
- •Contents
- •Preface to the Third Edition
- •About the Authors
- •How to Use Herbal Medicines
- •Introduction
- •General References
- •Agnus Castus
- •Agrimony
- •Alfalfa
- •Aloe Vera
- •Aloes
- •Angelica
- •Aniseed
- •Apricot
- •Arnica
- •Artichoke
- •Asafoetida
- •Avens
- •Bayberry
- •Bilberry
- •Bloodroot
- •Blue Flag
- •Bogbean
- •Boldo
- •Boneset
- •Borage
- •Broom
- •Buchu
- •Burdock
- •Burnet
- •Butterbur
- •Calamus
- •Calendula
- •Capsicum
- •Cascara
- •Cassia
- •Cat’s Claw
- •Celandine, Greater
- •Celery
- •Centaury
- •Cereus
- •Chamomile, German
- •Chamomile, Roman
- •Chaparral
- •Cinnamon
- •Clivers
- •Clove
- •Cohosh, Black
- •Cohosh, Blue
- •Cola
- •Coltsfoot
- •Comfrey
- •Corn Silk
- •Couchgrass
- •Cowslip
- •Cranberry
- •Damiana
- •Dandelion
- •Devil’s Claw
- •Drosera
- •Echinacea
- •Elder
- •Elecampane
- •Ephedra
- •Eucalyptus
- •Euphorbia
- •Evening Primrose
- •Eyebright
- •False Unicorn
- •Fenugreek
- •Feverfew
- •Figwort
- •Frangula
- •Fucus
- •Fumitory
- •Garlic
- •Gentian
- •Ginger
- •Ginkgo
- •Ginseng, Eleutherococcus
- •Ginseng, Panax
- •Golden Seal
- •Gravel Root
- •Ground Ivy
- •Guaiacum
- •Hawthorn
- •Holy Thistle
- •Hops
- •Horehound, Black
- •Horehound, White
- •Horse-chestnut
- •Horseradish
- •Hydrangea
- •Hydrocotyle
- •Ispaghula
- •Jamaica Dogwood
- •Java Tea
- •Juniper
- •Kava
- •Lady’s Slipper
- •Lemon Verbena
- •Liferoot
- •Lime Flower
- •Liquorice
- •Lobelia
- •Marshmallow
- •Meadowsweet
- •Melissa
- •Milk Thistle
- •Mistletoe
- •Motherwort
- •Myrrh
- •Nettle
- •Parsley
- •Parsley Piert
- •Passionflower
- •Pennyroyal
- •Pilewort
- •Plantain
- •Pleurisy Root
- •Pokeroot
- •Poplar
- •Prickly Ash, Northern
- •Prickly Ash, Southern
- •Pulsatilla
- •Quassia
- •Queen’s Delight
- •Raspberry
- •Red Clover
- •Rhodiola
- •Rhubarb
- •Rosemary
- •Sage
- •Sarsaparilla
- •Sassafras
- •Saw Palmetto
- •Scullcap
- •Senega
- •Senna
- •Shepherd’s Purse
- •Skunk Cabbage
- •Slippery Elm
- •Squill
- •St John’s Wort
- •Stone Root
- •Tansy
- •Thyme
- •Uva-Ursi
- •Valerian
- •Vervain
- •Wild Carrot
- •Wild Lettuce
- •Willow
- •Witch Hazel
- •Yarrow
- •Yellow Dock
- •Yucca
- •1 Potential Drug–Herb Interactions
- •4 Preparations Directory
- •5 Suppliers Directory
- •Index

Coltsfoot
Summary and Pharmaceutical Comment
The majority of the traditional uses associated with coltsfoot can be attributed to the mucilage content. However, coltsfoot also contains toxic pyrrolizidine alkaloids albeit at a low concentration. The risk of exposure to low concentrations of unsaturated pyrrolizidine alkaloids is unclear although hepatotoxicity following prolonged exposure has been documented (see Comfrey). The regular or excessive consumption of coltsfoot, especially in the form of herbal teas, should therefore be avoided.
Species (Family)
Tussilago farfara L. (Asteraceae/Compositae)
Synonym(s)
Farfara
Part(s) Used
Flower, leaf
Pharmacopoeial and Other Monographs
BHC 1992(G6)
BHP 1983(G7)
Complete German Commission E(G3)
Martindale 35th edition(G85)
Legal Category (Licensed Products)
GSL(G37)
Constituents
The following is compiled from several sources, including General Reference G2.
Figure 1 Selected constituents of coltsfoot.
