
Учебники / Head_and_Neck_Cancer_Imaging
.pdf
Neoplasms of the Sinonasal Cavities |
207 |
onstrating nerve tissue differentiation; sometimes foci of mature cartilage and bone, skeletal muscle differentiation (called ‘malignant Triton tumor’), and glandular or epithelioid components are histologically recognized (Heffner and Gnepp 1992).
PNSTs are rarely encountered in the sinonasal region and present with aspecific symptoms (Buob et al. 2003).
11.5.2.1.5
Ewing Sarcoma and Primitive Neuro-ectodermal Tumor (PNET)
These two neoplasms, which are very rarely seen in the sinonasal cavity, typically occur in childhood and young adults. They appear histologically very similar, and are distinguished based on immunohistochemical and ultrastructural differences.
These are aggressive neoplasms, that rapidly metastasize to distant sites.
11.5.2.1.6 Meningioma
Extracranial meningiomas are rare. The most frequent sites for extracranial meningiomas are the orbit, nose, paranasal sinuses and middle ear, and at the skull base foramina. Sinonasal meningioma most frequently affects the nasal cavity (Thompson and Gyure 2000) (Fig. 11.15). Extracranial meningiomas are formed by direct extension outside the skull of a primary intracranial meningioma, by metastasis from a malignant intracranial meningioma, or originate from extracranial arachnoid cell clusters. These cell clusters accompany certain of the cranial nerves outside the cranium.
The imaging characteristics are similar to those of intracranial meningioma: an enhancing mass lesion, remodelling bone, is seen.
11.5.2.2
Mesenchymal Neoplasms
11.5.2.2.1 Vascular Tumors
11.5.2.2.1.1
Juvenile Angiofibroma
Juvenile angiofibroma is an uncommon, highly vascular, locally invasive benign tumor which originates almost exclusively in the posterior nasal cavity of adolescent males. The tumor has the potential to kill or to cause serious morbidity due to uncontrolled growth,
and sometimes also indirectly due to treatment complications. The prefix ‘juvenile’ is commonly used, but the lesion also occurs in childhood and (rarely) middle age. The tumor has been reported to occur in young females, but these examples are so exceptional that some authors state that sex chromosome studies are indicated if the diagnosis is confirmed in a female patient. The onset of symptoms occurs between 7 and 21 years of age. Symptoms include nasal obstruction, recurrent severe epistaxis, purulent rhinorrhea, facial deformity and nasal speech. The diagnosis can usually be made on the basis of history, physical examination and imaging studies. Clinically, a deep red mass with increased vascularity of the overlying mucosa is seen. Biopsy is seldom required and dangerous to perform.
On CT and MRI, the tumor appears as a strongly contrast-enhancing mass lesion in the posterior nasal cavity and nasopharynx. Intratumoral flow voids are present on MR images. The mass lesion is typically centred on the sphenopalatine foramen and very often extends into the pterygopalatine fossa, resulting in widening of this fossa with anterior bowing of the posterior maxillary wall (Fig. 11.16). As the tumor grows, it tends to extend into the ipsilateral nasal cavity. Invasion of the neighbouring skull base
Fig. 11.15. Sagittal T1-weighted spin-echo image in a patient presenting with a nasal soft tissue mass. A large and strongly enhancing lesion is seen in the anterior cranial fossa (arrows), extending into the nose (arrowheads). Meningioma

208 |
R. Hermans |
a |
b |
Fig. 11.16a,b. Male adolescent presenting with recurrent epistaxis. Axial T1-weighted image spin echo image (a) shows a mass lesion (white arrows) centered on the left pterygopalatine fossa, anteriorly displacing the posterior maxillary wall and extending into the skull base. Normal right pterygopalatine fossa (arrowhead). The axial T1-weighted image after injection of gadolinium (b) demonstrates the dramatic enhancement of the lesion; some subtle flow voids are visible in the lesion
structures is often seen; in more than half of patients the sphenoid sinus is invaded through the roof of the nasopharynx (Fig. 11.17). Orbital and infratemporal spread are not uncommon. In large tumors, even intracranial extension may be seen. Angiography shows a hypervascular tumor, mainly supplied by the
Fig. 11.17 Male adolescent presenting with nasal obstruction; no history of epistaxis. Sagittal reformatting of axial contrastenhanced CT images. A strongly enhancing soft tissue mass (arrowheads) is seen in the choanae and in the nasopharyngeal roof, invading the sphenoid sinus. Juvenile angiofibroma
internal maxillary artery and ascending pharyngeal artery; this procedure is not usually needed for diagnosis, but is performed for presurgical tumor embolization. Natural regression almost never occurs. The tumor is radiosensitive, but the preferred therapy is complete surgical resection after selective tumor embolization. The prognosis is good, although fatalities due to haemorrhage are possible. Recurrences are probably related to incomplete resection, due to the multilobular nature of the tumor and its ability to invade adjacent spaces.
