
Учебники / Head_and_Neck_Cancer_Imaging
.pdf
Neoplasms of the Oral Cavity |
115 |
addition to the lips, any intraoral mucosal surface can be affected; however, three specific intraoral sites are predominantly affected. In descending frequency, the floor of the mouth, the retromolar trigone, and the ventrolateral tongue are involved (Mashberg and
Meyers 1976).
Small superficial T1 tumors are often not visible on both CT and MR images (Keberle et al. 1999). With increasing size, SCC infiltrate deeper submucosal structures. As a result, CT and MRI show a tumor mass and allow for an accurate evaluation of deep tumor infiltration (Kösling et al. 2000; Leslie et al. 1999). This results in the possibility of staging SCC of the oral cavity according to the TNM system (UICC 2002) (Table 6.2). In spite of the invasive character of SCC, bony structures and arteries resemble anatomic
Table 6.2. Squamous cell carcinoma of the oral cavity: T staging (UICC 2002)
T1 Tumor d 2 cm in greatest diameter
T2 Tumor > 2 cm but < 4 cm in greatest diameter
T3 Tumor t 4 cm in greatest diameter
T4a Oral cavity: Cortical bone, extrinsic muscles of the tongue, maxillary sinus, skin
Lips: Cortical bone, inferior alveolar nerve, floor of the mouth, skin
T4b Masticator space, pterygoid process, skull base, internal carotid artery
barriers and are infiltrated rather late in the course of the disease.
Regarding bony structures, cortical tumor infiltration can best be detected as erosion and/or lysis of the adjacent cortex on CT images with a bone-win- dow setting (van Den Brekel et al. 1998; Mukherji et al. 2001). A soft tissue mass within the bony marrow is a direct sign and can be seen on both CT and MR images. Especially, pre-contrast in combination with fat-saturated post-contrast T1-weighted MR images are very helpful to detect bone marrow invasion (Fig. 6.16).
Furthermore, an important aspect regarding malignancies of the oral cavity is the invasion of nerves and vessels of neurovascular bundles, such as in the sublingual space (Mukherji et al. 1996, Smoker 2003). Whereas vascular invasion yields a greater risk of remote as well as lymph node metastases, nerve involvement can lead to tumor extension along nerve routes (perineural extension) far beyond the expected tumor margins (compare Figs. 6.6 and 6.17). Perineural extension may be asymptomatic and is often not easy to detect with all imaging modalities. Therefore, perineural extension results in a greater likelihood of positive resection margins and/or remote tumor remnants. As a consequence, it is crucial to look for direct or indirect signs for perineural tumor extension. Direct signs are thickened (Fig. 6.17) and contrast-enhanced nerves. Indirect signs are
a |
b |