C
Acids Caffeic acid, caffeoyltartaric acid, ferulic acid, gallic acid, p-hydroxybenzoic acid, and tannic acid (phenolic); malic acid and tartaric acid (aliphatic).(1)
Alkaloids Pyrrolizidine-type. Senkirkine 0.015% and senecionine (minor) (unsaturated)(2, 3) and tussilagine (saturated).(4)
Carbohydrates Mucilage (water-soluble polysaccharides) 7–8% yielding various sugars following hydrolysis (e.g. arabinose, fructose, galactose, glucose, uronic acid and xylose); inulin (polysaccharide).(5)
Flavonoids Flavonols (e.g. kaempferol, quercetin) and their glycosides.(1)
Tannins Up to 17% (type unspecified).
Other constituents Bitter (glycoside), choline, paraffin (fatty acid), phytosterols (sitosterol, stigmasterol, taraxasterol), triterpene (amyrin), tussilagone (sesquiterpene)(6) and volatile oil.
Food Use
Coltsfoot is not commonly used as a food but it is listed by the Council of Europe as a source of natural food flavouring (category N4). This category indicates that although coltsfoot is permitted
for use as a food flavouring, there are insufficient data available for an assessment of toxicity to be made.(G16)
Herbal Use
Coltsfoot is stated to possess expectorant, antitussive, demulcent
and anticatarrhal properties. It has been used for asthma, bronchitis, laryngitis and pertussis.(G2, G7, G49, G64)
Dosage
Dosages for oral administration (adults) for traditional uses recommended in standard herbal reference texts are given below.
Dried herb 0.6–2.0 g by decoction three times daily.(G6)
Figure 2 Coltsfoot (Tussilago farfara).
185
186 Coltsfoot
C
Figure 3 Coltsfoot – dried drug substance (leaf).
Liquid extract 0.6–2.0 mL (1 : 1 in 25% alcohol) three times daily.(G7)
Tincture 2–8 mL (1 : 5 in 45% alcohol) three times daily.(G7)
Syrup 2–8 mL (liquid extract 1 : 4 in syrup) three times daily.(G7)
Pharmacological Actions
In vitro and animal studies
Antibacterial activity has been documented for coltsfoot against various Gram-negative bacteria including Staphylococcus aureus,
Proteus hauseri, Bordetella pertussis, Pseudomonas aeruginosa and Proteus vulgaris.(7–9)
Anti-inflammatory activity comparable to that of indometacin, determined in Selye's experimental chronic inflammation test, has been attributed to water-soluble polysaccharides in coltsfoot.(10) Weak acute anti-inflammatory activity has been reported for
coltsfoot when tested against carrageenan-induced rat paw oedema.(11, 12)
Platelet-activating factor (PAF) is known to be involved in various inflammatory, respiratory and cardiovascular disorders. The aggregating action of PAF is known to be weaker if intracellular concentrations of calcium are low. A sesquiterpene, L-652469, isolated from coltsfoot buds has been reported to be a weak inhibitor of both PAF receptor binding and calcium channel blocker binding to membrane vesicles.(13) This combination of actions was found to effectively block PAF-induced platelet aggregation. L-652469 was also found to be active orally, inhibiting PAF-induced rat paw oedema.(13) Interestingly, L- 652469 was reported to interact with the cardiac calcium channel blocker receptor complex (dihydropyridine receptor), but was also found to be a calcium channel blocker.(13)
Tussilagine has been reported to be a potent cardiovascular and respiratory stimulant.(6, 14) Dose-dependent pressor activity fol-
lowing intravenous injection has been observed in the cat, rat and dog.(14) The pressor effect is stated to be similar to that of
dopamine, but without tachyphylaxis. A significant stimulation of respiration was also observed.(6) Cardiovascular and respiratory effects are thought to be mediated by peripheral and central mechanisms, respectively.(6)
Clinical studies
There is a lack of clinical research assessing the effects of coltsfoot and rigorous randomised controlled clinical trials are required.
Side-effects, Toxicity
There is a lack of clinical safety and toxicity data for coltsfoot and further investigation of these aspects is required.
