
- •Contents
- •Preface
- •Acknowledgements
- •Abbreviations
- •Contributors
- •1 Normal pregnancy
- •2 Pregnancy complications
- •3 Fetal medicine
- •4 Infectious diseases in pregnancy
- •5 Medical disorders in pregnancy
- •6 Labour and delivery
- •7 Obstetric anaesthesia
- •8 Neonatal resuscitation
- •9 Postnatal care
- •10 Obstetric emergencies
- •11 Perinatal and maternal mortality
- •12 Benign and malignant tumours in pregnancy
- •13 Substance abuse and psychiatric disorders
- •14 Gynaecological anatomy and development
- •15 Normal menstruation and its disorders
- •16 Early pregnancy problems
- •17 Genital tract infections and pelvic pain
- •18 Subfertility and reproductive medicine
- •19 Sexual assault
- •20 Contraception
- •21 Menopause
- •22 Urogynaecology
- •23 Benign and malignant gynaecological conditions
- •24 Miscellaneous gynaecology
- •Index

Chapter 21 |
635 |
|
|
Menopause
Menopause: overview 636
Menopause: short-term consequences 637 Menopause: long-term consequences 638 Menopause: history taking and investigations 640 Premature menopause 642
Hormone replacement therapy: overview 644 Hormone replacement therapy: benefits 646 Hormone replacement therapy: risks 648 Hormone replacement therapy: uncertainties 650
Alternative medical treatments to hormone replacement therapy 651

636 CHAPTER 21 Menopause
Menopause: overview
All women will go through the menopause and the average age is 52yrs. The menopause is the cessation of the menstrual cycle and is caused by ovarian failure leading to oestrogen deficiency. Worldwide life expectancy is increasing and women live longer than men. A woman’s average life expectancy at birth in the UK is currently 81yrs and is estimated to reach 85yrs by 2031. Thus UK women can expect more than 30yrs of post-menopausal life. This population expansion will lead to an increasing importance of the health problems that affect post-menopausal women.
Definitions
•Menopause is the permanent cessation of menstruation that results from loss of ovarian follicular activity. Natural menopause is recognized to have occurred after 12 consecutive months
of amenorrhoea for which no other obvious pathological or physiological cause is present.
•Peri-menopause includes the period beginning with the first clinical, biological, and endocrinological features of the approaching menopause, such as vasomotor symptoms and menstrual irregularity, and ends 12mths after the last menstrual period.
•Pre-menopause is a term often used to refer either to the 1–2yrs immediately before the menopause or to the whole of the reproductive period before the menopause. Currently, this term is recommended to be used in the latter sense.
•Post-menopause should be defined from the final menstrual period regardless of whether the menopause was induced or spontaneous.
•Menopausal transition is the period of time before the final menstrual period, when variability in the menstrual cycle usually is increased.
•Climacteric is the phase encompassing the transition from the reproductive state to the non-reproductive state. The menopause itself thus is a specific event that occurs during the climacteric, just as the menarche is a specific event that occurs during puberty.

MENOPAUSE: SHORT-TERM CONSEQUENCES 637
Menopause: short-term consequences
Vasomotor symptoms
Hot flushes and night sweats are the commonest symptoms of the menopause, and, although they may begin before periods stop, the prevalence of flushes is highest in the first year after the final menstrual period. Although they usually are present for less than 5yrs, some women will continue to flush into their 70s.
Sexual dysfunction
Changes in sexual behaviour and activity are common. The term female sexual dysfunction (FSD) is now used. The percentage of women with sexual dysfunction rises from 42% to 88% during the early to late menopausal transition. The underlying reasons for FSD are commonly multifactorial. For example, vaginal dryness, which results from declining levels of oestrogen, can cause dyspareunia. Low androgen levels have been implicated in low sexual desire though the evidence is conflicting. Non-hormonal factors, such as conflict between partners and life stress or depression, are important contributors to a woman’s level of interest in sexual activity. In addition, male sexual problems should not be overlooked.
Sexual problems are classified into various types:
•Loss of sexual desire.
•Loss of sexual arousal.
•Problems with orgasm.
•Sexual pain such as painful sex or dyspareunia.
Psychological symptoms
Psychological symptoms associated with the menopause include:
•Depressed mood.
•Anxiety.
•Irritability and mood swings.
•Lethargy and lack of energy.
However, most women do not experience major changes in mood at the menopause and psychological problems are likely to be associated with past problems and current life stresses.

