
Полезные материалы за все 6 курсов / Учебники, методички, pdf / Kaplan Pediatrics USMLE 2CK 2021
.pdf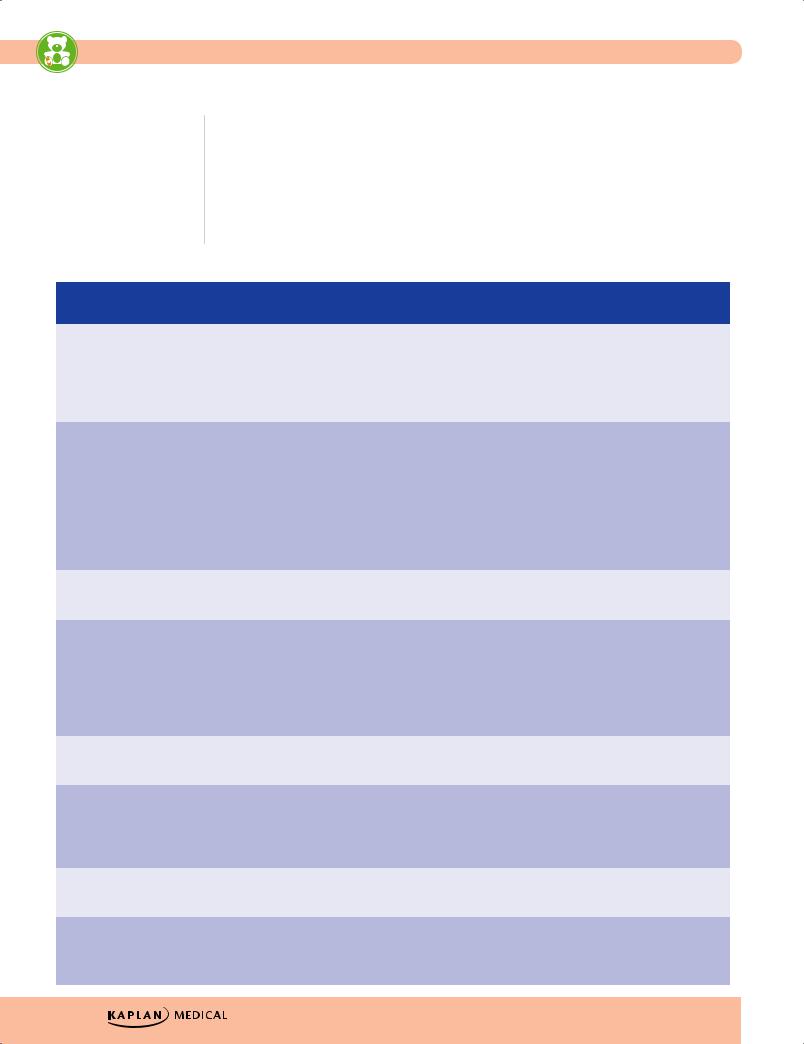
USMLE Step 2 CK λ Pediatrics
•Treatment of hyperbilirubinemia
–Phototherapy
°Complications: loose stools, erythematous macular rash, overheating leading to dehydration, and bronze baby syndrome (occurs with direct hyperbilirubinemia; dark, grayish-brown discoloration of the skin [photo-induced change in porphyrins, which are present in cholestatic jaundice])
–Double volume exchange transfusion—if bilirubin continues to rise despite intensive phototherapy and/or kernicterus is a concern
Table 1-7. Hyperbilirubinemia and Jaundice
|
|
|
|
Reason for |
|
|
|
|
|
Hgb, Hct/ |
|
|
|
|
|
|
|
|
Etiology |
|
|
Hyperbilirubinemia |
|
|
Other labs |
|
|
Treatment |
|
||||||
|
|
|
increased bilirubin |
|
|
|
|
Reticulocytes |
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Excessive |
RBCs → Hgb → |
Indirect |
• Normal to |
|
|
|
Phototherapy |
||||||||||
bruising/ |
Bilirubin |
|
|
|
|
slightly low |
|
|
|
|
|
|
|||||
cephalohematoma |
|
|
|
|
|
|
|
Hgb/Hct |
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
• Normal to |
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
slight increase |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
in reticulocytes |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Immune hemolysis |
Anti-Rh, anti-A, |
Indirect |
• Low Hgb/Hct |
• Rh negative |
Phototherapy + |
||||||||||||
• Rh |
anti-B, anti-minor |
|
|
|
|
(anemia) |
|
mother and Rh |
possible ex- |
||||||||
• ABO |
blood group Abs |
|
|
|
• Increased |
|
positive baby |
change transfu- |
|||||||||
• Minor blood |
|
|
|
|
|
|
|
reticulocytes |
• Type O mother |
sion |
|||||||
|
groups |
|
|
|
|
|
|
|
|
|
|
and type A or B |
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
baby |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• Direct Coombs |
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
positive |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• Decreased RBCs |
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Polycythemia |
High Hct, Hgb → high |
Indirect |
High (Hct >65)/ |
Increased RBCs |
Phototherapy + |
||||||||||||
|
|
|
bilirubin |
|
|
|
normal |
|
|
|
partial exchange |
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
transfusion |
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Non-immune |