Coltsfoot has been reported to be phototoxic in guinea-pig skin.(15)
Pyrrolizidine alkaloids with an unsaturated pyrrolizidine nucleus are known to be hepatotoxic in both animals and humans (see Comfrey). Of the pyrrolizidine alkaloids documented for coltsfoot, senecionine and senkirkine are unsaturated. Chronic hepatotoxicity has been described in rats following the incorpora-
tion of coltsfoot into their diet at concentrations ranging from 4– 33%.(16) After 600 days, it was found that rats fed more than 4%
coltsfoot had developed hepatic tumours (haemangioendothelial sarcoma) while none were observed in the control group. Furthermore, histological changes associated with pyrrolizidine alkaloid toxicity, such as centrilobular necrosis of the liver and cirrhosis, were observed in many of the rats who had ingested coltsfoot but who had not developed tumours.(16) The hepatotoxicity of coltsfoot was attributed to senkirkine, which is present at a concentration of only 0.015%, thus highlighting the dangers associated with chronic exposure to low concentrations of pyrrolizidine alkaloids.
Newborn rats have been found to be more susceptible than weanlings to the hepatotoxic effects of senkirkine despite lacking the hepatic microsomal enzymes required for the formation of the toxic pyrrolic metabolites.(17) Fatal hepatic veno-occlusive disease has been documented in a newborn infant whose mother had regularly consumed a herbal tea during pregnancy.(18) Analysis of the herbal tea revealed the presence of 10 different plants including coltsfoot and a Senecio species (known source of pyrrolizidine alkaloids, see Liferoot). The mother exhibited no signs of hepatic damage, suggesting an increased sensitivity of the fetal liver to pyrrolizidine alkaloid toxicity.
Pre-blooming coltsfoot flowers are reported to contain the highest concentration of alkaloids.(3) Considerable loss of both senkirkine and senecionine has been observed upon prolonged storage of the dried plant material.(3) Senkirkine and senecionine are both easily extracted into hot water and, therefore, would presumably be ingested in a herbal tea prepared from the fresh plant.(3) A cup of tea prepared from 10 g pre-blooming flowers has been estimated to contain a maximum of 70 mg senecionine and 1.4 mg senkirkine. Tea from the young leaves or mature plant would presumably contain considerably lower concentrations of alkaloids.(3) These concentrations are not considered to represent a health hazard compared to the known hepatotoxicity of senecionine (intravenous LD50 64 mg/kg body weight, mice).(3) However, prolonged exposure to low concentrations of pyrrolizidine alkaloids has resulted in hepatotoxicity (see Comfrey).
Tussilagine LD50 (mice, intravenous injection) has been determined as 28.9 mg/kg.(14)
Contra-indications, Warnings
In view of the known pyrrolizidine alkaloid content, excessive or prolonged ingestion should be avoided. In particular, herbal teas containing coltsfoot should be avoided.
Drug interactions None documented. However, the potential for preparations of coltsfoot to interact with other medicines administered concurrently, particularly those with similar or opposing effects, should be considered. There is limited evidence from preclinical studies that tussilagine, a constituent of coltsfoot,

has pressor activity. However, the clinical significance of this, if any, is not known.
Pregnancy and lactation Coltsfoot should not be taken during pregnancy or lactation in view of the toxicity associated with the pyrrolizidine alkaloid constituents. Coltsfoot is reputed to be an abortifacient.(G30)
Preparations
Proprietary multi-ingredient preparations
Argentina: Arceligasol; Negacne. Czech Republic: Perospir; Species Pectorales Planta. Italy: Lozione Same Urto. Spain: Llantusil. UK: Antibron; Chesty Cough Relief.
References
1Didry N et al. Phenolic compounds from Tussilago farfara. Ann Pharm Fr 1980; 38: 237–241.
2 Culvenor CCJ et al. The occurrence of senkirkine in Tussilago farfara. Aust J Chem 1976; 29: 229–230.
3 Rosberger DF et al. The occurrence of senecione in Tussilago farfara.
Mitt Geb Lebensm Hyg 1981; 72: 432–436.
4 Röder E et al. Tussilagine – a new pyrrolizidine alkaloid from
Tussilago farfara. Planta Med 1981; 41: 99–102.
5Haaland E. Water-soluble polysaccharides from the leaves of
Tussilago farfara L. Acta Chem Scand 1969; 23: 2546–2548.
6Yi-Ping L, Wang Y-M. Evaluation of tussilagone: a cardiovascularrespiratory stimulant isolated from Chinese herbal medicine. Gen Pharmacol 1988; 19: 261–263.
Coltsfoot 187
7Didry N et al. Components and activity of Tussilago farfara. Ann Pharm Fr 1982; 40: 75–80.
8 Didry N, Pinkas M. Antibacterial activity of fresh leaves of Tussilago spp. Bull Soc Pharm (Lille) 1982; 38: 51–52.
9 Ieven M et al. Screening of higher plants for biological activities I. Antimicrobial activity. Planta Med 1979; 36: 311–321.