Fig. 6.16a,b. Pre-contrast (a) and post-contrast (b) T1-weighted axial MRI showing carcinomatous infiltration of the mandible. Erosion of the bony cortex (arrow). The post-contrast image differentiates between hypointense edema and hyperintense tumor infiltration (asterisk on b) of the bone marrow. (Courtesy of Bodo Kress, MD, Heidelberg, Germany)
116 |
M. Keberle |
a 
 b
b
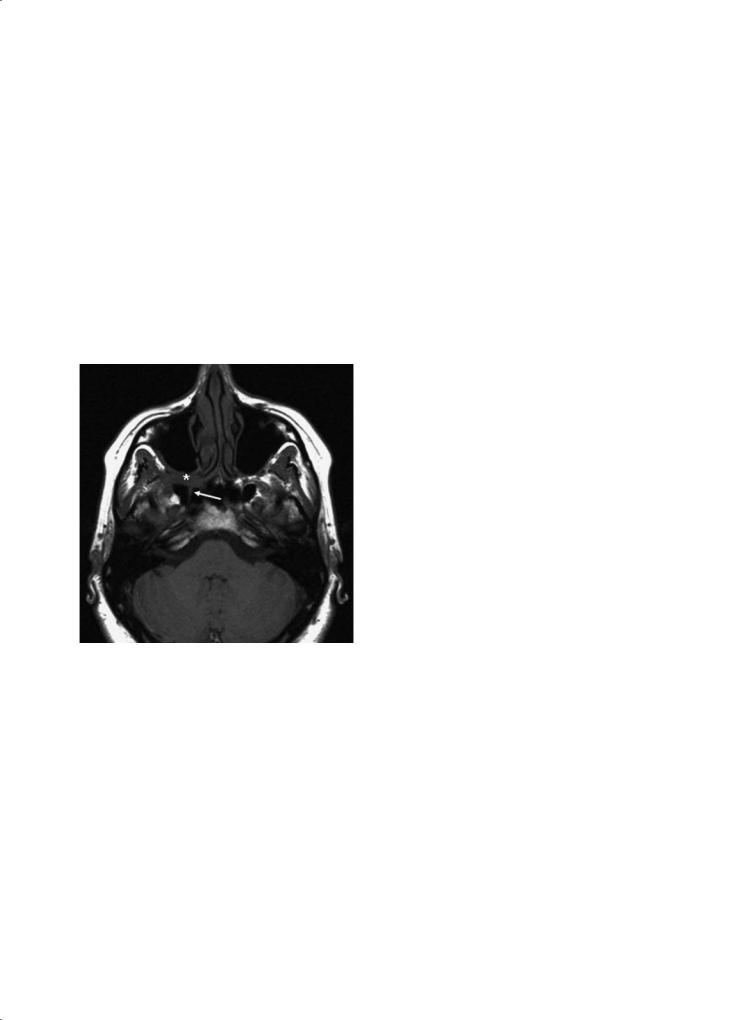
Fig. 6.17a–c. Axial pre-contrast T1-weighted MRI of an adenoid cystic carcinoma at the right maxillary alveolar ridge (a); the sig-
|
nal loss inside the bone represents medullar tumor infiltration. |
|
The patient complained of right-sided facial headache and an an- |
|
aesthesia of the palate, as a result of extensive perineural tumour |
|
spread. Accordingly, (b) shows soft tissue thickening in the region |
|
of the greater palatine canal containing the greater palatine nerve |
|
(arrow) and (c) shows tumor extension into the right pterygo- |
|
palatine fossa (asterisk) extending laterally in the infratemporal |
|
fossa, anterolaterally along the wall of the maxillary sinus, and |
|
posteriorly in the pterygoid (Vidian) canal (arrow). (Courtesy of |
c |
Robert Hermans, MD, PhD, Leuven, Belgium) |
invasion of sublingual space and widening of bony foramina or canals.
In general, SCC have a similar density to muscle on pre-contrast images (on both, CT and MR images) (Yasumotoetal.1995;Keberleetal.2002).Nonetheless, native T1-weighted MR images are of great value to delineate the tumor because the characteristic architecture of the tongue musculature is usually altered by the lesion. Furthermore, native T1-weighted images as well as post-contrast CT images yield the best contrast versus normal fat (e.g. the fatty tissue of the sublingual space).On T2 images,SCC are slightly hyperintense.On post-contrast images there is moderate enhancement, so that fat-saturated MR images have to be obtained. With increasing size, SCC (and respective metastases) often present with a central necrosis.
Cervical lymph node metastases occur in approximately 50% of the patients with SCC of the oral cavity (Magrin and Kowalski 2000; Smoker 2003). In tumors crossing the median (midline) there is often bilateral lymph node involvement. This holds especially true for tumors of the tongue. Lymph node involvement is generally accepted to be the single most important prognostic parameter (Magrin and Kowalski 2000). In addition to CT and MRI, ultrasound is known to be a very valuable tool regarding the detection and differentiation of cervical lymph nodes (see also Chap. 15).
In general, therapeutic options comprise surgery, radiation therapy, and chemotherapy. The latter is increasingly used as inductive chemotherapy in order to reduce the size of the tumor prior to surgery.