Abnormal RBC → |
Indirect |
Low (anemia)/ |
• If no membrane |
Phototherapy + |
||||||||||||
hemolysis |
splenic removal |
|
|
|
increased |
|
defect →, G6PD, |
transfusion |
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
PK activity |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• Characteristic |
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
RBCs if |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
membrane defect |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• Decreased RBCs |
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Displacement of |
Free bilirubin in |
Indirect |
Normal |
|
|
|
Treat underlying |
||||||||||
bound bilirubin |
circulation |
|
|
|
|
|
|
|
|
|
problem |
||||||
from albumin |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Familial |
Absence of glucuronyl |
Indirect |
Normal |
GT activity |
Phototherapy + |
||||||||||||
nonhemolytic |
transferase (type I) vs. |
|
|
|
|
|
|
|
|
|
exchange |
||||||
hyperbilirubinemia |
small amount of |
|
|
|
|
|
|
|
|
|
transfusion |
||||||
(Crigler-Najjar |
inducible GT (type II) |
|
|
|
|
|
|
|
|
|
|
|
|
||||
syndrome) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Extrahepatic |
Bilirubin cannot leave |
Direct |
Normal |
Ultrasound, liver |
Portojejunos- |
||||||||||||
obstruction— |
the biliary system |
|
|
|
|
|
|
biopsy |
tomy, then later |
||||||||
biliary atresia |
|
|
|
|
|
|
|
|
|
|
|
|
liver transplant |
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Cholestasis |
Abnormal hepatic |
Direct |
Normal |
With H and P, other |
Treat underlying |
||||||||||||
(TORCH, sepsis, |
function → decrease |
|
|
|
|
|
|
select labs |
problem |
||||||||
metabolic, |
bilirubin excretion |
|
|
|
|
|
|
suggestive of |
|
|
|
||||||
endocrine) |
|
|
|
|
|
|
|
|
|
underlying etiology |
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
14
Chapter 1 λ The Newborn
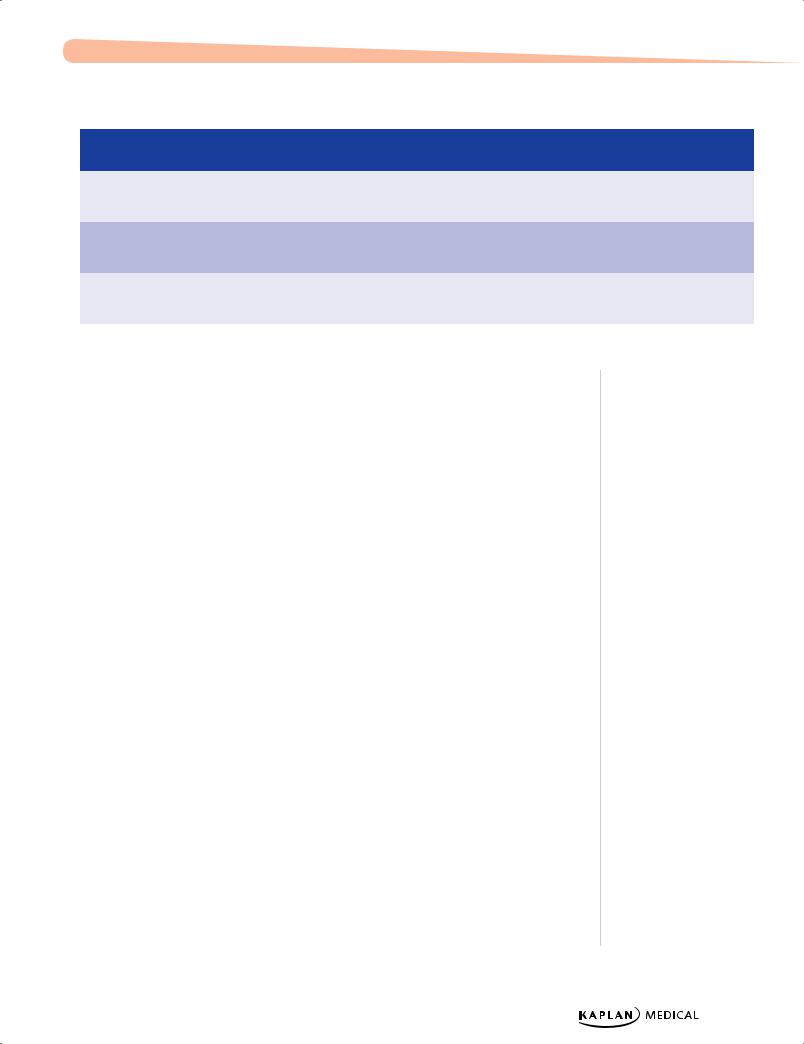
Table 1-7. Hyperbilirubinemia and Jaundice (Cont’d)
|
|
|
|
Reason for |
|
|
|
|
|
Hgb, Hct/ |
|
|
|
|
|
|
|
|
Etiology |
|
|
Hyperbilirubinemia |
|
|
Other labs |
|
|
Treatment |
|
||||||
|
|
|
increased bilirubin |
|
|
|
|
Reticulocytes |
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Bowel obstruction |
Increased |
Indirect |
Normal |
|
|
|
Relieve obstruc- |
||||||||||
|
|
|
enterohepatic |
|
|
|
|
|
|
|
|
|