10 Engalycheva E-I et al. Anti-inflammatory activity of polysaccharides |
C |
|
|
obtained from Tussilago farfara L. Farmatsiya 1982; 31: 37–40. |
|
11Benoit PS et al. Biological and phytochemical evaluation of plants. XIV. Antiinflammatory evaluation of 163 species of plants. Lloydia 1976; 39: 160–171.
12Mascolo N et al. Biological screening of Italian medicinal plants for anti-inflammatory activity. Phytother Res 1987; 1: 28–31.
13Hwang S-B et al. L-652,469 – a dual receptor antagonist of platelet activating factor and dihydropyridines from Tussilago farfara L. Eur J Pharmacol 1987; 141: 269–281.
14Wang Y-M. Pharmacological studies of extracts of Tussilago farfara L. II Effects on the cardiovascular system. Acta Pharm Sin 1979; 5: 268– 276.
15Masaki H et al. Primary skin irritation and phototoxicity of plants extracts for cosmetic ingredients. J Soc Cosmet Chem Jpn 1984; 18: 47–49.
16Hirono I et al. Carcinogenic activity of coltsfoot, Tussilago farfara L. Gann 1976; 67: 125–129.
17Schoental R. Hepatotoxic activity of retrorsine, senkirkine and hydroxysenkirkine in newborn rats, and the role of epoxides in carcinogenesis by pyrrolizidine alkaloids and aflatoxins. Nature 1970; 227: 401–402.
18Roulet M et al Hepatic veno-occlusive disease in newborn infant of a woman drinking herbal tea. J Pediatr 1988; 112: 433–436.
Comfrey
C
Summary and Pharmaceutical Comment
Comfrey is characterised by its pyrrolizidine alkaloid constituents. The hepatotoxicity of these compounds is well known, and cases of human poisoning involving comfrey have been documented. Human hepatotoxicity with pyrrolizidine-containing plants is well documented, particularly following the ingestion of Crotalaria, Heliotropium and Senecio species. Comfrey has traditionally been used topically for treating wounds. Percutaneous absorption of pyrrolizidine alkaloids present in comfrey is reported to be low, although application of comfrey preparations to the broken skin should be avoided.
Licensed herbal products intended for internal use are not permitted to contain comfrey. The inclusion of comfrey in products intended for topical application is permitted, provided the preparation is only applied to the unbroken skin and that its use is restricted to ten days or less at any one time.
As a result of a 1993 report by the Committee on Toxicity of Chemicals in Food to the Food Advisory Committee and the Ministry of Agriculture, Fisheries and Food (UK), the health food trade voluntarily withdrew all products, such as tablets and capsules, and advice was issued that the root and leaves should be labelled with warnings against ingestion. It was considered that comfrey teas contained relatively low concentrations of pyrrolizidine alkaloids and did not need any warning labels.
Species (Family)
Symphytum officinale L. (Boraginaceae)
Synonym(s)
Symphytum Radix
Related species include Prickly Comfrey (Symphytum asperum), Quaker and Russian Comfrey (Symphytum uplandicum, hybrid of
S. officinale S. asperum)
Part(s) Used
Leaf, rhizome, root
Pharmacopoeial and Other Monographs
BHC 1992(G6)
BHP 1996(G9)
Complete German Commission E(G3)
Martindale 35th edition(G85)
Legal Category (Licensed Products)
GSL (external use only)(G37)
Constituents
The following is compiled from several sources, including General References G2 and G6.