Neoplasms of the Oral Cavity |
117 |
Furthermore, surgery and radiation therapy are often combined. Clear extension beyond the midline in tongue cancer often precludes surgical resection as this would imply total glossectomy; primary radiation therapy is usually performed in such circumstances. Whereas smaller tumors can be removed with laser or classic surgery, larger tumors often re-
Fig. 6.18. CT in a 55-year-old pipe-smoking male with a squamous cell carcinoma of the lower lip. The contrast-enhancing mass is on both sides of the midline, the adjacent soft tissues are edematously swollen. In level II there are bilateral lymph node metastases with central necrosis
quire extensive surgery with tissue reconstruction. An additional invasion of the mandibular cortex requires marginal (cortical) mandibulectomy. Invasion of the mandibular marrow instead requires complete mandibular resection of the infiltrated segment (segmental mandibulectomy) with local reconstruction.
As a result there is a large variety of therapeutic options so that for any individual an exact evaluation of the tumor extension is essential.
6.3.2.2 Lip Cancer
As already mentioned, the lips are the most frequent location regarding SCC of the oral cavity (Fig. 6.18). However, only very large tumors require local evaluation of deep tumor extension by CT or MRI. In this regard, pretherapeutically important anatomic structures are the mandibular cortex, the mandibular marrow, and the inferior alveolar and/or mental nerves (for the imaging criteria of perineural and mandibular infiltration see Chap. 5).
6.3.2.3
Floor of the Mouth Cancer
Most tumors of the floor of the mouth originate in its anterior aspects. Here small superficial tumors are readily diagnosed by clinical means. In order to evaluate a tumor’s deep infiltration and for TN staging, cross-sectional imaging is needed (Figs. 6.19 and 6.20).
a |
b |
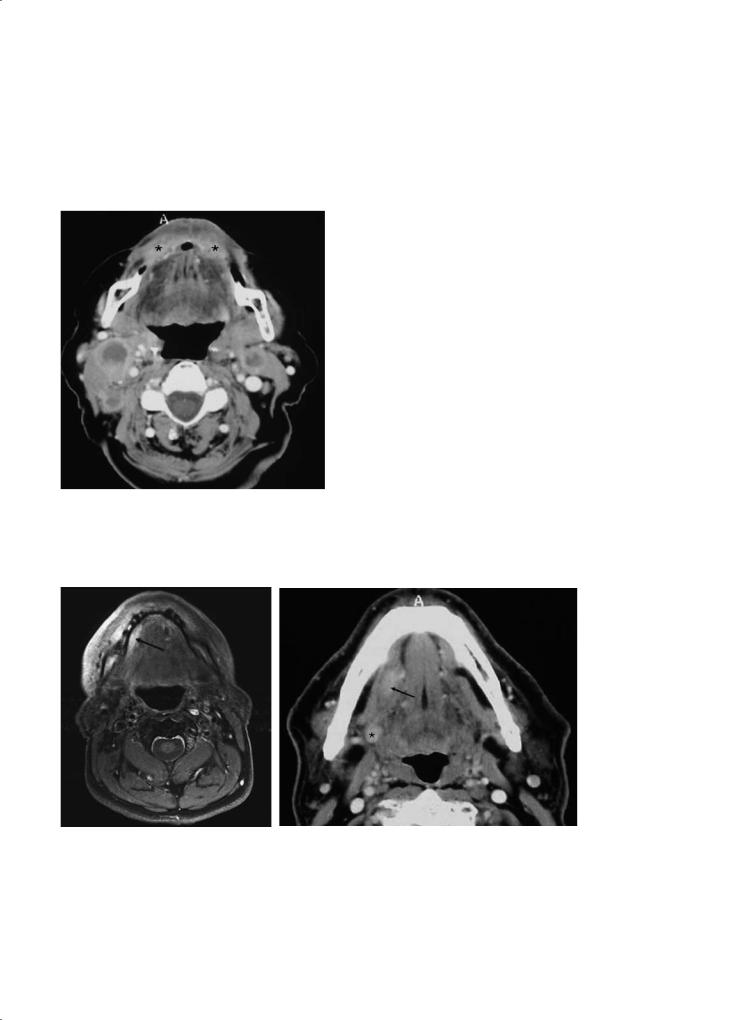
Fig. 6.19a,b. MRI of a 54-year-old man with a small T1 tumor (SCC) in the anterior part of the floor of the mouth (a). A fatsaturated axial T1-weighted MR image shows the small hyperintense mass adjacent to the attachment of the mylohyoid muscle at the inner mandibular surface. The cortex is intact. b A different patient (63-year-old male) presented with a squamous cell carcinoma of the right floor of the mouth. At CT, the small T1 tumor almost completely fills out the sublingual (fat) space and lies directly between the medially located ipsilateral neurovascular bundle (and hyoglossus muscle) and the laterally located mylohyoid muscle. A lymph node metastasis can be seen on the same slice (asterisk)

118 |
M. Keberle |
a |
b |
Fig. 6.20a,b. CT of a 62-year-old man with a squamous cell carcinoma lying more deeply in the floor of the mouth (a). The tumor is located between the mylohyoid muscle and the partially presented transverse (intrinsic) muscles of the tongue (cross). Note the bilateral lymph node metastases. Different patient (b) with a SCC with central necrosis on the left side of the floor of the mouth. At CT, the tumor (arrow) is located between the geniohyoid and the hyoglossus muscles. Note the ipsilateral lymph node metastasis with central necrosis