11.5.2.2.1.2 Angiomatous Polyp
An angiomatous polyp corresponds to a vascular compromised nasochoanal component of an antrochoanal polyp or sphenochoanal polyp. Because of the compression of the feeder vessels in the polyp, a sequence of dilatation and stasis of feeder vessels, oedema, infarction and neovascularization is set up (De Vuysere et al. 2001). This may lead to total necrosis or more often to an angiomatous polyp (Fig. 11.18). The term ‘angiomatous polyp’ is sometimes also used for a vascularized and fibrosed nasal polyp, presumed to be the response to minor trauma, but little can be found about this in the literature.
11.5.2.2.1.3 Hemangioma
Hemangioma is a benign vascular tumor that is especially common on the skin but may be present in

Neoplasms of the Sinonasal Cavities |
209 |
a 
 b
b
Fig. 11.18a,b. Axial gadolinium-enhanced T1-weighted images show maxillary polyp (asterisk) passing through an accessory ostium into the posterior nasal cavity (a, arrow). The pharyngeal component enhances strongly (b, arrow): angiomatous polyp. Vascular compromise at the level of the accessory ostium may induce a sequence of dilatation, stasis and occlusion of the feeder vessels, eventually leading to neovascularisation of the extrasinusal polyp component
any tissue, including bone. It is the most common tumor of childhood. Hemangiomas are not usually seen at birth, but show a rapid postnatal proliferation with slow involution afterwards. A hemangioma should not be confused with a vascular malformation, which is present at birth (although not always evidently) and grows with the child into adulthood.
About 60% of haemangiomas occur in the head and neck. Most are cutaneous lesions, but they also occur in the deeper tissues. A non-osseous localisation within the nose and/or paranasal sinuses is very uncommon. They may block the airway when located within the nose (Fig. 11.19). Hemangiomas in the paranasal sinuses are more rare than in the nose. Paranasal hemangioma sometimes causes destruction of adjacent bone, making it difficult to differentiate them from a malignant lesion (Fig. 11.20) (Kim et al. 1995).
Hemangioma within the maxillofacial bony structures is also rare; the mandible is affected most commonly.
11.5.2.2.1.4 Hemangiopericytoma
Hemangiopericytoma is a vascular tumor that can arise wherever capillaries are present. The pericytes surrounding the endothelial cells are believed to be the cells of tumor origin. About 15%–25% of hemangiopericytomas occur in the head and neck region, half of these in the nose or paranasal
sinuses. It is a rapidly growing, usually painless tumor, and is seen at all ages. The prognosis after resection is unpredictable; they should be regarded as locally aggressive tumors with a relatively high recurrence rate. On CT and MRI, a hemangiopericytoma appears as an expansile, bone remodelling lesion with variable enhancement of the mass (Fig. 11.21).
Fig. 11.19. Axial gadolinium-enhanced T1-weighted spin-echo image in a 5-month-old patient. Enhancing soft tissue tumor (arrows) in the wall of the left nostril, somewhat extending in the left nasal cavity; inferior nasal concha (arrowhead). Hemangioma

210 |
R. Hermans |
a |
b |
Fig. 11.20a,b. Coronal T2-weighted spin echo image (a) and axial gadolinium-enhanced spin echo image (b) in a 64-year-old patient, presenting with nasal obstruction, epistaxis and facial deformity; the complaints had been present for years. A large heterogenous soft tissue mass is seen in the nose and maxillary sinus, showing moderate enhancement. Expansion of the right maxillary sinus is evident. The lesion was endoscopically resected. Histologic examination showed hematoma with reparative phenomena; focally, clusters of vessels were recognized, suggesting an underlying vascular malformation or hemangioma
11.5.2.2.2
Osseous and Cartilaginous Tumors
11.5.2.2.2.1 Osteosarcoma
Osteosarcoma is a malignant neoplasm arising from bone forming cells. About 6% of the osteosarcomas originate in the maxillofacial skeleton, the mandible being the most frequent site. There is a wider age distribution in maxillofacial osteosarcoma than in skeletal osteosarcoma which occurs predominantly in the second decade of life. On imaging, these neoplasms appear as mass lesions, causing osteolysis or mixed lytic–sclerotic bone alterations. Within the tumor, new bone formation is commonly seen (Fig. 11.22).