638 CHAPTER 21 Menopause
Menopause: long-term consequences
Osteoporosis
Osteoporosis affects 1 in 3 women and 1 in 12 men. It is as ‘a skeletal disorder characterized by compromised bone strength predisposing to an increased risk of fracture’ (Table 21.1). Bone strength reflects the integration of two main features: bone density and bone quality. Bone density is expressed as grams of mineral per area or volume and, in any given individual, is determined by peak bone mass and amount of bone loss. BMD scan is used to measure the thickness of the bone in the hip and lumbar spine. Bone quality refers to architecture, turnover, damage accumulation (for example, microfractures), and mineralization. A fracture occurs when a failure-inducing force, which may or may not involve trauma, is applied to osteoporotic bone. Thus, osteoporosis is a significant risk factor for fracture. Fractures are the clinical consequences of osteoporosis.
The most common sites of osteoporotic fractures are:
•Lower end of radius (wrist or Colles’ fracture).
•Proximal femur (hip).
•Vertebrae.
Cardiovascular disease
Myocardial infarction and stroke are the primary clinical endpoints. Cardiovascular disease (CVD) is the most common cause of death in women over 60. Oophorectomized women are at 2–3-fold higher risk of coronary heart disease (CrHD) than age-matched pre-menopausal women.
Urogenital atrophy
The lower urinary and genital tracts have a common embryological origin and are approximated closely in adult women. Oestrogen receptors and progesterone receptors are present in the vagina, urethra, bladder, and pelvic floor musculature. Oestrogen deficiency after menopause causes atrophic changes within the urogenital tract and is associated with urinary symptoms, such as frequency, urgency, nocturia, incontinence, and recurrent infection. These symptoms may coexist with those of vaginal atrophy, including dyspareunia, itching, burning, and dryness.
|
|
MENOPAUSE: LONG-TERM CONSEQUENCES |
639 |
|
|
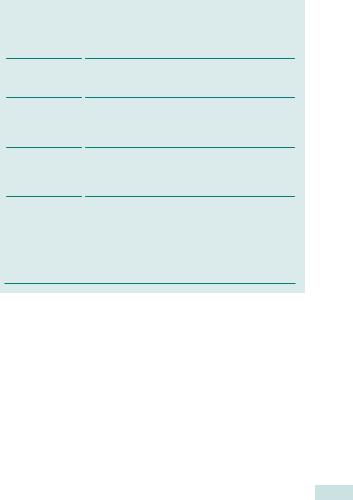
Table 21.1 Risk factors for osteoporosis |
|||
|
|
|
|
|
|
Risk factor |
Example |
||
|
|
|
|
|
|
Genetic |
Family history of fracture (particularly a 1st-degree |
||
|
|
relative with hip fracture) |
||
|
Constitutional |
Low BMI |
||
|
|
Early menopause |
||
|
|
(<45yrs of age) |
||
|
Environmental |
Cigarette smoking |
||
|
|
Alcohol abuse |
||
|
|
Low calcium intake |
||
|
|
Sedentary lifestyle |
||
|
Drugs |
Corticosteroids, >5mg prednisolone or equivalent |
||
|
|
daily |
||
|
|
Aromatase inhibitors |
||
|
|
GnRH analogues |
||
|
Diseases |
Rheumatoid arthritis |
||
|
|
Neuromuscular disease |
||
Chronic liver disease
Malabsorption syndromes
Hyperparathyroidism
Hyperthyroidism
Hypogonadism
640 CHAPTER 21 Menopause
Menopause: history taking and investigations
History
Symptoms, periods, and contraception
•Hot flushes and night sweats.
•Vaginal dryness.
•Other symptoms.
•Date of last menstrual period (could she be pregnant?).
•Frequency, heaviness, and duration of periods.
•Contraception.
Gynaecological history
•Hysterectomy.
•Oophorectomy.
Past medical and surgical history
•Risk factors for osteoporosis (see Table 21.1).
•Confirmed deep vein thrombosis or pulmonary embolism.
•Risk factors for cardiovascular disease (e.g. smoking, hypertension, diabetes).
•Breast cancer, benign breast disease, and date last mammogram (if applicable).
•Does she have migraines?
•Current medications.
•Does she take alternative or complementary therapies?
Family history in close family members
•Breast, ovarian, or bowel cancer.
•Confirmed deep vein thrombosis or pulmonary embolism.
•Cardiovascular disease.
•Osteoporosis.
Investigations
•FSH only helpful if diagnosis is in doubt, such as below age 40 and levels in menopausal range (>30IU/L).
•Luteinizing hormone, oestradiol, and progesterone are of no value in the diagnosis of ovarian failure.
•Thyroid function tests (free T4 and thyroid-stimulating hormone) as abnormalities of thyroid function can be confused with menopausal symptoms.
•Testosterone levels are of uncertain value.
•BMD if significant risk factors for osteoporosis (Table 21.2).
|
|
MENOPAUSE: HISTORY TAKING AND INVESTIGATIONS |
641 |
|
|
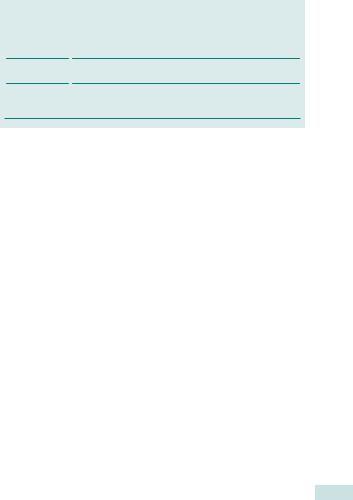
Table 21.2 Bone mineral density (BMD) |
|||
|
|
|
|
|
|
Description |
Definition |
||
|
|
|
|
|
|
Normal |
A person has a BMD value between −1 SD and +1 SD of |
||
|
|
the young adult mean (T score −1 to +1) |
||
|
Osteopenia |
A person has a BMD reduced between −1 and −2.5 SD |
||
|
|
from the young adult mean (T score −1 to −2.5) |
||
|
Osteoporosis |
A person has a BMD reduced by equal to or more than |
||
|
|
−2.5 SD from the young adult mean (T score −2.5 or |
||
lower)