Considering the latter facts, in ultrasound, the transducer has to be tilted so that the anterior part of the floor of the mouth can be evaluated accordingly (Mende et al. 1996; Keberle et al. 2000). SCC of the floor of the mouth preferentially infiltrate the surrounding soft tissues first before the mandible and/or the mylohyoid muscle are invaded (Lenz and Hermans 1996). Medially, the tumor can cross the midline, invade the contralateral neurovascular bundle and if there is also cranial extension of the tumor the tongue can be involved.As previously mentioned, large tumor involvement of the contralateral tongue and/or neurovascular bundle often precludes radical surgical resection (Mukherji et al. 1997). Dorsally and caudally, SCC of the floor of the mouth can spread to deeper cervical tissues. Usually, it comes to a dorsal spread first along the mylohyoid muscle and the inner surface of the mandible which are natural borders. Dorsally, Wharton’s duct or the submandibular gland itself can be infiltrated.Both can result in inflammatory changes of the gland due to duct obstruction (Yousem et al. 2000). Enlargement of the submandibular gland and dilatation of the duct are important indirect tumor signs. On the other hand, oropharyngeal tumors at the base of the tongue tend to infiltrate the floor of the mouth ventrally (resulting in a T4-oropharyngeal
tumor if extrinsic muscles of the tongue are involved) (Fig. 6.21). The same tumor stage applies for oral cavity tumors in case of invasion of extrinsic muscles of the tongue and/or lateral (as well as anterior) infiltration of the mandible (Table 6.2). Interestingly, caudal infiltration of the mylohyoid muscle is not regarded a T4 stage according to UICC guidelines (Table 6.2). The coronal plane facilitates the evaluation of the mylohyoid as well as extrinsic tongue muscles (Lell et al. 1999).
Tumors of the anterior part of the floor of the mouth in particular result in submental (level I; best seen on coronal slices; Lell et al. 1999) and/or submandibular (also level I) lymph node metastases (Fig. 6.20a).
6.3.2.4
Retromolar Trigone Cancer
SCC of the retromolar trigone are localized in the superoposterior part of the oral cavity and often involve oropharyngeal subregions (Fig. 6.22). These tumors are rarer than tumors of the lips or of the floor of the mouth, however, they are more difficult to detect by clinical means. Dorsally, the cranial part of the tonsillar pillar, the lateral aspect of the soft palate, as well as the pharyngeal tonsil can be affected. Deeply, along

Neoplasms of the Oral Cavity |
119 |
a 
 b
b
Fig. 6.21a,b. CT of a 56-year-old man with an oropharyngeal (T4) squamous cell carcinoma of the base of the tongue and deep tumor infiltration into the geniohyoid and genioglossus muscles of the floor of the mouth (stars) and midline crossing (a). The corresponding ultrasound nicely shows the relation to the lingual artery (arrow, asterisks indicate the mylohyoid muscle on both sides)(b)
a |
b |
Fig. 6.22a,b. Axial CT (a) and axial T2-weighted MRI (b) of a male patient with squamous cell carcinoma of the right retromolar trigone (arrows) extending medially to the soft palate. The contrast-enhancing (a) mass is hyperintense on the T2-weighted MR image (b). (Courtesy of Sabrina Kösling, MD, Halle, Germany)
the pterygomandibular space, the mandible, superior pharyngeal constrictor muscle, the pterygoid processes, the medial pterygoid muscle (eventually causing trismus), and the masticator and the parapharyngeal spaces (and this way even the skull base) can be infiltrated. Especially, in the case of tumor extension into the pterygopalatine fossa, one always has to watch for perineural tumor spread (Mukherji et al. 1997). Ventrally and cranially, the gingival and/or buccal mucosa as well as the maxillary alveolar ridge (the latter being a T4 stage) are possibly infiltrated (Table 6.2). Medially, the tumor may extend towards the hard palate; laterally, the buccinator space can be infiltrated.