tion + photother- |
||||
|
|
|
recirculation |
|
|
|
|
|
|
|
|
|
apy |
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Breastfeeding |
Increased |
Indirect |
Normal |
|
|
|
Phototherapy + |
||||||||||
jaundice |
enterohepatic |
|
|
|
|
|
|
|
|
|
hydration + teach |
||||||
|
|
|
recirculation |
|
|
|
|
|
|
|
|
|
breastfeeding |
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Breast milk |
Increased |
Indirect |
Normal |
|
|
|
Phototherapy + |
||||||||||
jaundice |
enterohepatic |
|
|
|
|
|
|
|
|
|
continued |
||||||
|
|
|
recirculation |
|
|
|
|
|
|
|
|
|
breastfeeding |
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
INFECTIONS
Neonatal Sepsis
A 3-week-old infant presents with irritability, poor feeding, temperature of 38.9 C (102 F), and grunting. Physical examination reveals a bulging fontanel, delayed capillary refill, and grunting.
•Signs and symptoms are very nonspecific.
•Risk factors
–Prematurity
–Chorioamnionitis
–Intrapartum fever
–Prolonged rupture of membranes
•Early onset: first week of life; maternal factors
–Chorioamnionitis
–Organisms: group B Streptococcus, E. coli, Listeria monocytogenes
•Late onset: second week through end of neonatal period; hospital or communityacquired organisms (if still hospitalized: iatrogenic infection)
–Most common organism: coagulase negative S. aureus (epidermidis)
•Diagnosis—sepsis workup: CBC, differential and platelets, blood culture, urine analysis and culture, chest x-ray; lumbar puncture only for neonates with severe signs (lethargy, hypothermia, hypotonia, poor perfusion, apnea, abnormal neurological findings, or clinical deterioration from birth)
•Treatment
–If no evidence of meningitis: ampicillin and aminoglycoside until 48–72-hour cultures are negative
–If meningitis or diagnosis is possible: ampicillin and third-generation cephalosporin (not ceftriaxone)
Note
In recent years studies have proven that in the first year of life, lumbar puncture reveals almost no cases of meningitis. Therefore, lumbar puncture should be reserved only for neonates with severe signs.
Published by dr-notes.com |
15 |
|
|
|
|
USMLE Step 2 CK λ Pediatrics
Note
Toxoplasmosis
Other (syphilis, varicella, HIV, and parvovirus B19)
Rubella Cytomegalovirus (CMV) Herpes
Transplacental Intrauterine Infections (TORCH)
TORCH infections are typically acquired in first or second trimester. Most infants have IUGR.