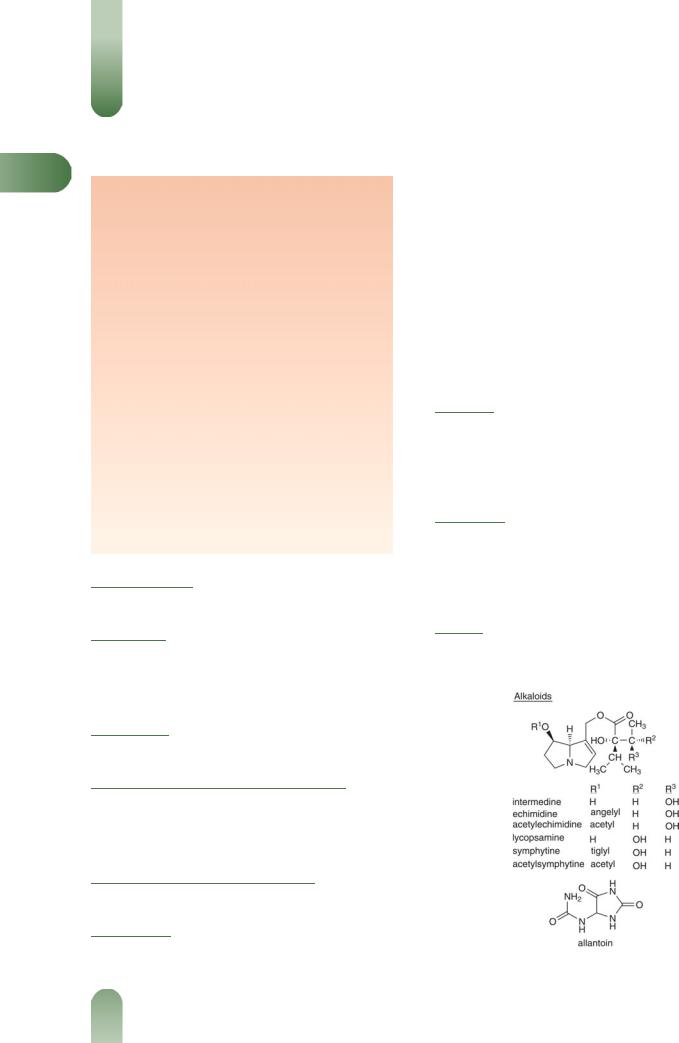
Alkaloids Pyrrolizidine-type. 0.3%. Symphytine, symlandine, echimidine, intermidine, lycopsamine, myoscorpine, acetyllycopsamine, acetylintermidine, lasiocarpine, heliosupine, viridiflorine and echiumine.(1–5)
Carbohydrates Gum (arabinose, glucuronic acid, mannose, rhamnose, xylose); mucilage (glucose, fructose).
Tannins Pyrocatechol-type. 2.4%.
Triterpenes Sitosterol and stigmasterol (phytosterols), steroidal saponins and isobauerenol.
Other constituents Allantoin 0.75–2.55%, caffeic acid, carotene 0.63%, chlorogenic acid, choline, lithospermic acid, rosmarinic acid and silicic acid.
Food Use
Comfrey is occasionally used as an ingredient of soups and salads. It is listed by the Council of Europe as natural source of food flavouring (category N4). This category indicates that although comfrey is permitted for use as a food flavouring, insufficient data are available to assess toxicity.(G16)
Herbal Use
Comfrey is stated to possess vulnerary, cell-proliferant, astringent, antihaemorrhagic and demulcent properties. It has been used for colitis, gastric and duodenal ulcers, haematemesis, and has been
applied topically for ulcers, wounds and fractures.(G2, G6, G7, G8,
G49, G64)
Dosage
Dosages for oral (unless otherwise stated) administration (adults) for traditional uses recommended in standard herbal reference texts are given below. Note: internal use is no longer advised.
Figure 1 Selected constituents of comfrey.
188
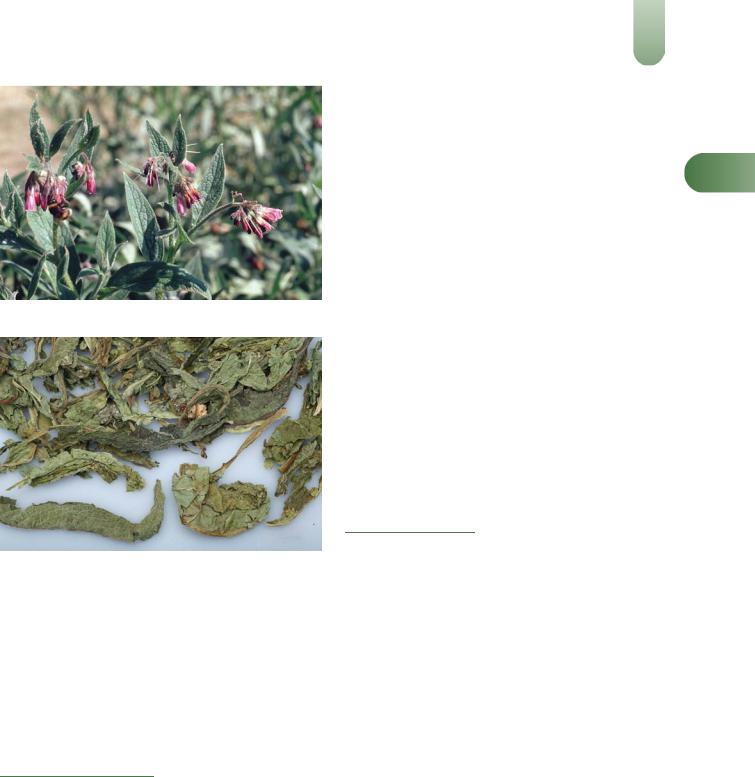
Figure 2 Comfrey (Symphytum officinale).
