
- •Contents
- •Preface
- •Acknowledgements
- •Abbreviations
- •Contributors
- •1 Normal pregnancy
- •2 Pregnancy complications
- •3 Fetal medicine
- •4 Infectious diseases in pregnancy
- •5 Medical disorders in pregnancy
- •6 Labour and delivery
- •7 Obstetric anaesthesia
- •8 Neonatal resuscitation
- •9 Postnatal care
- •10 Obstetric emergencies
- •11 Perinatal and maternal mortality
- •12 Benign and malignant tumours in pregnancy
- •13 Substance abuse and psychiatric disorders
- •14 Gynaecological anatomy and development
- •15 Normal menstruation and its disorders
- •16 Early pregnancy problems
- •17 Genital tract infections and pelvic pain
- •18 Subfertility and reproductive medicine
- •19 Sexual assault
- •20 Contraception
- •21 Menopause
- •22 Urogynaecology
- •23 Benign and malignant gynaecological conditions
- •24 Miscellaneous gynaecology
- •Index

Chapter 7 |
327 |
|
|
Obstetric anaesthesia
Pain relief in labour 328 Epidural analgesia: overview 330
Epidural analgesia: advantages and disadvantages 332 Anaesthetic techniques for Caesarean section: spinal 334 Anaesthetic techniques for Caesarean section: epidural 335 Anaesthetic techniques for Caesarean section: combined spinal
epidural 336
Anaesthetic techniques for Caesarean section: general anaesthesia 337

328 CHAPTER 7 Obstetric anaesthesia
Pain relief in labour
Uterine contractions in labour are associated with pain. Professionals can help to reduce women’s fears by giving precise, accurate, and relevant information antenatally including the types of analgesia available in their unit.
Ideal pain relief in labour
Should
•Provide good analgesia.
•Be safe for the mother and baby.
•Be predictable and constant in its effects.
•Be reversible if necessary.
•Be easy to administer.
•Be under the control of the mother.
Should not
•Interfere with uterine contractions.
•Interfere with mobility.
Non-pharmacological methods
•Education regarding what to expect may help reduce fear and the sense of loss of control.
•A trusted companion present throughout labour and birth reduces the need for pain relief.
•Warm bath, acupuncture, hypnosis, and homeopathy are also helpful.
Transcutaneous electrical nerve stimulation (TENS) is a safe form of analgesia. It may help with short labour and postpone the need for stronger analgesia, but may not be adequate as labour advances.
Pharmacological methods
Nitrous oxide (Entonox®)
Entonox® is premixed nitrous oxide and oxygen as a 50:50 mixture. It is self-administered and has quick onset of action and a short half-life. Side effects can include feeling faint, nausea, and vomiting.
Narcotic agents
•Pethidine: administered at a dose of 50–150mg; onset of action is 15–20min. It lasts about 3–4h and can be repeated. It is usually given with an antiemetic. If given within 2h of delivery, it can cause neonatal respiratory depression and naloxone may be needed.
•Diamorphine: is also used in some units at a dose of 2.5–5mg. There is controversy about the extent and timing of neonatal respiratory depression, but it may be up to 3–4h after the last dose.
•Meptazinol: is an opioid that may cause less respiratory depression. The onset of action starts in 15min and lasts for about 2–7h.
PAIN RELIEF IN LABOUR 329
Pudendal nerve block and local perineal infiltration
•Pudendal nerve block is used for operative vaginal delivery and is performed by the obstetrician: lidocaine (lignocaine) is injected 1–2cm medially, and below the right and left ischial spines; this is done transvaginally with a specially designed pudendal needle.
•Local anaesthetic such as lidocaine (lignocaine) is infiltrated in the perineum before performing an episiotomy at the time of delivery, or before suturing tears and episiotomies.
330 CHAPTER 7 Obstetric anaesthesia
Epidural analgesia: overview
Safe and effective analgesia for labour is still something that is not available for the vast majority of women in the world today. Although the provision of epidural analgesia during labour has been one of the greatest advances in the care of women during this difficult and distressing time, it still carries a small, but definite complication rate.
Consent for analgesia in labour
Women in labour present a particular group of patients in whom obtaining fully informed consent may be difficult because of a variety of factors such as pain, fatigue, or the effects of narcotic analgesia administered previously. Ideally anaesthetists should try to explain the risks and benefits of epidural analgesia to women in the antenatal period.
Anatomy
The epidural space lies between the spinal dura and the vertebral canal (Fig. 7.1). The superior margin is the foramen magnum, inferiorly the sacrococcygeal membrane. Posteriorly lies the ligamentum flavum and the anterior surfaces of the laminae, anteriorly the posterior longitudinal ligament. Within the epidural space lie the spinal nerve roots as well as the spinal arteries and extradural veins. The usual distance between skin and the epidural space in the lumbar region in adults is about 4–5cm. It is important to realize that the epidural space is continuous the whole way down the back. The lumbar region is chosen for the provision of labour analgesia as this is where the nerve roots involved in the production of pain during labour are found.
The pain of the first stage of labour is caused by uterine contractions and is referred by afferent A and C fibres mainly to dermatones T10–L1, and by distension of the perineum during the second stage of labour to S2–4.
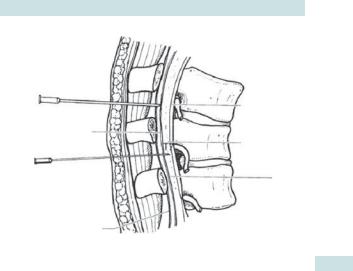
Epidural
needle
Epidural space
Spinal needle
Ligamentum flavum
EPIDURAL ANALGESIA: OVERVIEW 331
Posterior longitudinal ligament
Subarachnoid space
Dura
Fig. 7.1 Subarachnoid and epidural spaces. Reproduced from Allman KG, McIndoe A, Wilson I. (2011). Oxford Handbook of Anaesthesia, 3 edn. With permission from Oxford University Press.
332 CHAPTER 7 Obstetric anaesthesia
Epidural analgesia: advantages and disadvantages
Advantages
•Effective analgesia in labour.
•Reduced maternal catecholamine secretion (thought to benefit fetus).
•Can be topped up for an operative delivery or any other complications, e.g. retained placenta or difficult perineal repair.
•Can provide effective postoperative analgesia.
•Can be used to aid BP control in pre-eclampsia.
Disadvantages and complications
•Failure to site, or a patchy, or incomplete block.
•Hypotension from sympathetic blockade.
•Decreased mobility.
•Tenderness over the insertion site.
2 There is no association between epidural analgesia and long-term backache.
•Inadvertent dural puncture:
•incidence <1:100
•may develop a post-dural puncture headache, characterized by i on sitting up or standing
•may need treatment with an epidural blood patch.
•Respiratory depression:
•from the catheter migrating into the subarachnoid space followed by bolus of local anaesthetic (total spinal)
•from accumulation of epidurally administered opiates.
•Extremely rare complications resulting in neurological deficits:
•epidural abscess formation
•epidural haematoma
•damage to individual nerves or the spinal cord itself.
•Increased risk of operative delivery.
An alternative to epidural: remifentanil patient-controlled analgesia
There are a few women in whom epidural analgesia is contraindicated and who are not able to obtain adequate analgesia from more conventional methods such as nitrous oxide. Remifentanil, a powerful opiate which is rapidly metabolized and unable to cross the placenta, may be used via a patient-controlled IV system (patient-controlled analgesia (PCA)).

