
Gale Encyclopedia of Genetic Disorder / Gale Encyclopedia of Genetic Disorders, Two Volume Set - Volume 2 - M-Z - I
.pdf
boxylase deficient individual, all the glucose required by the body must be ingested. This causes a glucose shortage that leads to low blood sugar (hypoglycemia) and a progressive degeneration of the tissues, with the most profound effects observed in the brain and central nervous system, since these tissues are the most reliant on the use of glucose for energy.
Pyruvate carboxylase is also important in the process that removes excess nitrogen from the body (the urea cycle). Since pyruvate carboxylase deficient individuals do not have sufficient quantities of pyruvate carboxylase, they develop a build-up of nitrogen, in the form of ammonia, in the bloodstream and the tissues.
Genetic profile
The gene that is responsible for the production of pyruvate carboxylase has been localized to a small region of chromosome 11. There are at least three mutations in this gene that lead to type B PCD. There is only one known mutation that leads to type A PCD.
Both types of PCD are transmitted via a recessive trait which means that both parents must be carriers of the mutation in order for it to occur in their children. In the case of parents with one child affected with PCD, the likelihood that a second child will be affected with PCD is 25%.
Demographics
PCD is estimated to occur in approximately one in every 250,000 live births, although only 39 cases had been described in the literature prior to 2001.
Type A PCD is also called North American PCD because it occurs almost exclusively in Algonquin lan- guage-speaking Native North Americans. In the Micmac, Cree, and Ojibwa tribes of Canada, it is estimated that as high as one in 10 individuals are carriers of the mutation that causes type A PCD. This suggests a founder effect in these populations. A founder effect is a genetic term that means a single individual brought a mutation into a subpopulation at a time when the subpopulation was quite small. As a result, a large majority of the members of the subpopulation carry the mutation derived through direct ancestry to this one individual.
Type B PCD is also called French PCD because it has a much higher incidence among the French than among any other subpopulation.
Signs and symptoms
Type A, or infantile onset, PCD may be fatal prior to birth, or it may not present any symptoms until approximately three months of age. These individuals
K E Y T E R M S
Allelic variants—A disease is said to have allelic variants when different mutations in the same allele result in identical, or nearly identical, symptoms. An allele is the combined locations of a gene on the two paired chromosomes that contain this gene.
Autosomal—Relating to any chromosome besides the X and Y sex chromosomes. Human cells contain 22 pairs of autosomes and one pair of sex chromosomes.
Biotin—A growth vitamin of the vitamin B complex found naturally in liver, egg yolks, and yeast.
Enzyme efficiency—The rate at which an enzyme can perform the chemical transformation that it is expected to accomplish. This is also called turnover rate. Individuals affected with type A PCD produce an enzyme that is much slower than the normal pyruvate carboxylase enzyme.
Necrotizing encephalomyelopathy—A progressive degeneration of the brain and central nervous system. This condition is fatal in nearly all individuals affected with type A pyruvate carboxylase deficiency.
Pyruvate carboxylase—The enzyme that is responsible for the first step in the conversion of pyruvate molecules into glucose molecules. Individuals with type A PCD produce a highly inefficient form of pyruvate carboxylase. Individuals with type B PCD either completely lack the ability to produce this enzyme, or they cannot produce it in sufficient quantities to sustain life.
will show severe physical and mental delay. Additionally, children affected with type A PCD have a progressive degeneration of the entire brain and nervous system (necrotizing encephalomyelopathy) that eventually leads to death.
Type B, or neonatal, PCD is generally fatal prior to birth. In the rare instances of a liveborn child affected with type B PCD, severe growth delay (extremely low birth weight) and severe mental impairment are to be expected. Children born with type B PCD will fail to thrive and generally do not survive past the first three months of life.
Diagnosis
PCD is diagnosed primarily through blood tests to determine the blood concentrations of lactate and pyru-
deficiency carboxylase Pyruvate
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
971 |

Pyruvate dehydrogenase complex deficiency
vate. Extremely high levels of both of these chemicals in the blood indicate that a congenital problem in cellular metabolism is most likely present. PCD is often differentiated from other cellular metabolic disorders by the extreme speed with which glucose levels in the blood drop during fasting (fasting hypoglycemia) and the abnormally low levels of the chemical aspartic acid in the blood.