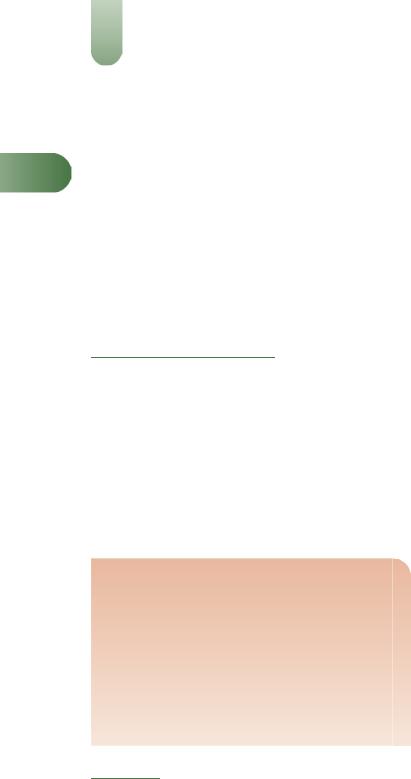
Figure 3 Comfrey – dried drug substance (leaf).
Dried root/rhizome 2–4 g as a decoction three times daily.(G7)
Root, liquid extract 2–4 mL (1 : 1 in 25% alcohol) three times daily.(G7)
Ointment symphytum root 10–15% root extractive in usual type ointment basis applied topically three times daily.(G7)
Dried leaf 2–8 g or by infusion three times daily.(G7)
Leaf, liquid extract 2–8 mL (1 : 1 in 25% alcohol) three times daily.(G7)
Pharmacological Actions
The classical pharmacology of pyrrolizidine alkaloids is overshadowed by the well-recognised toxicity of this class of compounds. Consequently, the majority of data documented for comfrey involve toxicity. Many useful reviews have been published
on the toxicity of pyrrolizidine alkaloids in humans (see below).(5–11)
In vitro and animal studies
Wound-healing and analgesic activities have been documented in rats administered comfrey extract orally.(12) Percutaneous absorption of pyrrolizidine alkaloids obtained from comfrey is reported to be low in rats, with minimal conversion of the pyrrolizidine alkaloid N-oxides to the free pyrrolizidine alkaloids in the urine
Comfrey |
189 |
|
(reduction of the N-oxides is required before they can be |
|
|
metabolised into the reactive pyrrolic esters).(13, 14) |
|
|
Rosmarinic acid has been isolated from comfrey (S. officinale) |
|
|
as the main constituent with in vitro anti-inflammatory |
|
|
activity.(15) Biological activity was determined by inhibition of |
|
|
malonic dialdehyde formation in human platelets. Minor |
C |
|
components, chlorogenic and caffeic acids, were not |
found to |
|
exhibit any significant activity. The pyrrolic esters have been reported to possess mild antimuscarinic activity, which is more pronounced in the non-hepatotoxic esters of saturated amino alcohols.(16) Conversely, the free amino alcohols are reported to exert indirect cholinomimetic action involving the release of acetylcholine from postganglionic sites in the guinea-pig ileum.(16)
Comfrey has been reported to stimulate the activity of the
hepatic drug-metabolising enzyme aminopyrine N-demethylase in rats.(17)
A comfrey extract has been reported to enhance uterine tone in vitro.(18) The action of comfrey was reported to be weaker than
that exhibited by German chamomile, calendula and plantain, but stronger than that shown by shepherd's purse, St. John's wort and uva-ursi.
Clinical studies
There is a lack of clinical research assessing the effects of comfrey and rigorous randomised controlled clinical trials are required.