642 CHAPTER 21 Menopause
Premature menopause
Ideally, premature menopause should be defined as menopause that occurs at an age more than 2SDs below the mean estimate for the reference population. The age of 40yrs is used frequently as an arbitrary limit below which the menopause is said to be premature. It affects 1% of women younger than 40yrs and 0.1% of those under 30yrs. In most cases no cause is found.
Causes of premature ovarian failure
Primary
•Chromosome abnormalities.
•FSH receptor gene polymorphism and inhibin B mutation.
•Enzyme deficiencies.
•Autoimmune disease.
Secondary
•Chemotherapy and radiotherapy.
•Bilateral oophorectomy or surgical menopause.
•Hysterectomy without oophorectomy.
•Infection.
Presentation and assessment
•The most common presentation is samenorrhoea or oligomenorrhoea (which may not necessarily be accompanied by hot flushes).
•Co-existing disease may be detected, particularly:
•hypothyroidism
•Addison’s disease
•diabetes mellitus
•any chromosome abnormalities (especially those who have not achieved successful pregnancy).
•The diagnostic usefulness of ovarian biopsy outside the research setting has yet to be proved.
Management issues in premature menopause
Fertility and contraception
•Reduced fertility.
•May require assisted conception.
•Need for contraception if no fertility goals.
2 Women need oestrogen replacement until average age of natural menopause, which is usually regarded as 52.
•HRT.
•COCP without gaps (back-to-back).
•No evidence regarding use of bisphosphonates, strontium ranelate, or raloxifene.
•No evidence regarding use of alternative and complementary therapies.

PREMATURE MENOPAUSE 643
Consequences of premature menopause
•Women with untreated premature menopause (no oestrogen replacement) are at increased risk of osteoporosis and cardiovascular disease, but at lower risk of breast malignancy.
•Premature menopause can lead to reduced peak bone mass (if <25yrs old) or early bone loss thereafter.
1 Mean life expectancy in women with menopause before the age of 40yrs is 2.0yrs shorter than that in women with menopause after the age of 55yrs.

644 CHAPTER 21 Menopause
Hormone replacement therapy: overview
More than 50 HRT preparations, which feature different strengths, combinations, and routes of administration, are available. HRT can be given either systemically for hot flushes and osteoporosis or vaginally (or topically) for local symptoms such as vaginal dryness. In non-hysterectomized women HRT consists of an oestrogen combined with a progestagen.
Oestrogens
Oestrogens used in HRT include oestradiol, oestrone, and oestriol, which, although chemically synthesized from soya beans or yams, are molecularly identical to the natural human hormone. Conjugated equine oestrogens containing about 50–65% oestrone sulphate, with the remainder being equine oestrogens (mainly equilin sulphate), are also used.
Progestagens
The progestagens used in HRT are almost all synthetic and derived from plant sources. They are structurally different from progesterone. 17-hydroxyprogesterone and 19-nortestosterone derivatives are the progestagens used most commonly in HRT.
17-Hydroxyprogesterone
•Dydrogesterone.
•Medroxyprogesterone acetate.
19-Nortestosterone derivatives
•Norethisterone.
•Levonorgestrel.
Other hormones used at the menopause
•Tibolone: is a synthetic steroid compound that itself is inert, but on absorption is converted to metabolites with oestrogenic,
progestagenic, and androgenic actions. It is classified as HRT in the British National Formulary. It is used in post-menopausal women.
•Testosterone: patches and implants may be used to improve libido.
Treatment of local symptoms
Some women do not wish to take, or cannot tolerate, systemic HRT and simply require relief of local symptoms, which are usually urogenital. Synthetic or conjugated equine oestrogens should be avoided, as they are well absorbed from the vagina. The options available are low-dose natural oestrogens, such as vaginal estriol by cream or pessary or estradiol by tablet or ring. Treatment is needed in the long term, if not lifelong, as symptoms return on cessation of treatment. With the recommended dose regimens, no adverse endometrial effects should be incurred, and a progestagen need not be added in non-hysterectomized women.