PCD can be tested prenatally by measuring the activity of pyruvate carboxylase in chorionic villi samples.
Treatment and management
Administration of aspartic acid has been successful in decreasing the pyruvate and lactate concentrations in the blood of some PCD affected individuals. But, this treatment does not repair the damage to the pyruvate carboxylase enzyme, so progressive degeneration of the nervous system is slowed only slightly and the outcome is still death.
Biotin (a B-complex vitamin) is a coenzyme to pyruvate carboxylase. It has been shown that type B PCD is responsive to treatment with biotin while type A is not. Therefore, in the rare instance of a liveborn child with type B PCD, life may be extended through the administration of biotin.
Prognosis
Without prenatal administration of enzyme replacement therapy (which is currently not available), in which the developing fetus is given an artificial form of pyruvate carboxylase, individuals affected with either type A or type B PCD will die either prior to birth or, generally, within the first six months of life. Without prenatal enzyme replacement therapy, most children affected with PCD are born with such brain and nervous system dysfunction that a decision has to be made about treatment to sustain life.
Resources
BOOKS
Al-Essa, M. A., and P. T. Ozand. Manual of Metabolic Disease. Riyadh, Saudi Arabia: King Faisal Specialist Hospital and Research Centre, 1998.
PERIODICALS
Brun, N., et al. “Pyruvate carboxylase deficiency: prenatal onset of ischemia-like brain lesions in two sibs with the acute neonatal form.” American Journal of Medical
Genetics (May 1999): 94–101.
Van Costner, R. N., S. Janssens, and J. P. Mission. “Prenatal diagnosis of pyruvate carboxylase deficiency by direct measurement of catalytic activity on chorionic villi samples.” Prenatal Diagnosis (October 1998): 1041–4.
ORGANIZATIONS
Children Living with Inherited Metabolic Diseases. The Quadrangle, Crewe Hall, Weston Rd., Crewe, Cheshire, CW1-6UR. UK 127 025 0221. Fax: 0870-7700-327.http://www.climb.org.uk .
United Mitochondrial Disease Foundation. PO Box 1151, Monroeville, PA 15146-1151. (412) 793-8077. Fax: (412) 793-6477. http://www.umdf.org .
WEBSITES
American Medical Association at New York University School of Medicine. http://endeavor.med.nyu.edu/student-org/ ama/docs/mgb1999-2000/ab12.htm .
International Mitochondrial Disease Network.http://www.imdn.org/index.html . (27 February 2001).
Online Mendelian Inheritance in Man (OMIM). http://www
.ncbi.nlm.nih.gov/htbin-post/Omim/dispmim?266150 . “Pyruvate carboxylase deficiency.” eMedicine http://www
.emedicine.com/ped/topic1967.htm .
Paul A. Johnson
I Pyruvate dehydrogenase complex deficiency
Definition
Pyruvate dehydrogenase complex deficiency (PDHA) is a genetic disorder that results in a malfunctioning of the Krebs, or tricarboxylic acid (TCA), cycle. It is sex-linked and appears to be a dominant trait.
Description
PDHA is one of the most common of the genetic disorders that cause abnormalities of mitochondrial metabolism. The mitochondria are the organelles inside cells that are reponsible for energy production and respiration at the cellular level. One of the most important processes in the mitochondria is the TCA cycle (also known as the Krebs cycle). The TCA cycle produces the majority of the ATP (chemical energy) necessary for maintenance (homeostasis) of the cell. The production of this ATP is accomplished by chemically converting molecules of the chemical pyruvate into carbon dioxide, water, and ATP. After a blood sugar (glucose) molecule has been broken down into two pyruvate molecules, one of two things will occur: if energy is required by the cell, the molecules will be further broken down into ATP, carbon dioxide, and water; or, if energy is not needed by the cell, the pyruvate molecules will be put back together to
972 |
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
reform a glucose molecule. These transformations of pyruvate are accomplished primarily by two enzymes: pyruvate carboxylase, an enzyme that converts pyruvate molecules into oxaloacetate molecules in preparation to reform glucose molecules; and pyruvate dehydrogenase (PDH), an enzyme that begins the breakdown of the pyruvate into the eventual products of carbon dioxide, water, and ATP. To break down the pyruvate, PDH gets some help from two other enzymes: dihydrolipoyl transacetylase and dihydrolipoyl dehydrogenase. These three enzymes and the five coenzymes (CoA, NAD+, FAD+, lipoic adic, and TPP) that assist these enzymes are collectively known as the pyruvate dehydrogenase complex (PDH complex).