11.5.2.2.2.2 Chondrosarcoma
Chondrosarcoma is a malignant neoplasm derived from cartilage cells. In the head and neck, they are seen originating from the jaw bones, sinonasal region (usually nasoethmoidal), skull base, larynx and trachea. It is difficult to firmly differentiate between benign chondroma and low-grade chondrosarcoma on a small amount of tissue obtained by biopsy; both may show a lobular growth pattern. Compared to chondroma, low-grade chondrosarcoma may display only minimally increased cellularity and nuclear atypia, a pattern overlapping with benign chondro-
mas; there is no appreciable degree of mitotic activity in such lesions.
The distinctive imaging feature of these tumors is a mass containing scattered calcifications, as visible on CT. On MRI they usually display low signal on T1-
Fig. 11.21. Coronal T1-weighted gadolinium-enhanced spinecho image. A strongly enhancing expansile mass is seen in the right maxillary sinus, displacing and eroding the orbital floor, extending into the nasal cavity and through the lateral maxillary wall. This patient suffered hemangiopericytoma
Neoplasms of the Sinonasal Cavities
a
b
c
211
weighted and high signal on T2-weighted sequences, as well as presence of low signal intensity septa separating high signal intensity lobules on T2-weighted images (De Beuckeleer et al. 1995). After injection of gadolinium, these tumors typically show enhancement of scalloped margins and curvilinear septa (the so-called ‘ring-and-arc pattern’); the enhanced areas correspond to fibrovascular bundles surrounding hyaline cartilage lobules (Fig. 11.23) (Aoki et al. 1991).
Surgery is the only curative modality of cartilaginous tumors. Low-grade chondrosarcomas may locally recur if incompletely resected, but have only limited risk of metastatic disease.
11.5.2.2.3
Soft Tissue Sarcomas
11.5.2.2.3.1 Rhabdomyosarcoma
Rhabdomyosarcoma is a malignant tumor of skeletal muscle. This tumor mainly occurs in children. Apart from lymphoma, it is the most common malignant tumor of the head and neck in childhood. Rhabdomyosarcoma is divided into four histological subtypes: embryonal, botryoid, alveolar and pleomorphic; the embryonal and botryoid subtype account for about 90% of primary head and neck lesions. Head and neck rhabdomyosarcoma has three sites of predilection: the orbit, the nasopharynx and paranasal cavities, and the temporal bone.
These tumors are usually large at presentation and nearly always invade neighbouring structures (Fig. 11.24).
Rhabdomyosarcoma may show early metastases, sometimes before significant local invasion occurs. The lung is the most frequent site of distant metastasis (Herrmann et al. 2003). As the treatment is determined by the local tumor extent and the possible presence of distant disease, imaging should include a CT and/or MRI scan of the primary tumor site and a CT scan of the chest. In patients at risk of developing meningeal extension, a gadolinium-enhanced MR study of the brain should be performed.
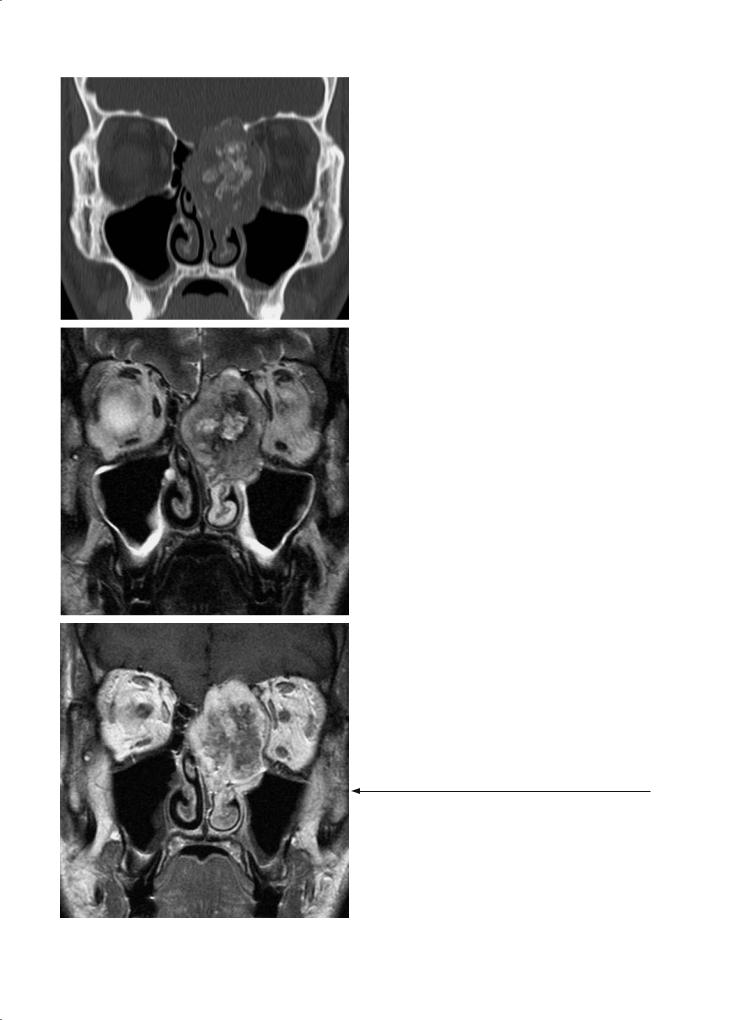
Fig. 11.22a–c. A 26-year-old patient presenting with severe headache and proptosis on the left side. a Coronal CT image (bone window). Expansile nasoethmoidal mass lesion on the left, growing through the nasal septum, displacing the medial orbital wall and causing destruction of the nasoethmoidal roof. The lesion contains areas of gross calcification and/or ossification. b,c Corresponding coronal T2-weighted (b) and gadolinium-enhanced T1-weighted spin echo image (c). Biopsy showed osteosarcoma

