
- •contents
- •1 introduction
- •2 general points about renal biopsy specimens
- •3 technical handling of renal biopsy specimens
- •4 how to look at a renal biopsy specimen: preliminary study
- •5 how to look at a renal biopsy specimen: initial study of the kidney
- •6 indication for biopsy: nephrotic syndrome
- •7 indication for biopsy: acute renal failure
- •8 indication for biopsy: chronic renal failure
- •9 indication for biopsy: hematuria
- •10 indication for biopsy: proteinuria
- •11 indication for biopsy: renal allograft
- •12 other indications for biopsy of kidneys
- •index
Chapter 4
How to Look at a Renal Biopsy Specimen: Preliminary Study
Immediate Study of Initial Sections
When sections stained by hematoxylin and eosin are available, the pathologist should look at them immediately, before sections stained in other ways are ready.
This should be done whatever was the indication for biopsy. The reasons are these.
1.There may be no kidney in the specimen. A percutaneous renal biopsy is a more difficult procedure than biopsy of skin, or liver, or organs that can be seen by endoscopy. Blood and connective tissues including fat, fibrous tissue, nerves, skeletal muscle, and blood vessels are often found, with or without kidney. Hemosiderin deposits are common if there was a previous renal biopsy on the same side. Perls’ Prussian blue stain will confirm that these deposits contain iron, but this is not usually important.
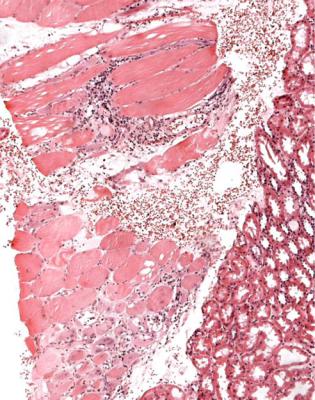
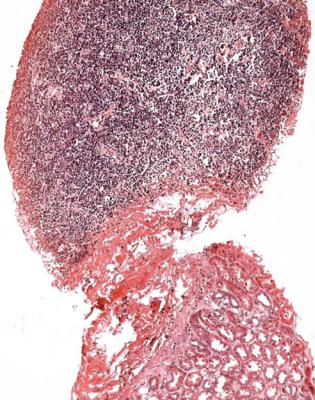
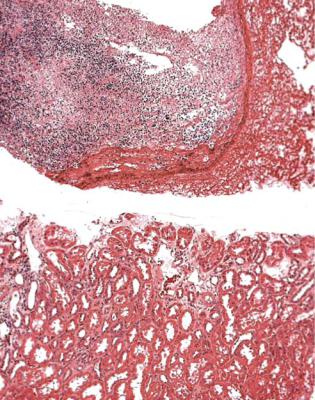
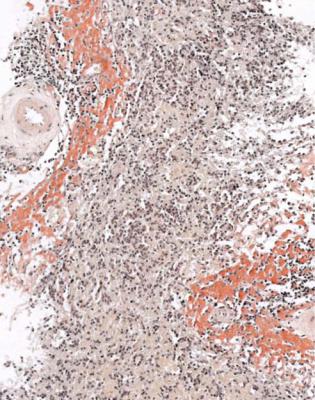
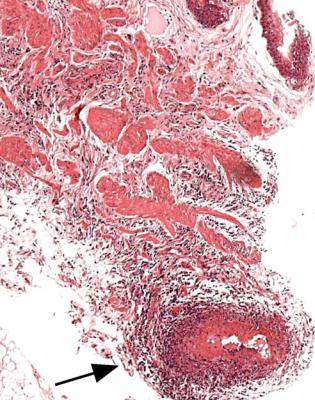
All tissues should be examined, whether or not there is kidney. Occasionally a significant abnormality can be detected outside the kidney, such as myositis (Fig. 4.1), or lymphoma (Fig. 4.2), or pus, which may be seen particularly around renal allografts (Fig. 4.3).
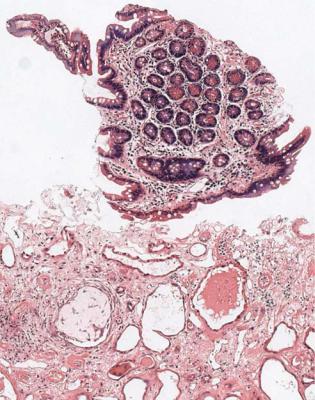
2.There may be other abdominal organs in the specimen, with or without kidney. The commonest is bowel, sometimes just muscle layers rather than full thickness with mucosa, and more often small intestine than large intestine (Fig. 4.4). Spleen and liver are seen less often. Adrenal gland, pancreas, and lymph node are uncommon. Skin is hardly ever seen, because the skin is cut to make an opening for the biopsy needle. All tissues should still be examined (Fig. 4.5).