Individuals affected with PDHA have deficiencies in one or more of the three enzymes within the PDH complex. Most have a deficiency of the PDH enzyme itself. Tissues that require the greatest amounts of oxygen (highly aerobic tissues), such as those of the brain and the rest of the central nervous system, are most sensitive to deficiencies in the PDH complex.
People with PDHA have either a complete inability or a severely limited ability to produce PDH. Since these individuals cannot produce the amounts of PDH required to break down pyruvate, the cells cannot produce enough energy, in the form of ATP, to maintain themselves. This causes a progressive degeneration of the tissues, with the most profound effects observed in the brain and central nervous system.
PDH is an enzyme. An enzyme is a chemical that facilitates (catalyzes) the chemical reaction of another chemical or of other chemicals; it is neither a reactant nor a product in the chemical reaction that it facilitates (catalyzes). As a result, enzymes are not used up in chemical reactions; they are recycled. One molecule of an enzyme may be used to facilitate (catalyze) the same chemical reaction over and over again several hundreds of thousands of times. All the enzymes necessary for catalyzing the various reactions of human life are produced within the body by genes. Genetic enzyme deficiency disorders, such as PDHA, result from only one cause: the affected individual cannot produce enough of the necessary enzyme because the gene designed to make the enzyme is faulty. Enzymes are not used up in chemical reactions, but they do eventually wear out, or accidentally get expelled. Also, as an individual grows, they may require greater quantities of an enzyme. Therefore, most enzyme deficiency disorders will have a time component to them. Individuals with no ability to produce a particular enzyme may show effects of this deficiency at birth or shortly thereafter. Individuals with only a partial ability to produce a particular enzyme may not show the effects of this deficiency until their need for the enzyme, because
of growth or maturation, has outpaced their ability to produce it.
The level of ability of the pyruvate dehydrogenase complex deficiency affected individual to produce PDH, or his or her ability to sustain existing levels of PDH, are the sole determinants of the severity of the observed symptoms in that individual and the age of onset of these symptoms.
PDHA is the most common cause of non-exercise- related build-up of lactic acid in the tissues (primary lactic acidosis). When a tissue requires more energy than it can gain from aerobic processing (TCA cycle), it begins to break down carbohydrates, via an anaerobic process, in order to gain the necessary energy. Lactic acid is the by-product of carbohydrate metabolism. The build-up of lactic acid in the muscle tissues and red blood cells is normal during strenuous exercise. However, the accumulation of lactic acid in other tissues without exercise or without oxygen deprivation is symptomatic of an underlying problem in the normal aerobic process (TCA cycle).
Genetic profile
The gene responsible for PDHA has been mapped to Xp22.2-p22.1. This gene is now termed the PDHA1 gene. At least 50 different mutations of this gene resulting in varying symptoms of PDHA have been identified. Because the gene for PDHA is on the X chromosome, it is called a sex-linked disease. PDHA shows a dominant inheritance pattern: therefore, females with only one affected X chromosome also exhibit symptoms of the disease.
Demographics
Almost equal numbers of males and females have been identified as being affected with PDHA. Even though PDHA is known to be transmitted as a sex-linked dominant trait on the X chromosome, it is not necessarily lethal in affected males (who possess only a single X chromosome), because the symptoms of PHDA are quite different depending on the precise mutation responsible for the symptoms in each individual. The genetic mutations are linked to the sex of the affected individual. Affected liveborn males tend to have minor (missense/ nonsense type) mutations, while affected females tend to have more major (insertion/deletion type) mutations. The almost unobserved insertion/deletion mutations in males with PDHA suggests that these mutations are fatal to males with only a single X chromosome (homozygous males). Females with two X chromosomes, only one of which contains an insertion/deletion type mutation (heterozygous females) and males with an extra X
deficiency complex dehydrogenase Pyruvate
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
973 |

Pyruvate dehydrogenase complex deficiency
K E Y T E R M S
ATP—Adenosine triphosphate. The chemical used by the cells of the body for energy.
