolonged fever, weight loss, nonspecific bowel symptoms, and a chronic wasting illness are common clinical findings.An erroneous initial diagnosis is common in parts of the world with a low prevalence of abdominal tuberculosis.
Hypercalcemia developed in patients with tuberculous peritonitis without pulmonary involvement. Elevated serum CA 125 tumor
marker levels are found in some of these patients; levels decrease after antituberculous therapy.
Tuberculosis ranges from disseminated disease to abdominal involvement only.Abdominal tuberculosis varies in organ involvement considerably, with ulcerative ileocecal involvement not uncommon. Peritonitis, mesenteric and extraperitoneal lymphadenopathy, and genitourinary involvement can occur as separate findings or together; multiorgan involvement, including ulcerative ileocecal involvement is not uncommon. Bowel perforation and obstruction lead to an acute abdomen. Presence vascular and perivascular granulomas, intraluminal thrombi and subintimal fibrosis suggest that bowel ischemia is a common pathway.
A diagnosis of peritoneal tuberculosis is difficult; in spite of clinical, endoscopic, and radiologic evaluation, peritoneal tuberculosis, especially if it involves the ileocecal region, is readily misdiagnosed as Crohn’s disease. Differentiating peritoneal tuberculosis from advanced ovarian cancer is difficult. Malignant lymphoma is also often in the differential diagnosis.
Tuberculous ascitic fluid acid-fast stains tend to be negative and not all Mycobacterium tuberculosis cultures are positive. Biopsy in some patients reveals epithelioid giant-cell granulomas containing caseous necrosis. At times diagnostic laparotomy and culture of tissue biopsy specimens are necessary for diagnosis.
Imaging
Imaging identifies intraand extraperitoneal lymphadenopathy. At times these enlarged nodes are focal in location and mimic a malignancy. Nevertheless, CT lymph node location and specific node appearance provide clues aiding the differentiation of these two entities.
Tuberculosis tends to involve more superior para-aortic lymph nodes, while lymphoma more often involves the inferior para-aortic lymph nodes (25). An exception is with disseminated tuberculosis, which affects nodes diffusely and involves the hepatoduodenal and hepatogastric ligaments and mesenteric and extraperitoneal lymph nodes; nondisseminated tuberculosis can involve similar node chains, except the inferior extraperitoneal lymph nodes are mostly spared. The large, confluent lymph nodes found in lym-