Toxoplasmosis
Toxoplasmosis is a maternal infection worldwide, due primarily to ingestion of undercooked or raw meat containing tissue cysts. Ingestion of water or food with oocytes that have been excreted by infected cats (fecal contamination) is the most common form of transmission in the United States. Advise pregnant women not to change/clean cat litter while pregnant.
•Findings
–Jaundice, hepatosplenomegaly
–Thrombocytopenia, anemia
–Microcephaly
–Chorioretinitis
–Hydrocephalus
–Intracranial calcifications
–Seizures
•Outcomes
–Psychomotor retardation
–Seizure disorder
–Visual impairments
•Treatment—maternal treatment during pregnancy reduces the likelihood of transmission significantly (spiramycin)
–Infants are treated with pyrimethamine, sulfadiazine, and leucovorin.
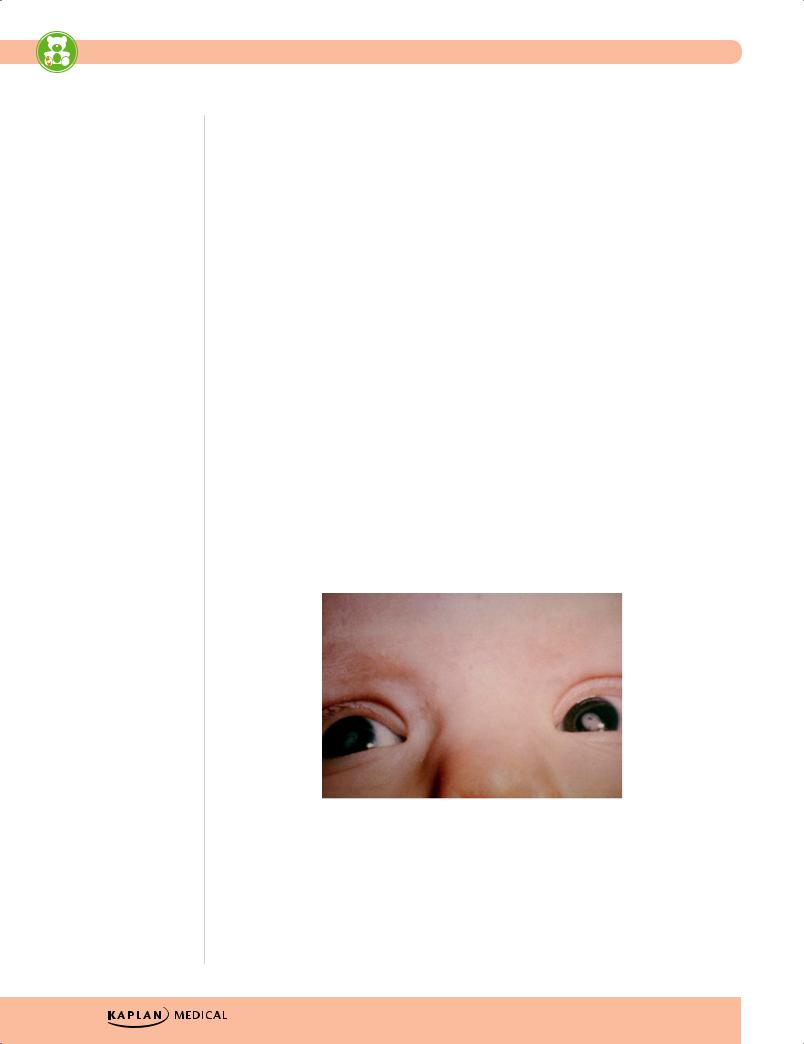
phil.cdc.gov
Figure 1-3. Congenital Cataract Secondary to Maternal Rubella Infection
16
Chapter 1 λ The Newborn
Congenital rubella
•Classic findings when maternal infection occurs in first 8 weeks’ gestation.