Enzyme—A protein that catalyzes a biochemical reaction or change without changing its own structure or function.
Highly aerobic tissues—Tissue that requires the greatest amount of oxygen to thrive.
Hypotonia—Reduced or diminished muscle tone.
Lactic acid—The major by-product of anaerobic (without oxygen) metabolism.
Mitochondria—Organelles within the cell responsible for energy production.
Pyruvate dehydrogenase complex—A series of enzymes and co-factors that allow pyruvate to be converted into a chemical that can enter the TCA cycle.
TCA cycle—Formerly know as the Kreb’s cycle, this is the process by which glucose and other chemicals are broken down into forms that are directly useable as energy in the cells.
chromosome (XXY males) with this type of mutation on only one chromosome (heterozygous males) are affected with non-lethal forms of PDHA.
A fixed sequence difference between African and non-African samples of the PDHA1 gene has been identified. That is, those of African descent carry a different version of the PDHA1 gene than those of non-African descent. It has been established that these differences in the subpopulations arose more than 200,000 years ago, which predates the earliest known modern human fossils. This genetic evidence is interesting in that it suggests that the modern human emerged from already genetically divided subpopulations.
Signs and symptoms
PDHA affects primarily the brain and central nervous system. In individuals with extreme deficiencies of PDH, the brain may fail to reach normal size during fetal development leading to a small brain and skull (microcephaly). Abnormal development of the cerebrum, cerebellum, and brainstem are the most common brain dysfunctions associated with PDHA. The normal hollow cavities (ventricles) within the brain are usually much larger than normal (dilated) in individuals affected with PDHA. The connection between the left and right hemi-
spheres of the brain (corpus callosum) is generally underdeveloped or completely absent as well.
A condition in which the normal insulating layer (myelin) that surrounds the neurons is either absent or insufficent (leukodystrophy) is observed in many individuals affected with PDHA. Some PDHA affected individuals also have periods of brain malfunctioning in which the neurons within the cerebellum temporarily lose the ability to act in a coordinated fashion (cerebellar ataxia). These attacks of cerebellar ataxia generally last from a few days to a few weeks and reoccur every three to six months thoughout life with decreasing severity after puberty. Lactic acid accumulation in the brain may also lead to breathing (respiratory) and kidney (renal) problems.
Some individuals affected with PDHA experience increased muscle tone in both legs (spastic diplegia) or in all four limbs (spastic tetraplegia) similar to that seen in the classic case of cerebral palsy. Seizures occur in almost all individuals with PDHA. A seizure is the result of sudden abnormal electrical activity in the brain. This electrical activity can result in a wide variety of clinical symptoms including muscle twitches; tongue biting; fixed, staring eyes; a loss of bladder control resulting in involuntary urination; total body shaking (convulsions); and/or loss of consciousness.
Unusual, or dysmorphic, facial features are sometimes associated with PDHA. These include a broad or upturned nose; low-set ears; downward-slanted eyes, drooping eyelids; and a staring or squinting appearance. Other physical symptoms of PDHA include short fingers and arms, urogenital malformations, low muscle tone (hypotonia), and feeding difficulties. Mental impairment is present in some cases. Delayed physical and motor development can also occur.
Diagnosis
Improper brain development in individuals with PDHA is observable in the womb via ultrasound or MRI after birth, although brain malformations may result from any number of other factors. Babies born with PDHA may exhibit low birth weight, a weak suck, failure to thrive, lack of muscle tone, and unusual appearance of the head, face, and limbs. Convulsions, developmental delay, and eye problems may develop a few months after birth. A diagnosis of PDHA is generally confirmed with a blood test for severe lactic acidosis, an observance of deficient PDH activity in sampled or cultured fibroblasts, or by an observance of elevated amounts of lactate and pyruvate in the cerebrospinal fluid drawn in a spinal tap.
974 |
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |

Treatment and management
Treatment of PDHA is on a case-by-case basis depending on the observed symptoms. These treatments may include early and continuing intervention programs for developmental delays and mental retardation, anticonvulsants to control seizures, muscle relaxants to control spasticity, and/or surgery to release the permanent muscle, tendon, and ligament tightening (contracture) at the joints that is characteristic of longer term spasticity.