6.3.2.5 Tongue Cancer
The ventrolateral surface of the tongue is involved more often than the rest of the tongue (Fig. 6.23). These tumors easily invade the intrinsic muscles of the tongue. The floor of the mouth with the ipsilateral neurovascular bundle (Fig. 6.24), the base of the tongue, the gingival mucosa and eventually the oropharyngeal tonsils, the soft palate, and the mandible may become invaded. Again, it is crucial to evaluate tumor extension in relation to the midline and to the contralateral neurovascular bundle and sublingual space.

120 |
M. Keberle |
a 
 b
b
Fig. 6.23a,b. CT with axial (a) as well as coronal reformation (b) in a 49-year-old male with a T2 squamous cell carcinoma of the ventrolateral tongue. The tumor does not cross the midline and, thus can more easily be removed than the masses shown in Figs. 6.21 and 6.24 (e.g. by hemiglossectomy)
a 
 b
b
Fig. 6.24a,b. CT with coronal (a) and axial (b) reconstructions of a 60-year-old male with a huge squamous cell carcinoma of the tongue. The tumor extends into the floor of the mouth and reaches the mandible as well as the midline but without crossing it. The tumor shows a strong rim enhancement and appears to surround the ipsilateral neurovascular bundle. Beneath the mylohyoid muscle is a small submandibular lymph node metastasis (level I)
6.3.2.6
Hard Palate, Gingival and Buccal Cancer
Tumor location at the mucosal layer beneath the hard palate eventually implies close evaluation of the adjacent bone (Fig. 6.25). This can best be achieved on coronal MR or CT images (bone window). Furthermore, the incisive canal and the greater and lesser palatine canals have to be inspected closely for potential perineural tumor spread along the respective palatine
nerves (nerve V/2) towards the pterygopalatine fossa. Whereas CT can demonstrate asymmetric pathologic widenings (sometimes cortical erosions) of the respective bony canals, MRI superiorly displays perineural spread as thickening (Fig. 6.17) and/or contrast enhancement of the nerve.
SCC of the gingival or buccal mucosa may eventually invade the mandibular or maxillary cortex (Figs. 6.16 and 6.26), which is usually best seen on axial slices.