HORMONE REPLACEMENT THERAPY: OVERVIEW 645
Types of systemic oestrogen-based HRT
•Oestrogen alone in hysterectomized women.
•Oestrogen plus progestagen in non-hysterectomized women.
•oestrogen and cyclical progestagen in peri-menopausal women
•continuous combined oestrogen–progestagen (‘no bleed’ HRT) in post-menopausal women.
•Routes of administration of oestrogen:
•oral
•transdermal
•subcutaneous
•vaginal.
•Routes of administration of progestagen:
•oral
•transdermal
•intrauterine (levonorgestrel).
Minimum bone-sparing doses of HRT
•Estradiol oral: 1–2mg
•Estradiol patch: 25–50 micrograms
•Estradiol gel: 1–5g*
•Estradiol implant: 50mg every 6mths
•Conjugated equine estrogens: 0.3–0.625mg daily
*Depends on preparation: lower doses may be effective.
Side effects of systemic HRT
•Oestrogen-related: fluid retention, bloating, breast tenderness or enlargement, nausea, headaches, leg cramps, and dyspepsia.*
•Progestagen-related: fluid retention, breast tenderness, headaches or migraine, mood swings, depression, acne, lower abdominal pain, and backache.*
•Combined HRT: irregular, breakthrough bleeding (may need investigation).
•All types of HRT: weight gain (but not proved in randomized trials).
* Changing dose, type, and route of administration (tablet to patch) may help.

646 CHAPTER 21 Menopause
Hormone replacement therapy: benefits
Two large studies—randomized Women’s Health Initiative (WHI) and the observational Million Women Study (MWS)—undertaken in women aged >50 resulted in controversy about use of HRT. There are benefits and risks in its use, and some uncertainty concerning some claims made about HRT.
Benefits of HRT
•dVasomotor symptoms.
•dUrogenital symptoms and improved sexuality.
•dRisk of osteoporosis.
•dRisk of colorectal cancer.
Relief of vasomotor symptoms
•Oestrogen is effective in treating hot flushes:
•improvement usually is noted within 4wks
•maximum therapeutic response usually achieved by 3mths
•should be continued for at least 1yr or symptoms often recur
•the most common indication for a prescription of HRT
•often is used for fewer than 5yrs.
•Oestrogen more effective than SSRIs or clonidine (largely ineffective).
Urogenital symptoms and sexuality
•Urogential symptoms respond well to oestrogen (which may be given vaginally or systemically).
•Improvement may take several months.
•Long-term treatment often is needed, as symptoms can recur.
•Urinary incontinence is not improved by systemic therapy.
•Sexuality may be improved with oestrogen alone, but may need addition of testosterone, especially in young oophorectomized women.
Osteoporosis
•HRT dthe risk of spine and hip and other osteoporotic fractures.
•Most epidemiological studies suggest continuous and lifelong use is required for HRT to be an effective method of preventing fracture.
•The efficacy of alternatives such as bisphosphonates in peri-menopausal or early post-menopausal women remains uncertain.
•HRT is significantly cheaper than alternative therapies, such as bisphosphonates, strontium ranelate, and parathyroid hormone.
Colorectal cancer
•HRT dthe risk of colorectal cancer by about 1/3.
•Little known about risk when treatment is stopped or in high risk populations.
•Currently, prevention of colonic cancer is not an indication for HRT.
This page intentionally left blank