A high fat diet including beer as an alternative source of the chemical acetyl-CoA that is not produced in high enough supply because of the deficiency of PDH enzyme is often recommended for those individuals affected with PDHA. Dietary supplements of thiamine, liproic acid and L-carnitine have also proven beneficial in some cases.
Prognosis
The prognosis for PDHA affected individuals varies widely with the severity of the symptoms. Until gene or enzyme replacement therapy becomes available, the most seriously affected individuals are not likely to receive relief from their symptoms and many will die at early ages. For those less seriously affected, several treatments are available to improve quality of life. Many less severely affected individuals live normal lifespans with their abilities and quality of life only limited by the degree of mental impairment and muscle spasticity that is present.
Resources
PERIODICALS
Harris, E. and J. Hey “X chromosome evidence for ancient human histories.” Proceedings of the National Academy of
Sciences of the United States of America (March 1999): 3320-4.
Hesterlee, S. “Mitochondrial disease in prespecitve: Symptoms, diagnosis and hope for the future.”Quest (October 1999).
Lissens, W. et al. “Mutations in the X-linked pyruvate dehydrogenase (E1) alpha subunit gene (PDHA1) in patients with a pyruvate dehydrogenase complex deficiency.” Human Mutations (2000): 209-19.
ORGANIZATIONS
Children’s Mitochondrial Disease Network. Mayfield House, 30 Heber Walk, Chester Way, Northwich, CW9 5JB. UK 01606 44733. http://www.emdn-mitonet.co.uk .
United Mitochondrial Disease Foundation. PO Box 1151, Monroeville, PA 15146-1151. (412) 793-8077. Fax: (412) 793-6477. http://www.umdf.org .
WEBSITES
International Mitochondrial Disease Network. http://www
.imdn.org/index.html
Jablonski’s Multiple Congenital Anomaly/Mental Retardation (MCA/MR) Syndromes Database http://www.nlm.nih
.gov/cgi/jablonski/syndrome_cgi?index=548 .
Neuromuscular Center of the Presbyterian Hospital of Dallas.
http://www.texashealth.org/nmc/pyruvate_dehydrogenase
.htm .
OMIM—Online Mendelian Inheritance in Man. http://www
.ncbi.nlm.nih.gov/htbin-post/Omim/dispmim?312170 (February 15, 2001).
Paul A. Johnson
I Pyruvate kinase deficiency
Definition
Pyruvate kinase deficiency (PKD) is part of a group of disorders called hereditary nonspherocytic hemolytic anemias. Hereditary nonspherocytic anemias are rare genetic conditions that affect the red blood cells. PKD is caused by a deficiency in the enzyme, pyruvate kinase. Although PKD is the second most common of the hereditary nonspherocytic anemias, it is still rare, with the incidence estimated to be 51 cases per million in the Caucasian population.
Description
In PKD, there is a functional abnormality with the enzyme pyruvate kinase. Usually, pyruvate kinase acts as a catalyst in the glycolysis pathway, and is considered an essential component in this pathway. Glycolysis is the method by which cells produce their own energy. A problem with any of the key components in glycolysis can alter the amount of energy produced. In the red blood cells, glycolysis is the only method available to produce energy. Without the proper amount of energy, the red blood cells do not function normally. Since pyruvate kinase is one of the key components in glycolysis, when there is a problem with this enzyme in the red blood cells, there is a problem with the production of energy, causing the red blood cells to not function properly.
There are four different forms of the pyruvate kinase enzyme in the human body. These forms, called isozymes, all perform the same function but each isozyme of pyruvate kinase is structurally different and works in different tissues and organs. The four isozymes of pyruvate kinase are labeled M1, M2, L, and R. The isozyme M1 is found in the skeletal muscle and brain, isozyme M2 can be found in most fetal and adult tissues, isozyme L works in the liver, and isozyme R works in the
deficiency kinase Pyruvate
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
975 |
Pyruvate kinase deficiency
K E Y T E R M S
Anemia—A blood condition in which the level of hemoglobin or the number of red blood cells falls below normal values. Common symptoms include paleness, fatigue, and shortness of breath.