EPIDURAL ANALGESIA: ADVANTAGES AND DISADVANTAGES 333
Contraindications to epidural analgesia
•Septicaemia.
•Infection at site of insertion.
•Coagulopathy/thrombocytopaenia (platelet count < 75 × 109).
Beware of a falling count over the past few days—always check the platelet count if this has occurred.
If the platelet count is between 75 and 100 × 109, clotting studies should be performed before proceeding with the epidural.
•Raised intracranial pressure.
•Haemorrhage and cardiovascular instability/hypovolaemia.
2There may be limited circumstances where an epidural is appropriate in these cases.
•Known allergy to amide (lidocaine-type) local anaesthetic solutions or opioids.
•Fixed cardiac output states, e.g. severe aortic stenosis, hypertrophic obstructive cardiomyopathy (HOCM).
Technique for siting an epidural
•The procedure should be explained and consent sought.
•There should be no clotting abnormalities.
•Establish wide-bore IV access.
•Position the woman either on her side or sitting, with the back curved to open intervertebral spaces.
•Full aseptic technique must be followed.
•A suitable interspace, usually L3/4, is identified and lidocaine (lignocaine) 1% injected.
•The epidural space is identified by a loss of resistance technique, usually to saline 0.9%.
•Once the space is identified, a catheter is threaded in and the needle withdrawn and the catheter firmly fixed to the skin.
•A test dose of local anaesthetic, usually bupivacaine, can be given to check that the epidural catheter has not inadvertently entered the subarachnoid space.
•Various regimens exist for the delivery of local anaesthetic to the epidural space either involving bolus administration or infusions.
•Careful monitoring is mandatory following epidural top-up doses including BP reading every 5min for 20min following the administration of a top-up dose.
•Block height and degree of motor block should be recorded.
•Continuous electronic fetal monitoring is required if an epidural has been sited.
Further reading
Mhttp://www.youtube.com/watch?v=1evFwMXnGiI