•Findings
–Blueberry muffin spots (extramedullary hematopoiesis), thrombocytopenia
–Cardiac—PDA, peripheral pulmonary artery stenosis
–Eye—cataracts
–Congenital hearing loss
–Thrombocytopenia
–Hepatosplenomegaly
•Outcomes
–Hearing loss
–Persistent growth retardation
–Microcephaly
–Mental and motor retardation
Cytomegalovirus (CMV)
•Primary infection (higher risk of severe disease) or reactivation of CMV
•Findings
–Hepatosplenomegaly, jaundice
–Periventricular calcifications
–Intrauterine growth retardation
–Chorioretinitis
–Microcephaly
–Thrombocytopenia, hemolytic anemia
•Outcomes
–Sensorineural hearing loss
–Neuromuscular abnormalities
–Intellectual disability
Herpes simplex
•Keratoconjunctivitis, skin (5–14 days), CNS (3–4 weeks), disseminated (5–7 days)
•Best diagnosis: PCR, any body fluid
•Best treatment: IV acyclovir ASAP
•Outcomes
–Microcephaly, spasticity
–Deafness
–Blindness
–Seizure disorder
–Psychomotor retardation
–Death
•Prevention is elective Cesarean section when active disease or visible lesions are identified; however, this is not 100% effective.
•Treatment—acyclovir
Published by dr-notes.com |
17 |
|
|
|
|
USMLE Step 2 CK λ Pediatrics
Congenital syphilis
•Transplacental transmission usually during second half of gestation
•At-risk infants must undergo serologic testing at the time of delivery.
•Findings
–Early (birth–2 yrs): snuffles, maculopapular rash (including palms of soles, desquamates), jaundice, periostitis, osteochondritis, chorioretinitis, congenital nephrosis
–Late (>2 years of age): Hutchinson teeth, Clutton joints, saber shins, saddle nose, osteochondritis, rhagades (thickening and fissures of corners of mouth)
•Diagnosis—Treponema in scrapings (most accurate test) from any lesion or fluid, serologic tests
–Infant with positive VDRL plus pathognomonic signs; if not, perform serial determinations—increasing titer in infection
–Most helpful specific test is IgM-FTA-ABS (immunoglobin fluorescent treponemal antibody absorption) but it is not always positive immediately.
•Treatment—penicillin
Varicella
•Neonatal
–Seen when delivery occurs <1 week before/after maternal infection
–Treat with VZIG (varicella zoster immune globulin), if mother develops varicella 5 days before to 2 days after delivery.
•Congenital
–Associated with limb malformations and deformations, cutaneous scars, microcephaly, chorioretinitis, cataracts, and cortical atrophy
–Associated with infection during 1st or 2nd trimester
Many of the findings of the TORCH infections are very similar, so note the most likely presentations:
• Toxoplasmosis: hydrocephalus with generalized calcifications and chorioretinitis • Rubella: the classic findings of cataracts, deafness, and heart defects
• CMV: microcephaly with periventricular calcifications; petechiae with thrombocytopenia; hepatosplenomegaly; sensorineural hearing loss
• Herpes: skin vesicles, keratoconjunctivitis, acute meningoencephalitis
• Syphilis: osteochondritis and periostitis; skin rash involving palms and soles and is desquamating; snuffles (mucopurulent rhinitis)
18
Chapter 1 λ The Newborn
Clinical Recall
Which of the following TORCH infections is correctly matched to an associated finding?
A.Rubella: patent ductus arteriosus
B.CMV: maculopapular rash
C.Herpes simplex: chorioretinitis
D.Congenital syphilis: periventricular calcifications
E.Varicella: snuffles
Answer: A
Published by dr-notes.com |
19 |
|
|
|
|

Genetics/Dysmorphology 2
Chapter Title
Learning Objectives
Demonstrate understanding of chromosome abnormalities
Solve problems concerning early overgrowth with associated defects, defects with facial features as the major defect, osteochondrodysplasias, and disorders of connective tissue
Explain information related to unusual brain and/or neuromuscular findings with associated defects
ABNORMALITIES OF CHROMOSOMES
Trisomy 21 (Down Syndrome)
Down syndrome is the most common pattern of human malformation.