Catalyst—A substance that changes the rate of a chemical reaction, but is not physically changed by the process.
Compound heterozygotes—Having two different mutated versions of a gene.
Enzyme—A protein that catalyzes a biochemical reaction or change without changing its own structure or function.
Glycolysis—The pathway in which a cell breaks down glucose into energy.
Hemolytic anemia—Anemia that results from premature destruction and decreased numbers of red blood cells.
Heterozygote—Having two different versions of the same gene.
Homozygote—Having two identical copies of a gene or chromosome.
Isozyme/Isoenzyme—A group of enzymes that perform the same function, but are different from one another in their structure or how they move.
Mutation—A permanent change in the genetic material that may alter a trait or characteristic of an individual, or manifest as disease, and can be transmitted to offspring.
Nonspherocytic—Literally means not sphereshaped. Refers to the shape of red blood cells in nonspherocytic hemolytic anemia.
red blood cells. In PKD, only the pyruvate kinase isozyme found in red blood cells, called PKR, is abnormal. Therefore, PKD only affects the red blood cells and does not directly affect the energy production in the other organs and tissues of the body.
Genetic profile
There are two PK genes and each gene produces two of the four isozymes of pyruvate kinase. The M1 and M2 isozymes are produced by the pyruvate kinase gene called PKM2 and pyruvate kinase isozymes, L and R, are
products of the pyruvate kinase gene, PKLR. The PKLR gene is located on chromosome 1, on the q arm (the top half of the chromosome), in region 21 (written as 1q21). As of 2001, there have been over 125 different mutations described in the PKLR gene that have been detected in individuals with PKD.
PKD is mainly inherited in an autosomal recessive manner. There have been a few families where it appeared that PKD was inherited in either an autosomal dominant manner or where the carriers of PKD exhibited mild problems with their red blood cells. As with all autosomal recessive conditions, affected individuals have a mutation in both pair of genes. Most individuals with PKD are compound heterozygotes, meaning that each PKLR gene in a pair contains a different mutation. There are individuals who have the same mutation on each PKLR gene, but these individuals tend to be children of parents who are related to each other.
There are three mutations in the PKLR gene called, 1529A, 1456T, and 1468T, that are seen more frequently in individuals with PKD than the other mutations. The mutation 1529A is most frequently seen in Caucasians of northern and central European descent and is the most common mutation seen in PKD. The mutation 1456T is more common in individuals of southern European descent and the mutation 1468T is more common in individuals of Asian descent.
For most of the mutations seen in the PKLR gene, no correlation between the specific mutation and the severity of the disorder has been observed. However, for two of the mutations, there has been speculation on their affect on the severity of PKD. When the mutation 1456T has been seen in the homozygous state (when both PKLR genes contain the same mutation), those rare individuals experienced very mild symptoms of PKD. Also, there have been individuals who were homozygous for the 1529A mutation. These individuals had a very severe form of PKD. Therefore, it is thought that the 1456T mutation is associated with a milder form of the disease and the 1529A mutation is associated with a more severe form of the disease. It is not known how these mutations affect the severity of PKD when paired with different mutations.
Demographics
In general, PKD not does appear to affect one gender more than another or be more common in certain regions. However, there are studies of an Amish group in Pennsylvania where a severe form of PKD is more common. As previously mentioned, the three mutations found in the PKLR gene have been linked to individuals of specific decents. Caucasians of northern and central
976 |
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
European decent are more likely to have the 1529A mutations, individuals of southern European descent usually have the 1456T mutation, and individuals of Asian descent are more likely to have the 1468T mutation.
Signs and symptoms
In general, the more severe the PKD, the earlier in life symptoms tend to be detected. Individuals with the more severe form of PKD often show symptoms soon after birth, but most individuals with PKD begin to exhibit symptoms during infancy or childhood. In individuals with the more mild form of PKD, the condition is sometimes not diagnosed until late adulthood, after an acute illness, or during a pregnancy evaluation.
Symptoms of PKD are similar to those symptoms seen in individuals who have long-term hemolytic anemia. The more common symptoms include variable degrees of jaundice (a yellowish pigment of the skin), slightly to moderately enlarged spleen (splenomegaly), and increased incidence of gallstones. Other physical effects of PKD can include smaller head size and the forehead appearing prominent and rounded (called frontal bossing). If a child with PKD has their spleen removed, their growth tends to improve. Even within the same family, individuals can have different symptoms and severity of PKD.