The antimuscarinic properties of certain pyrrolic esters have been utilised. Two non-hepatotoxic pyrrolizidine alkaloids, sarracine and platyphylline, have been used for the treatment of gastrointestinal hypermotility and peptic ulceration.(16)
Side-effects, Toxicity
Two reports of human hepatotoxicity associated with the ingestion of comfrey have been documented.(19, 20) One case
involved a 13-year-old boy who had been given a comfrey root
preparation in conjunction with acupuncture to treat Crohn's disease. (19) The boy was diagnosed with veno-occlusive disease of
the liver and the authors concluded comfrey to be the only possible causal factor of the liver disease. The second case involved a 49-year-old woman diagnosed with veno-occlusive disease.(20) She had been taking various food supplements including a herbal tea and comfrey-pepsin pills. Pyrrolizidine alkaloids were identified in both the tea (stated to contain ginseng) and the comfrey-pepsin pills. The authors estimated that over a period of six months the woman had ingested 85 mg of pyrrolizidine alkaloids, equivalent to 15 mg/kg body weight per day. This report highlighted the potential toxicity associated with chronic ingestion of relatively small amounts of pyrrolizidine alkaloids.
The toxicity of pyrrolizidine alkaloids is well recognised. Pyrrolizidine alkaloids with an unsaturated pyrrolizidine nucleus are metabolised in the liver to toxic pyrrole metabolites.(8) Acute toxicity results in hepatic necrosis, whereas chronic toxicity typically results in veno-occlusive disease characterised by the presence of greatly enlarged liver cells.(8, 10)
Reports of human hepatotoxicity associated with pyrrolizidine alkaloid ingestion have been documented.(5, 8–10, 21–30) Many of these reports have resulted from crop (and subsequently flour and bread) contamination with Crotalaria, Heliotropium and Senecio species and from the use of pyrrolizidine-containing plants in medicinal 'bush' teas. In addition, pyrrolizidine alkaloid poisoning has been associated with the use of herbal teas in Europe and the United States.(20, 25–27) The diagnosis of veno-occlusive disease in a
190 Comfrey
newborn infant who subsequently died highlights the susceptibility of the fetus to pyrrolizidine alkaloid toxicity.(30) In this case, the mother had consumed a herbal tea as an expectorant during pregnancy. The tea, which was purchased from a pharmacy in Switzerland, was analysed and found to contain pyrrolizidine
C alkaloids. The mother did not exhibit any signs of hepatotoxicity.
Interestingly, liver function tests in 29 chronic comfrey users have been reported to show no abnormalities.(31)
The hepatotoxicity of pyrrolizidine alkaloids is well documen-
ted in animals.(5) In addition, carcinogenicity has been described in rats fed a diet supplemented with comfrey.(32) The mutagenicity
of comfrey has been attributed to lasiocarpine,(23) which is known to be mutagenic and carcinogenic. However, other workers have reported a lack of mutagenic activity for comfrey following assessment using direct bacterial test systems (Ames), host mediated assay (Legator), liver microsomal assay and the micronucleus technique.(33, 34)
Contra-indications, Warnings
In view of the hepatotoxic properties documented for the pyrrolizidine alkaloid constituents, comfrey should not be taken internally. The topical application of comfrey-containing preparations to broken skin should be avoided.
Drug interactions None documented. However, the potential for preparations of comfrey to interact with other medicines administered concurrently, particularly those with similar or opposing effects, should be considered.
Pregnancy and lactation The safety of comfrey has not been established. In view of the toxicity associated with the alkaloid constituents, comfrey should not be taken during pregnancy or lactation.
Preparations
Proprietary single-ingredient preparations
Austria: Traumaplant. Czech Republic: Traumaplant. Germany: Kytta-Plasma f; Kytta-Salbe f; Traumaplant. Switzerland: Kytta Pommade. Venezuela: Traumaplant.
Proprietary multi-ingredient preparations
Czech Republic: Dr Theiss Beinwell Salbe; Stomatosan. Germany: Kytta-Balsam f; Rhus-Rheuma-Gel N. Israel: Comfrey Plus. Switzerland: Gel a la consoude; Keppur; Keppur; Kytta Baume. USA: MSM with Glucosamine Creme.
References
1Culvenor CCJ et al. Structure and toxicity of the alkaloids of Russian comfrey (Symphytum uplandicum Nyman), a medicinal herb and
item of human diet. Experientia 1980; 36: 377–379.
2Smith LW, Culvenor CCJ. Hepatotoxic pyrrolizidine alkaloids. J Nat Prod 1981; 44: 129–152.
3Huizing HJ. Phytochemistry, systematics and biogenesis of pyrrolizidine alkaloids of Symphytum taxa. Pharm Weekbl (Sci) 1987;
9: 185–187.
4Mattocks AR. Toxic pyrrolizidine alkaloids in comfrey. Lancet 1980; ii: 1136–1137.
5Pyrrolizidine alkaloids. Environmental Health Criteria 80. Geneva: WHO, 1988.