212
a
b
c
R. Hermans
11.5.2.2.3.2
Other Soft Tissue Sarcomas
Other soft tissue sarcomas, such as leiomyosarcoma, fibrosarcoma and malignant fibrous histiocytoma have been reported to occur in the sinonasal area, but they are all very rare.
11.5.2.3 Lymphoreticular Tumors
11.5.2.3.1 Lymphoma
For a more general discussion on lymphoma, see Chap. 16.
In non-Hodgkin lymphoma (NHL), two distinct extranodal sites are recognized: extranodal lymphatic spread or involvement of Waldeyer’s ring, and extranodal extralymphatic spread. Extranodal extralymphatic NHL occurs most commonly in the sinonasal cavities and orbits. In a series of 55 cases of extranodal NHL of the head and neck, 11 patients (34%) had involvement of the sinonasal cavities and/or palatum (Fig. 11.25). In most of these cases, bone alterations were present and appeared always lytic; tumor traversing bone without clear lysis was not observed (Hermans et al. 1994). The radiological appearance of such a tumor mass is aspecific, but the association with pathological neck lymph nodes (especially when appearing large and non-necrotic on imaging studies) and/or involvement of Waldeyer’s ring, suggests the diagnosis of NHL (Hermans et al. 1994).
11.5.2.3.2 Plasmocytoma
Plasmocytoma is usually a polyostotic neoplasm (multiple myeloma), but solitary lesions may occur. The maxillofacial skeleton is affected in about 30%
Fig. 11.23a–c. A 15-year-old patient presenting with progressive nasal obstruction. a Coronal T2-weighted spin echo image. Large midline nasal mass, showing overall high intensity but transversed by low-intensity bands. The nasal septum can not be recognized. The lesion reaches the left lamina cribrosa, but there is no evidence of erosion of this structure. The inferior and middle nasal conchae (arrows) are pushed against the lateral nasal wall. Inflammatory changes in the surrounding paranasal sinuses. b Coronal gadolinium-enhanced T1weighted spin echo image shows a ‘ring and arc’ enhancement pattern. c Axial gadolinium-enhanced T1-weighted spin echo image. The lesion is centered on the nasal septum. The tumor was surgically removed. Histology showed low grade chondrosarcoma

Neoplasms of the Sinonasal Cavities |
213 |
a |
b |
Fig. 11.24a,b. Coronal T1-weighted spin echo image (a) shows large mass in the left maxillary sinus, growing through the orbital floor, and into the nasal cavity and adjacent ethmoidal cells; high signal intensity just below the fovea ethmoidalis probably corresponds to thickened secretions (white arrowhead). Axial gadolinium-enhanced T1-weighted spin (b) also reveals posterior extension into the pterygopalatine fossa and retromaxillary fat (arrows); invasion of the nasolacrimal canal (black arrowhead). Rhabdomyosarcoma
of the cases, the mandible more frequently than the maxilla. Radiologically, multiple sharply demarcated osteolytic lesions are seen, usually with a diameter smaller than 2 cm; sometimes it may appear as confluent osteolytic lesions with poorly defined borders
Fig. 11.25. Coronal CT image (soft tissue window). Polypoid nasoethmoidal soft tissue mass (arrows), bulging into the maxillary sinuses; destruction of ethmoidal septae and erosion of surrounding bone structures is seen. Non-Hodgkin lymphoma
or as generalized osteoporosis. Solitary lesions may be difficult to differentiate from odontogenic tumors or odontogenic cysts.