3.The only parts of the kidney in the specimen may be medulla or renal pelvis.
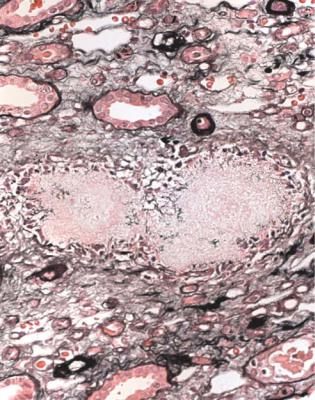
Occasionally, these may allow the pathologist to make a diagnosis, for instance if there is papillary necrosis, or amyloid, or vasculitis (Fig. 4.6). Usually cortex is needed to make a diagnosis, even if the medulla shows abnormalities such as deposits of pus or urate crystals (Fig. 4.7), because these can occur together with disorders that are not evident in the medulla.
4.There may be cortex in the specimen, but not much. Cortex is recognised by the presence of glomeruli and convoluted parts of tubules. The pathologist has
A. J. Howie, Handbook of Renal Biopsy Pathology. |
19 |
C Springer 2008 |
|
20 |
4 How to Look at a Renal Biopsy Specimen: Preliminary Study |
Fig. 4.1 Skeletal muscle included in a renal biopsy specimen from a woman of 34 with the nephrotic syndrome and a multisystem illness. There is active myositis. This and Figs 4.2–4.5 show that tissues as well as kidney in a specimen should always be examined
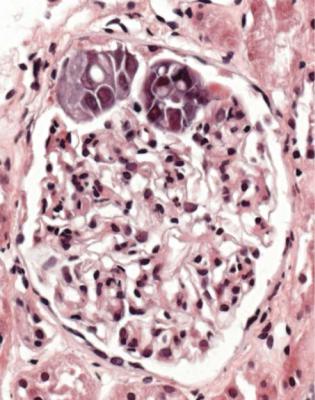
to judge the chances that a diagnosis will be made. No rule can say how much cortex is necessary for a diagnosis. One glomerulus, even without any other renal tissue, may be enough to allow a diagnosis of IgA nephropathy, or vasculitic glomerulonephritis, or membranous nephropathy, or diabetic glomerulopathy, or amyloid, among others (Fig. 4.8). A small sample of cortex may not be adequate for proper assessment of conditions such as suspected rejection of an allograft or suspected vasculitis.
Occasionally, there are recommendations about the minimum number of glomeruli or amount of cortex necessary to consider a renal biopsy specimen adequate. The answer to the question of what is an adequate specimen is “It depends”. It depends upon the clinical circumstances, and the pathologic findings. On some specimens, a satisfactory diagnosis may be given with hardly any glomeruli (Fig. 4.8), or without cortex (Fig. 4.6), or even without kidney (Fig. 4.5), while on others with many glomeruli and a large amount of cortex, the pathologist may not be able to give a satisfactory diagnosis. Some pathologists
Immediate Study of Initial Sections |
21 |
Fig. 4.2 Renal biopsy specimen from a man of 56 with the nephrotic syndrome, and an IgM paraprotein in serum. There is a lymphoplasmacytoid lymphoma outside the capsule of the kidney. The man had Waldenström’s macroglobulinemia, named after Jan Gosta Waldenström (1906–1996), a Swedish physician. In English, the name is often pronounced as it looks, wall-den-strome, which is not the Swedish pronunciation
are more ready than others to call a specimen inadequate, but as much useful information as possible should always be given on a specimen, which may be the only one ever available.
5.There may be findings in the specimen that could have an influence on immediate clinical management. These could be expected or unexpected. Often in acute renal failure, a renal biopsy is taken to investigate the possibility of renal vasculitis, which is a nephrologic emergency. Vasculitis is usually easy to diagnose on sections stained by hematoxylin and eosin. Similarly, biopsy of an allograft is usually taken to see whether there is active rejection, which may be treated immediately. These are among the few occasions when a pathologist can have an important role in urgent clinical problems. Occasionally, unexpected findings of immediate significance are seen. For example, neoplasms are sometimes found by surprise (Fig. 4.9).