Neoplasms of the Oral Cavity |
121 |
a
a
b
Fig. 6.25a,b. Coronal MRI (post-contrast T1-weighted) |
|
in a 72-year-old male showing a mildly enhancing squa- |
|
mous cell carcinoma of the hard palate with infiltration |
b |
of bone and extension into the right maxillary sinus (a). b |
|
An adenoid cystic carcinoma in a 84-year-old female (fat- |
|
saturated T1-weighted post-contrast MRI) of the hard |
|
palate with severe extension into the maxillary sinus. |
|
Although adenoid cystic carcinoma is often associated |
|
with perineural infiltration, this patient did not present |
|
with the latter form of tumor spread |
|
Fig. 6.26a–c. Axial MRI in a 60-year-old female with a swollen |
|
cheek and histologically proven squamous cell carcinoma of the |
|
gingival mucosa at the level of the left-sided 7th and 8th maxillary |
|
molar teeth. Isointense mass on native T1 (a), hyperintense mass |
|
on T2 (b), and homogeneously enhancing hyperintense mass on |
|
fat-saturated post-contrast T1 (c). The adjacent maxillary cortex |
|
is not invaded. The tumor grows behind the 8th molar into the |
|
region of the retromolar trigone. (Courtesy of Nicole Freling, |
|
MD, Amsterdam, The Netherlands) |
c |

122 |
M. Keberle |
6.3.3
Other Malignant Tumors
6.3.3.1
Adenoid Cystic Carcinoma
Malignant tumors other than SCC are quite rare. Adenoid cystic carcinoma (ACC) originates from the minor salivary glands which can be found ev-
erywhere in the oral cavity (Figs. 6.17, 6.25b, and 6.27) (Cawson 1998). They usually occur in the fifth to seventh decade of life,men and women are affected about equally. The long term prognosis is worse in comparison to SCC (Friedman et al. 1986). This is mainly due to the propensity of adenoid cystic carcinoma for perineural tumor spread and deep local invasion (Sigal et al. 1992; Parker and Harnsberger 1991). On the other hand, lymphatic metastases are much
a |
b |
c 
 d
d
Fig. 6.27a–d. MRI of a 56-year-old female with a short history of dysphagia. Axial T2- (a) and post-contrast T1-weighted (b) images of an irregular, slightly inhomogeneous hyperintense adenoid cystic carcinoma of the tongue which infiltrates the floor of the mouth and clearly crosses the midline. Thus, there were no surgical options. Sagittal T2- (c) and post-contrast T1-weighted (d) images better show the entire longitudinal and sagittal extension of the tumor. Posteriorly, the tumor infiltrates the base of the tongue. (Courtesy of Nicole Freling, MD, Amsterdam, The Netherlands)

Neoplasms of the Oral Cavity |
123 |
rarer than in SCC, but hematogenous spread, mainly to the lungs and liver, does occur. Perineural invasion mainly affects the maxillary (V2) and/or the mandibular (V3) nerves. To avoid underestimation of tumor spread, in this regard, the latter nerves, the pterygopalatine fossa (V2), the foramen rotundum (V2), the pterygoid canal (canal containing mixed paraand orthosympathic nerve entering the pterygopalatine canal), the foramen ovale (V3), and the cavernous sinus have to be inspected thoroughly. It is important to note that in some cases of ACC tumor-free areas (“skip areas”) along the nerves have been reported. On CT images, perineural spread might be identified by enlargement of skull base foramina, whereas enlarged nerves are usually not directly visualized. On MR images, perineural tumor spread can directly be visualized as an enlarged nerve with a varying extent of contrast enhancement. The primary tumor itself cannot be distinguished form SCC by cross-sectional imaging (Becker et al. 1998); perineural spread can also occur in SCC. Thus, differentiation of ACC and SCC requires histopathologic analysis.
6.3.3.2
Mucoepidermoid Carcinoma
As adenoid cystic carcinoma, mucoepidermoid carcinoma arises from minor salivary glands. An important aspect to mucoepidermoid carcinoma is the wide range of histological subclassifications (Som and Brandwein 2003; Smoker 2003). Low-grade mucoepidermoid carcinoma have a very good prognosis. On imaging studies they appear as well-delin- eated solid tumors. Cystic tumor components and even calcifications can be present. On the other hand, high-grade mucoepidermoid carcinoma have a very poor prognosis. The latter tumors are ill-defined and have similar imaging characteristics as SCC or ACC.
6.3.3.3
Miscellaneous (see also Table 6.1)
Other malignancies in the oral cavity are extremely rare. However, lymphoma, especially non-Hodgkin lymphoma (NHL), merits some attention (see also Chap. 16). Extranodal involvement of the oropharynx by NHL or Burkitt lymphoma can reach a considerable size and, this way extend ventrally to affect the oral cavity. NHL tends to present with homogeneous masses, usually, originating from lymphatic tissues of the base of the tongue or the pharyngeal tonsils (Fig. 6.28). Necrotic tumor components are rare as opposed to carcinomas. This also applies to cervical
lymph nodes and more remote tumor sites which are mostly present in NHL (Lee et al. 1987).