In individuals with PKD, the red blood cells are taken out of their circulation earlier than normal (shorter life span). Because of this, individuals with PKD will have hemolytic anemia. Additionally, the anemia or other symptoms of PKD may worsen during a sudden illness or pregnancy.
Diagnosis
A diagnosis of PKD can be made by measuring the amount of pyruvate kinase in red blood cells. Individuals with PKD tend to have 5–25% of the normal amount of pyruvate kinase. Carriers of PKD also can have less pyruvate kinase in their red blood cells, approximately 40–60% of the normal value. However, there is an overlap between the normal range of pyruvate kinase and the ranges seen with carriers of PKD. Therefore, measuring the amount of pyruvate kinase in the red blood cells is not a good method of detecting carriers of PKD. If the mutations causing PKD in a family are known, it may be pos-
sible to perform mutation analysis to determine carrier status of an individual and to help diagnose individuals with PKD.
Treatment and management
In the severest cases, individuals with PKD will require multiple blood transfusions. In some of those cases, the spleen may be removed (splenectomy). Red blood cells are normally removed from circulation by the spleen. By removing an individual’s spleen (usually a child), the red blood cells are allowed to stay in circulation longer than normal; thereby reducing the severity of the anemia. After a splenectomy, or once an individual with PKD is older, the number of transfusions tends to decrease.
Prognosis
The prognosis of PKD is extremely variable. Early intervention and treatment of symptoms frequently improve the individual’s health. Without treatment, individuals may experience severe complications that could become fatal. Individuals with a mild form of PKD may appear to have no symptoms at all.
Resources
PERIODICALS
Beutler, Ernest, and Terri Gelbart. “Estimating the Prevalence of Pyruvate Kinase Deficiency from the Gene Frequency in the General White Population.” Blood 95 (June 2000): 3585–88.
Kugler, W., et. al. “Eight Novel Mutations and Consequences of mRNA and Protein Level in Pyruvate Kinase Deficient Patients with Nonspherocytic Hemolytic Anemia.” Human Mutation 15 (2000): 261–72.
ORGANIZATIONS
National Heart, Lung, and Blood Institute. PO Box 30105, Bethesda, MD 20824-0105. (301) 592-8573. nhlbiinfo @rover.nhlbi.nih.gov. http://www.nhlbi.nih.gov .
WEBSITES
“Entry 266200: Pyruvate Kinase Deficiency of Erythrocyte.”
OMIM—Online Mendelian Inheritance in Man.
h t t p : / / w w w. n c b i . n i h . g o v / h t b i n - p o s t / O m i m / dispmim?266200 . (March 24, 1999).
Sharon A. Aufox, MS, CGC
deficiency kinase Pyruvate
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
977 |
R
Rapp-Hodgkin syndrome see Ectodermal dysplasia
I Raynaud disease
Definition
Raynaud disease refers to a disorder in which the fingers or toes (digits) suddenly experience decreased blood circulation. It is characterized by repeated episodes of color changes of the skin of digits during cold exposure or emotional stress.
Description
Raynaud disease can be classified as one of two types: primary (or idiopathic) and secondary (also called Raynaud’s phenomenon). Primary Raynaud disease has no predisposing factor, is more mild, and causes fewer complications. About half of all cases of Raynaud disease are of this type. Women are five times more likely than men to develop primary Raynaud disease. The average age of diagnosis is between 20 and 40 years. Approximately three out of ten people with primary Raynaud disease eventually progress to secondary Raynaud disease after diagnosis. About 15% of individuals improve.
Secondary Raynaud disease is the same as primary Raynaud disease, but occurs in individuals with a predisposing factor, usually a form of collagen vascular disease. What is typically identified as primary Raynaud may be later identified as secondary once a predisposing disease is diagnosed. This occurs in approximately 30% of patients. As a result of the predisposing disease, the secondary type is often more complicated and severe, and is more likely to worsen.