22 |
4 How to Look at a Renal Biopsy Specimen: Preliminary Study |
Fig. 4.3 Needle biopsy specimen of a renal allograft in a woman of 25, three months after transplantation. The specimen includes hemorrhagic pus from around the kidney, which has no evidence of significant rejection
Immediate Study of Initial Sections |
23 |
Fig. 4.4 Small intestine included in a renal biopsy specimen from a man of 69 with renal failure, which clinically seemed acute. The kidney has late damage from tubular effects of myeloma
24 |
4 How to Look at a Renal Biopsy Specimen: Preliminary Study |
Fig. 4.5 Attempted renal biopsy in a man of 54 with the nephrotic syndrome and psoriatic arthropathy. There is no kidney in the specimen, but there is spleen, and this contains amyloid stained by Congo red, shown to be AA amyloid. The nephrotic syndrome was assumed to be due to AA amyloidosis. Amyloid, from Greek words meaning starch and resembling or like, is sometimes mistakenly considered one of the many words invented by Rudolf Ludwig Karl Virchow (1821–1902), called the greatest figure in the history of pathology by E R Long in A History of Pathology, 1928. Virchow apparently pronounced his surname feer-cho, with the ch as the Scottish pronounce it in loch, but several other pronunciations are used in English. The word amyloid was first used by two Germans J Vogel and M J Schleiden in 1839, because of the similar staining properties of cellulose and starch. Virchow showed that waxy or lardaceous change of the spleen was due to amyloid, which he thought was a cellulose like meterial
Immediate Study of Initial Sections |
25 |
Fig. 4.6 Renal biopsy specimen from a man of 53 with hematuria, proteinuria, upper respiratory tract abnormalities, and a high titer of antineutrophil cytoplasmic antibodies. There is only renal pelvis in the specimen, but this shows acute arteritis, arrowed
26 |
4 How to Look at a Renal Biopsy Specimen: Preliminary Study |
Fig. 4.7 Medulla in a renal biopsy specimen from a man of 50. The cortex shows late changes of IgA nephropathy. There is an amorphous mass surrounded by inflammatory cells, with the appearances of urate deposits. The crystals do not remain after fixation and processing. Medulla meant marrow in Latin

Immediate Study of Initial Sections |
27 |
Fig. 4.8 Renal biopsy specimen from a man of 67 with chronic renal failure and proteinuria. There is only one glomerulus in the specimen, arrowed, but immunoperoxidase staining shows that this contains IgA, and gives the diagnosis of IgA nephropathy
28 |
4 How to Look at a Renal Biopsy Specimen: Preliminary Study |
Fig. 4.9 Wedge biopsy specimen taken at the time of transplantation of a cadaveric kidney from a man of 45 into a man of 61. A glomerulus contains metastatic carcinoma. This finding had an immediate effect on clinical management. The story is given in Barnes AD, Fox M. Transplantation of tumour with a kidney graft. British Medical Journal 1976; 1: 1442–1444
Actions After Immediate Study of Initial Sections
Actions to take are these.
1.If there is a possibility that further sections may help to show more cortex, these should be requested from the laboratory. If there is no kidney in the specimen, immediate inspection should prevent the laboratory from wasting time and resources on unnecessary staining.
2.If a diagnosis is unlikely to be made, usually because there is no cortex in the specimen, or if an organ other than kidney is seen, the nephrologists or surgeons should be told immediately. They may wish to repeat the biopsy if there
Summary: How to Look at a Renal Biopsy Specimen: Preliminary Study |
29 |
is no cortex, and will be prepared if there is a clinical problem from damage to the bowel, or spleen, or other organ.
3.Nephrologists or surgeons should be told about findings in a biopsy specimen taken for an urgent indication, even if only a provisional diagnosis is possible. They should also be told about unexpected findings likely to be of clinical importance.
Summary: How to Look at a Renal Biopsy Specimen: Preliminary Study
The pathologist should look immediately at sections of a renal biopsy specimen stained by hematoxylin and eosin, because the findings may be of clinical or technical importance.
All tissues in a specimen should be examined, even if there is no cortex. Judgment should be used by the pathologist to decide whether the specimen is
adequate to allow a diagnosis to be made, given the clinical circumstances and the pathologic findings.