Other extremely rare malignancies include sarcoma (rhabdomyo-, lipo-, fibro-, angio-, and leiomyosarcoma). Among these, rhabdomyosarcoma merit further attention since these tumors are the most frequent malignancies during the first two decades of life (Peters et al. 1989). Several histopathologic subtypes occur in rhabdomyosarcomas, which have a predilection for the head and neck region. In the oral cavity, the floor of the mouth and the tongue are more frequently involved than the rest of the oral cavity. On precontrast images, they have the density of muscle. Mostly, there is inhomogeneous contrast enhancement. On MR, rhabdomyosarcomas may be slightly hyperintense on T2-weighted images. Both welland ill-defined masses have been reported.
6.3.4
Recurrent Cancer
In the oral cavity, there are typical post-therapeutic imaging findings which should not be misinterpreted with recurrent tumor. After radiation therapy these alterations are generally unspecific and consist in mucosal thickening, edematous changes, and later fibrotic changes (for a more general description of tissue changes after radiotherapy, see Chap. 4).
A specific complication in the oral cavity after radiation therapy may be osteoradionecrosis (Fig. 6.29) which usually presents with local lysis, sclerosis and
Fig. 6.28. CT of a 50-year-old female with multi-focal nonHodgkin lymphoma also involving her left masseter muscle, cheek, and lip

124 |
M. Keberle |
Fig. 6.29. Axial CT-image (bone window) of a patient treated by external irradiation 10 years earlier for a right-sided parotid malignancy, now presenting with oral pain and mucosal dehiscence. Extensive resorption of right-sided mandibular spongiosa and destruction of both lingual and buccal cortex, complicated by a pathologic fracture (arrowheads). Intra-osse- ous air bubbles are seen. Histopathologic examination showed necrotic bone with signs of osteomyelitis (Courtesy of Robert Hermans, MD, PhD, Leuven, Belgium)
eventually bone destruction (Hermans 2003; Weber et al. 2003). On the other hand, recurrent tumor may infiltrate the mandible or maxilla. Although sometimes difficult, CT is the imaging modality of choice to differentiate osteoradionecrosis and recurrent tumor with bony infiltration. An adjacent soft tissue mass suggests the presence of bony tumor infiltration, whereas a typical moth-eaten appearance and sequestrations favor the diagnosis of osteoradionecrosis.
Specific post-operative changes in the oral cavity can be seen after hemiglossectomy (Lell et al. 2000). Often the tip of the tongue is inverted towards the resected side. Sometimes soft tissue reconstructions (e.g. myocutaneous flaps) are performed to reduce functional impairment after surgery (Fig. 6.30) (Hudgins et al. 1994). Due to denervation, transformation of muscle into fat and eventually atrophy of the transplanted flap occur.
In contrast to primary carcinoma, which start out superficially, recurrent tumor mainly grows deeply so that for clinicians it is difficult to find recurrent tumor in an early stage (Fig. 6.31). However, because of the aforementioned expected post-therapeutic tissue changes and the possible presence of other post-ther- apeutic lesions (e.g. inflammatory changes, granulation tissue, etc.), it is challenging to find a recurrent cancer on imaging studies. In general, the signs for recurrent tumor are similar to the pretherapeutic situation.
There is a predisposition for local recurrences in the tongue (Fig. 6.32). The reason for this are the rather close resection margins in patients with tumors that are close to or just across the midline in order to avoid severe post-operative swallowing disorders (Keberle et al. 2003).
Rather than evaluating anatomic features associated with tumor growth, FDG-PET assesses abnormal metabolic activity of tumor and, this way, avoids some of the difficulties inherent in examining the post-treatment head and neck (Lapela et al. 1995). However, except for a high negative predictive value (91%) the positive predictive value is rather low (5%) (Goodwin 1998) (see also Chap. 17).
Fig. 6.30. Axial MRI of 63-year-old male patient after resection of a squamous cell carcinoma with flap reconstruction on the right side (a). On the one hand, note the flow-voids of the arterial supply and the fatty transformation of the myocutaneous flap itself. And on the other hand, note the fatty transformation of the muscles (asterisk) between the flap and the midline due to muscle denervation. The borders of the flap and of the anatomic structures are smooth, there is no recurrence