648 CHAPTER 21 Menopause
Hormone replacement therapy: risks
Risks of HRT
•iRisk of breast cancer.
•iRisk of endometrial cancer with unopposed oestrogen.
•iRisk of VTE.
•iRisk of gallbladder disease.
Endometrial cancer
•Unopposed oestrogen ithe risk of endometrial cancer:
•the relative risk (RR) is 2.3
•risk iwith prolonged use (RR 9.5 for ≥10yrs)
•risk remains ifor 5 or more years after stopping (RR 2.3).
•This risk is not eliminated completely with the addition of monthly sequential progestagen (especially if used for >5yrs).
•No irisk has been found with continuous combined HRT.
Venous thromboembolism
1 HRT more than doubles the risk of VTE, but absolute risk remains small.
•For non-users, over a 5yr period, the incidence of VTE will be:
•3:1000 women aged 50–59yrs
•8:1000 women aged 60–69yrs.
•The number of additional VTE events in healthy women on HRT ≥5yrs is estimated to be:
•4:1000 women aged 50–59yrs
•9:1000 women aged 60–69yrs.
•The VTE is more likely in the first year of HRT.
•iAge, obesity, and thrombophilia significantly irisk of VTE.
•Using HRT after VTE has irisk of recurrence in first year of use.
•Transdermal HRT may be associated with a lower risk than oral.
Gallbladder disease
XHRT appears to ithe risk of gallbladder disease, but:
•Risk iwith age and obesity.
•Women who use HRT may have silent pre-existing disease.

HORMONE REPLACEMENT THERAPY: RISKS 649
Risk of breast cancer with HRT
•HRT confers a similar degree of risk to late natural menopause:
•every year the menopause is naturally delayed, the risk iby 2.8%
•with HRT, the risk iby 2.3% per year.
•The risk is dependent on duration of HRT.
•The effect is not sustained once HRT is stopped: 5yrs after stopping, the risk is the same as for women who have never had HRT.
•The risk of breast cancer with HRT is dependent on the regimen:
•greatest with combined oestrogen–progestagen HRT
•less with unopposed oestrogen (but irisk of endometrial cancer).
1Combined HRT probably accounts for an extra 3 breast cancers per 1000 women who start it at the age of 50yrs and use it for 5yrs.
X All risk estimates are based on starting HRT at 50; this effect is not seen in women who start it early for premature menopause (therefore duration of exposure to female sex hormones is probably relevant).
X The increase in risk of breast cancer found in nulliparous women, those with a high BMI, those who delay their first birth, and those who have a family history may be higher than that conferred by HRT.
650 CHAPTER 21 Menopause
Hormone replacement therapy: uncertainties
Uncertainties concerning HRT
•Cardiovascular disease.
•Dementia.
•Ovarian cancer.
•Quality of life.
Cardiovascular disease
•The role of HRT in por sprevention is uncertain, and it should not be used primarily for this indication.
•The timing, dose, and possibly type of HRT, however, may be critical in determining cardiovascular effects: women in the WHI who started HRT within 10yrs of the menopause had a lower risk of coronary heart disease than women who started later.
Dementia and cognition
•Oestrogen may delay or dthe risk of Alzheimer’s disease, but it does not seem to improve established disease.
•It is unclear if there is a critical age to start HRT or an optimal duration of treatment to prevent dementia.
Ovarian cancer
•There is irisk in the very long term (>10yrs) with oestrogen alone.
•This risk is not seen with continuous combined therapy.
X This issue is unresolved and requires further examination. Currently insufficient evidence is available to recommend alterations in HRT prescribing practice.
Quality of life
XAlthough some studies have shown improvement in both symptomatic and asymptomatic women, others have not. This area is difficult to evaluate because of the different measures used, varying levels of menopausal symptoms, a large placebo effect, and extrinsic factors that may alter women’s responses.

ALTERNATIVE MEDICAL TREATMENTS TO HRT 651
Alternative medical treatments to hormone replacement therapy
Publication of the WHI and the MWS studies led to women stopping HRT and considering alternative medical treatments to eleviate menopausal symptoms.
Treatment of vasomotor symptoms
•SSRIs: fluoxetine and paroxetine.
•SNRI: venlafaxine.
•Clonidine (α-agonist): once mainstay treatment, but now shown as having limited effect.
Prevention and treatment of osteoporosis
Agent used to either inhibit bone resorption or stimulate bone formation.
•Calcium and vitamin D.
•Bisphosphonates (inhibits osteoclasts).
•Selective oestrogen reuptake modulators (SERMs).
Urogenital symptoms
•Oestrogen cream, an intra-vaginal sustained-release oestradiol ring, or oestradiol vaginal tablets are the most effective treatment for vaginal atrophy and dyspareunia.
•Patient can be reassured of minimal systemic absorption and no need for added progestagen.
•Alternative treatment to alleviate dyspareunia; vaginal lubricant and bio-adhesive moisturizers (Replens®).
This page intentionally left blank