334 CHAPTER 7 Obstetric anaesthesia
Anaesthetic techniques for Caesarean section: spinal
Regional anaesthetic techniques are undoubtedly safer for the woman and most anaesthetists would counsel women having a CS to opt for one of them. However, the choice of anaesthetic technique may be influenced by the urgency of the CS. Facilities for conversion to GA, such as drugs and endotracheal tubes must always be available, as conversion to GA may be required if the block wears off during surgery, or is too high, or if the woman requests it due to pain or discomfort.
Spinal anaesthesia
•Accounts for the majority of CS performed in the UK.
•Fasting and antacid precautions are ideal, as GA may be required if the block is unsatisfactory.
•Good IV access is essential to provide fluids rapidly to counteract hypotension that may occur. Vasopressor drugs, such as phenylephrine or ephedrine, should also be available.
•Hyperbaric bupivacaine 0.5% in a dose of 12.5–15mg is usually used, together with an opiate such as fentanyl (20 micrograms) or damorphine (around 250 micrograms).
Advantages and disadvantages
Advantages
•Technically relatively easier than epidurals to perform.
•Enable mother to bond immediately with baby.
•The most reliable option for establishing a dense, bilateral block.
Disadvantages
•May cause severe hypotension.
•May wear off if surgery is unexpectedly prolonged.
Hypotension is common due to sympathetic blockade and inadequate tilt leading to aortocaval pressure, and must be prevented by the use of fluids, adequate left lateral tilt, and vasopressors if appropriate.
2Patients must be warned of the risk of intra-operative pain and the small chance of conversion to GA.
2The full extent of the block must be tested and recorded by the anaesthetist, prior to the commencement of surgery.
ANAESTHETIC TECHNIQUES FOR CAESAREAN SECTION: EPIDURAL 335
Anaesthetic techniques for Caesarean section: epidural
Conversion of a functioning epidural from analgesia to anaesthesia is the choice if a woman requires an operative or instrumental delivery, provided there is sufficient time (it takes about 20min or longer).
Advantages and disadvantages
Advantages
•Can be topped, should the surgery be extended.
•Can be used for good postoperative analgesia.
Disadvantages
•More likely than spinal anaesthesia to produce patchy or unilateral blockade.
•Takes longer to establish an adequate block.
•Can be technically difficult, with a higher incidence of headache in the event of inadvertent dural puncture.
•The catheter can migrate into the subarachnoid or subdural space, resulting in unpredictable and possibly fatal complications if large doses of local anaesthetic are administered.
•Larger doses of local anaesthetic agents are required, leading to the possibility of toxicity if the catheter has migrated intravenously.
336 CHAPTER 7 Obstetric anaesthesia
Anaesthetic techniques for Caesarean section: combined spinal epidural
These are usually performed by inserting a spinal needle through an epidural needle, although two separate injections may be performed.
2 Combined spinal epidural (CSE) anaesthesia combines the advantages of spinal anaesthesia, i.e. speed of onset and dense block, with the ability to prolong the period of anaesthesia and analgesia via the epidural route.
Advantages and disadvantages
Advantages
•The epidural component can be used to top-up the block.
•A smaller volume of local anaesthetic can be used intrathecally and the block extended gradually with the epidural component (this may cause less cardiovascular instability and be useful in women with cardiac disease).
•The epidural component can provide postoperative analgesia.
Disadvantages
•There is a higher risk of failure of the intrathecal component.
•Possible higher risk of meningitis than with either spinal or epidural alone.
•The epidural component of the technique is untested and any local anaesthetic agents must be given in small boluses, in case the catheter is in the subarachnoid space.

ANAESTHETIC TECHNIQUES FOR CAESAREAN SECTION: GA 337
Anaesthetic techniques for Caesarean section: general anaesthesia
There has been a general trend throughout the developed world away from using GA for CS. However, it is still necessary in the presence of contraindications to regional anaesthesia or in an emergency.
Problems with GA
•Potential airway difficulties: incidence of failed intubation in pregnant women is approximately 1:300 compared with 1:3000 in the general surgical population.
•Pulmonary aspiration of gastric contents.
•Awareness: rare with modern anaesthetic techniques, but may occur if inadequate levels of inhalational agents are used.
Technique for GA in pregnancy
•Adequate assessment of the airway is essential, as well as questioning about relevant medical, obstetric, and drug treatment, and allergies.
•Antacid prophylaxis must be administered.
•Left lateral tilt maintained at all times to prevent aortocaval compression.
•Adequate preoxygenation must precede induction of GA, regardless of the obstetric indications for the CS.
•ECG, pulse oximetry, and capnographic monitoring must be available.
•For full discussion of GA for CS, readers are advised to consult a specialist anaesthetic text.
Emergency GA is associated with increased maternal morbidity and mortality.
2There are few absolute indications for GA for CS.
This page intentionally left blank