•Genetics
–94% full trisomy 21(nondisjunction); risk of recurrence 1–2% and then increases with advancing maternal age
–4–6% with translocation; most are new mutations but must obtain parental karyotypes for possible balanced translocation carrier
•Findings
–Upward slanting palpebral fissures; speckling of iris (Brushfield spots); inner epicanthal folds
–Small stature, mouth open with tongue protrusion; mild microcephaly, short neck, flat occiput, short metacarpals and phalanges; single palmar crease
–Hypotonia
–Hearing loss (sensorineural, conductive, and mixed)
–Primary gonadal deficiency
–Cardiac anomaly—ECD > VSD > PDA, ASD; also MVP
–GI anomalies: duodenal atresia, Hirschsprung
–Atlanto-axial instability
–Hypothyroidism
–Acute lymphocytic leukemia (but acute myeloblastic leukemia if in first 3 years of life)
–Intellectual disability, variable
Cardiac Abbreviations
ASD: atrial septal defect
ECD: endocardial cushion defect
MVP: mitral valve prolapse
PDA: patent ductus arteriosus
VSD: ventricular septal defect
Published by dr-notes.com |
21 |
|
|
|
|

USMLE Step 2 CK λ Pediatrics
•Natural history
–Major cause for early mortality is congenital heart disease
–Muscle tone improves with age
–Rate of development slows with age
–Early onset of Alzheimer disease
Trisomy 18 (Edwards Syndrome)
Edwards syndrome is the second most common pattern of human malformation.
•Genetics—older maternal age; nondisjunction
•Findings
–Growth deficiency
–Intellectual disability
–Low-set, malformed ears; microcephaly, micrognathia; prominent occiput
–Clenched hand—index over third; fifth over fourth
–Short sternum
–VSD, ASD, PDA, cyanotic lesions,
–Rocker-bottom feet, hammertoe
–Omphalocele
•Natural history
–Many spontaneous abortions
–Feeble from birth
–Most do not survive first year
Trisomy 13 (Patau Syndrome)
Patau syndrome is a defect of midface, eye, and forebrain development → single defect in first 3 weeks’ development of prechordal mesoderm. It involves older maternal age.
•Findings
–Holoprosencephaly and other CNS defects
–Severe intellectual disability
–Microcephaly; microphthalmia
–Severe cleft lip, palate, or both
–Scalp defects in parietal-occipital area (cutis aplasia)
–Postaxial polydactyly
–VSD, PDA, ASD, cyanotic lesions
–Single umbilical artery
Aniridia–Wilms Tumor Association (WAGR Syndrome)
•Genetics
–1/70 with aniridia also has Wilms
–WAGR syndrome: deletion of 11p13; Wilms + Aniridia + GU anomalies + MR
–Have 45–60% chance of developing Wilms tumor
22
Chapter 2 λ Genetics/Dysmorphology
Klinefelter Syndrome (XXY)
•Genetics; most common findings manifested at puberty
•Findings
–Decreased IQ (average IQ 85−90)
–Behavioral/psychiatric problems
–Long limbs (decreased upper:lower segment ratio)
–Slim (weight/height ratio low)
–Hypogonadism and hypogenitalism (testosterone replacement at age 11−12 years) = hypergonadotropic hypogonadism (increased FSH and LH, and decreased testosterone)
–Infertility in almost all
–Gynecomastia
Turner Syndrome (XO)
•Genetics
–Generally sporadic; no older maternal age seen
–Paternal chromosome more likely to be missing
–Many mosaic patterns (including Y-chromatin)
•Findings
–Small-stature female
–Absence of one SHOX gene (short stature homeobox; embryonic regulation of skeletal system, especially arms and legs)
–Abnormal GH–IGF receptor axis
–Gonadal dysgenesis–streak ovaries in XO
–Average IQ 90
–Congenital lymphedema, residual puffiness over dorsum of fingers and toes
–Broad chest, wide-spaced nipples
–Low posterior hairline; webbed posterior neck
–Cubitus valgus (elbow) and other joint problems
–Horseshoe kidney and other renal defects
–Cardiac:
°Bicuspid aortic valve (number 1 cardiac anomaly)
°Coarctation (Turner syndrome is the condition in which this is seen most often, but it is not the most common cardiac condition in Turner syndrome)
°Aortic stenosis, mitral valve prolapse
°Hypertension common, even without cardiac or renal disease
–Primary hypothyroidism, mostly autoimmune, and other autoimmune diseases (celiac disease)
•Natural history
–Decreased height velocity with delayed bone age
–Estrogen treatment indicated
–May increase height by 3−4 cm with growth hormone (GH)
Note
Gonadal dysgenesis is not evident in childhood, so chromosomes are warranted in any short-stature female whose phenotype is compatible with Turner syndrome.
Also consider in any adolescent with absent breast development by age 13, pubertal arrest, or primary/secondary amenorrhea with increased FSH.
Published by dr-notes.com |
23 |
|
|
|
|