6Abbott PJ. Comfrey: assessing the low-dose health risk. Med J Aust 1988; 149: 678–682.
7 Awang DVC. Comfrey. Can Pharm J 1987; 120: 101–104.
8McLean EK. The toxic actions of pyrrolizidine (Senecio) alkaloids. Pharmacol Rev 1970; 22: 429–483.
9 Huxtable RJ. Herbal teas and toxins: novel aspects of pyrrolizidine poisoning in the United States. Perspect Biol Med 1980; 24: 1–14.
10Mattocks AR. Chemistry and Toxicology of Pyrrolizidine Alkaloids. London: Academic Press, 1986.
11Jadhav SJ et al. Pyrrolizidine alkaloids: A review. J Food Sci Technol 1982; 19: 87–93.
12Goldman RS et al. Wound healing and analgesic effect of crude extracts of Symphytum officinale. Fitoterapia 1985; 6: 323–329.
13Brauchli J et al. Pyrrolizidine alkaloids from Symphytum offinale L. and their percutaneous absorption in rats. Experientia 1982; 38: 1085– 1087.
14Brauchli J et al. Pyrrolizidine alkaloids in Symphytum officinale L. and their dermal absorption in rats. Experientia 1981; 37: 667.
15Gracza L et al. Biochemical-pharmacological investigations of medicinal agents of plant origin, I: Isolation of rosmarinic acid from Symphytum officinale L. and its anti-inflammatory activity in an invitro model. Arch Pharm (Weinheim) 1985; 318: 1090–1095.
16Culvenor CCJ. Pyrrolizidine alkaloids: some aspects of the Australian involvement. Trends Pharmacol Sci 1985; 6: 18–22.
17Garrett BJ et al. Consumption of poisonous plants (Senecio jacobaea,
Symphytum officinale, Pteridium aquilinum, Hypericum perforatum) by rats: Chronic toxicity, mineral metabolism, and hepatic drugmetabolizing enzymes. Toxicol Lett 1982; 10: 183–188.
18Shipochliev T. Extracts from a group of medicinal plants enhancing the uterine tonus. Vet Med Nauki 1981; 18: 94–98.
19Weston CFM et al. Veno-occlusive disease of the liver secondary to ingestion of comfrey. Br Med J 1987; 295: 183.
20Ridker PM et al. Hepatic venocclusive disease associated with the consumption of pyrrolizidine-containing dietary supplements. Gastroenterology 1985; 88: 1050–1054.
21Anderson C. Comfrey toxicity in perspective. Lancet 1981; i: 944.
22Huxtable RJ et al. Toxicity of comfrey-pepsin preparations. N Engl J Med 1986; 315: 1095.
23Furmanowa M et al. Mutagenic effects of aqueous extracts of
Symphytum officinale L. and of its alkaloidal fractions. J Appl Toxicol
1983; 3: 127–130.
24Ridker PM, McDermott WV. Comfrey herb tea and hepatic venoocclusive disease. Lancet 1989; i: 657–658.
25Lyford CL et al. Hepatic veno-occlusive disease originating in Ecuador. Gastroenterology 1976; 70: 105–108.
26Kumana CR et al. Herbal tea induced hepatic veno-occlusive disease: quantification of toxic alkaloid exposure in adults. Gut 1985; 26: 101– 104.
27Stillman AE et al. Hepatic veno-occlusive disease due to pyrrolizidine (Senecio) poisoning in Arizona. Gastroenterology 1977; 73: 349–352.
28McGee JO'D et al. A case of veno-occlusive disease of the liver in Britain associated with herbal tea consumption. J Clin Pathol 1976;
29:788–794.
29Datta DV et al. Herbal medicines and veno-occlusive disease in India. Postgrad Med J 1978; 54: 511–515.
30Roulet M et al. Hepatic veno-occlusive disease in newborn infant of a woman drinking herbal tea. J Pediatr 1988; 112: 433–436.
31Anderson PC, McLean AEM. Comfrey and liver damage. Hum Toxicol 1989; 8: 55–74.
32Hirono I et al. Carcinogenic activity of Symphytum officinale. J Natl Cancer Inst 1978; 61: 865–869.
33Lim-Sylianco CY et al. Mutagenicity studies of aqueous extracts from leaves of comfrey (Symphytum officinale Linn). NRCP Res Bull 1977;
32:178–191.
34White RD et al. An evaluation of acetone extracts from six plants in the Ames mutagenicity test. Toxicol Lett 1983; 15: 23–31.