Extramedullary plasmocytoma is an uncommon plasma cell neoplasm, arising most frequently from the soft tissues of the head and neck region, without evidence of systemic disease. The most common sites are the nose and the paranasal sinuses. The gross appearance is nonspecific (Fig. 11.26). It may spread to surrounding soft tissues and invade bone, and may show lymphatic metastasis. There is controversy as to whether extramedullary plasmacytoma is a separate clinicopathological entity, or a stage in the development of multiple myeloma. Intramedullary lesions often evolve to multiple myeloma after a few years whereas extramedullary lesions, commonly involving sinonasal structures, typically remain solitary (Bourjat et al. 1999).
11.5.2.4 Fibro-osseous Disease
The most important entities belonging to the heading fibro-osseous disease are fibrous dysplasia and ossifying fibroma.
Fibrous dysplasia is a condition in which normal medullary bone is replaced by an abnormal proliferation of fibrous tissue, resulting in asymmetrical distortion and expansion of bone; it may be con-

214 |
R. Hermans |
a |
b |
Fig. 11.26a,b. Axial contrast-enhanced (a) and coronal (bone window) CT image (b) in a 72-year-old patient. Soft tissue mass in left nasal cavity (white arrowheads), growing into the nasopharynx. Erosion of the posterior side of the nasal septum and pterygoid process (black arrowheads). On the coronal image, lysis is apparent of all three nasal turbinates, as well as bulging of the medial maxillary wall. Extramedullary plasmocytoma
fined to a single bone (monostotic fibrous dysplasia) or involve multiple bones (polyostotic fibrous dysplasia).
The monostotic form may involve any of the facial bones, but is most commonly seen in the maxilla. The association of the polyostotic form with sexual precocity and cutaneous pigmentation in a female patient is known as McCune-Albright syndrome.
Fibrous dysplasia is a disease of young patients. It may be an incidental finding. In the maxilla it usually presents with swelling and deformity of the cheek, but sometimes it causes nasal obstruction and/or orbital symptoms. Fibrous dysplasia may give rise to a mucocele. Involvement of the skull base may cause neurovascular compression. Extensive involvement of the face is referred to as leontiasis ossea.
Usually no new lesions appear after the cessation of skeletal growth. The lesions become more sclerotic with time but may continue to grow slowly into adulthood. Occasionally, reactivation of the lesions occurs during pregnancy.
Aggressive clinical behaviour of maxillary fibrous dysplasia has been described, causing pain and rapid development of a mass, although histopathological examination shows typical findings of fibrous dysplasia without evidence of malignancy. However, secondary malignant degeneration into a sarcoma (0.5% of cases)
should be considered when stable or recurrent fibrous dysplasia produces pain or soft tissue extension.
Radiologically, fibrous dysplasia appears as enlarged bone with a dense ground-glass appearance; sometimes the lesions have a more osteolytic appearance, with regions of more dense calcification within them (Fig. 11.27). On MRI, the lesions usually have a low to intermediate signal intensity on all sequences, with marked contrast enhancement; incidentally found fibrous dysplasia may be confused with a neoplastic lesion on an MR study (Fig. 11.28).
Ossifying fibroma is a benign tumor composed of fibrous tissue and containing bone or osteoid. Ossifying fibroma of the craniofacial skeletal mainly, but not exclusively,occurs in children,hence the name juvenile ossifying fibroma (JOF). Two histopathological variants are distinguished: psammomatoid JOF and trabecular JOF (El-Mofty 2002). The imaging findings in JOF overlap with those in fibrous dysplasia (Commins et al. 1998). An aneurysmal bone cyst may develop in psammomatoid JOF; in such case, fluid levels are apparent on imaging studies. Both types may show a fast and aggressive growth pattern, eroding and invading the surrounding bone.
The term ossifying fibroma has also been used to describe odontogenic neoplasms in adults, which are also known as cemento-ossifying fibroma and cementifying fibroma.

Neoplasms of the Sinonasal Cavities |
215 |
b
a
Fig. 11.27a,b. Axial (a) and coronal (b) CT images (bone window) in a 20-year-old patient with progressive naso-orbital swelling on the left. A largely calcified, well-delimited lesion is seen centered on the left ethmoid, involving the fovea ethmoidalis and lamina papyracea, and displacing the medial orbital wall and extending into the naso-orbital corner. The lesion was resected, and histologic examination showed fibrous dysplasia
a 
 b
b
Fig. 11.28a,b. Patient presenting with episodes of visual disturbances. On an axial gadolinium-enhanced T1-weighted brain spinecho image, an enhancing mass lesion is seen in the sphenoid sinus (a, arrow), initially suspected to correspond to a neoplastic lesion. Coronal CT image shows the typical ground-glass appearance of fibrous dysplasia (b, arrowhead)
11.6
Therapeutic Relevance of Imaging Findings
Many patients with malignant sinonasal neoplasms are managed surgically. Most cancers will require some form of transfacial surgical approach, with more or less extensive resection of sinonasal structures.
Preoperative imaging may influence the composition and approach of the surgical team treating a patient with sinonasal cancer (Ahmadi et al. 1993). Surgical resection of sinonasal neoplasms involving
the anterior skull base requires a combined transfacial and transcranial approach to allow an en bloc resection of the tumor. This means that a neurosurgical team and a head and neck surgical team will work in close cooperation during such an anterior fossa craniofacial resection. This procedure is indicated for lesions involving or transgressing the anterior skull base, and should be considered when a tumor comes close to the skull base and is unlikely to be resected completely using a standard transfacial technique (Kraus and Andersen 1997). Dural invasion can usually be handled safely during a craniofacial resec-

216 |
R. Hermans |
tion, but cure (often at the expense of neurological sequelae) can hardly ever be obtained if brain invasion is present.
The surgical management of orbital involvement is controversial. In general, if the tumor has not grown through the periorbita, the eye may be surgically preserved (Eisen et al. 2000). Involved periorbita can be resected, but the functional results of patch reconstruction are not very good; furthermore, all these patients will need postoperative radiotherapy, including the orbit. Invasion of the orbital fat precludes complete resection of the tumor without orbital exenteration. In a number of cases, the final decision regarding orbital exenteration will have to made depending on the intra-operative findings (Maroldi et al. 1997).
Perineural extension towards the foramen rotundum and cavernous sinus makes surgical clearance of the tumor highly unlikely; it also suggests a low probability of cure with radiation therapy.
Nasal endoscopy has an important role in the diagnostic work-up of these patients, enhancing the traditional speculum and mirror examination of the nose, and being complementary to CT and/or MRI; endoscopy is also an excellent way to follow-up patients and look for early recurrences. In few cases endoscopic resection of a tumoral mass might be feasible. Imaging is essential in the selection of patients for such a limited intervention. The patients are to be advised of the possibility of proceeding
with a traditional procedure because of tumor extent. Experience with this approach is relatively limited (Jorissen 1995; Levine et al. 1997; Goffart et al. 2000).
Surgery can be the sole treatment modality or part of a multimodality treatment plan, depending on tumor extent; often a combined treatment will be necessary. In advanced sinonasal cancer, surgery is often combined with radiation therapy to improve outcome. The radiation fields are individualized based on disease extent; the radiation dose to critical structures as the eye and brain should be as low as possible to avoid added morbidity. CT and/or MRI findings play an important role in this regard; in a postoperative situation the surgical and pathological findings also influence the radiation portal set-up.
11.7
Imaging After Therapy
Residual or recurrent cancer after therapy displays similar tissue characteristics on CT or MR studies, as the primary tumor before treatment. A focal, rounded, contrast-enhancing soft tissue mass within the previous tumor bed is suggestive for tumor recurrence (Fig. 11.29). However, after surgery and radiotherapy, scar, granulation tissue and/or
a 
 b
b
Fig. 11.29a,b. Patient treated by endoscopic surgery and radiotherapy for left-sided maxillary squamous cell carcinoma. At 2 years later, endoscopic examination was suspicious for tumor recurrence. Coronal T1-weighted spin-echo images, before (a) and after (b) injection of gadolinium, show nodular, enhancing mass lesion (arrowhead) abutting the floor of the left orbit. Some inflammatory changes are present in the left maxillary sinus. The lesion was resected and corresponded to recurrent cancer