Several related conditions that predispose persons to secondary Raynaud disease include scleroderma, lupus
erythematosus, rheumatoid arthritis, and polymyositis. Pulmonary hypertension and some nervous system disorders such as herniated discs and tumors within the spinal column, strokes, and polio can progress to Raynaud disease. Finally, injuries due to mechanical trauma caused by vibration (such as that associated with chain saws and jackhammers), repetitive motion (carpal tunnel syndrome), electrical shock, and exposure to extreme cold can led to the development of Raynaud disease. Some drugs used to control high blood pressure or migraine headaches have been known to cause Raynaud disease.
Genetic profile
There is significant familial aggregation of primary Raynaud disease. However, as of 2001, no causative gene has been identified.
Risk factors for Raynaud disease differ between males and females. Age and smoking seem to be associated with Raynaud disease only in men, while the associations of marital status and alcohol use with Raynaud disease are usually only observed in women. These findings suggest that different mechanisms influence the expression of Raynaud disease in men and women.
Demographics
The prevalence of Reynaud phenomena in the general population varies from 4–15%. Females are seven times more likely to develop Raynaud diseases than are men. The problem has not been correlated with coffee consumption, dietary habits, occupational history (excepting exposure to vibration), or exposure to most drugs. An association between Raynaud disease and migraine headaches has been reported. Secondary Raynaud disease is common among individuals with systemic lupus erythematosus in tropical countries.
Signs and symptoms
Both primary and secondary Raynaud disease signs and symptoms are thought to be due to arterioles
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
979 |

Raynaud disease
K E Y T E R M S
Arteriole—The smallest type of artery.
Artery—A blood vessel that carries blood away from the heart to peripheral tissues.
Gangrene—Death of a tissue, usually caused by insufficient blood supply and followed by bacterial infection of the tissue.
Idiopathic—Of unknown origin.
Lupus erythematosus—A chronic inflammatory disease that affects many tissues and parts of the body including the skin.
Polymyositis—An inflammation of many muscles.
Pulmonary hypertension—A severe form of high blood pressure caused by diseased arteries in the lung.
Rheumatoid arthritis—Chronic, autoimmune disease marked by inflammation of the membranes surrounding joints.
Scleroderma—A relatively rare autoimmune disease affecting blood vessels and connective tissue that makes skin appear thickened.
over-reacting to stimuli. Cold normally causes the tiny muscles in the walls of arteries to contract, thus reducing the amount of blood that can flow through them. In people with Raynaud disease, the extent of constriction is extreme, thus severely restricting blood flow. Attacks or their effects may be brought on or worsened by anxiety or emotional distress.
There are three distinct phases to an episode of Raynaud disease. When first exposed to cold, small arteries respond with intense contractions (vasoconstriction). The affected fingers or toes (in rare instances, the tip of the nose or tongue) become pale and white because they are deprived of blood and, thus, oxygen. In response, capillaries and veins expand (dilate). Because these vessels are carrying deoxygenated blood, the affected area then becomes blue in color. The area often feels cold and tingly or numb. After the area begins to warm up, the arteries dilate. Blood flow is significantly increased. This changes the color of the area to a bright red. During this phase, persons often describe the affected area as feeling warm and throbbing painfully.
Raynaud disease may initially affect only the tips of fingers or toes. As the disease progresses, it may eventually involve all of one or two digits. Ultimately, all the fingers or toes may be affected. About one person
in ten will experience a complication called sclerodactyly. In sclerodactyly, the skin over the involved digits becomes tight, white, thick, smooth, and shiny. In approximately 1% of cases of Raynaud disease, deep sores (ulcers) may develop in the skin. In rare cases of frequent, repetitive bouts of severe ischemia (decreased supply of oxygenated blood to tissues or organs), tissue loss, or gangrene, may result and amputation may be required.
Diagnosis
Primary Raynaud disease is diagnosed following the Allen Brown criteria. There are four components. The certainty of the diagnosis and severity of the disease increase as more criteria are met. The first is that at least two of the three color changes must occur during attacks provoked by cold and/or stress. The second is that episodes must occur periodically for at least two years. The third is that attacks must occur in both the hands and the feet in the absence of vascular occlusive disease. The last is that there is no other identifiable cause for the Raynaud episodes.
A cold stimulation test may also be performed to help to confirm a diagnosis of Raynaud disease. The temperature of affected fingers or toes is taken. The hand or foot is then placed completely into a container of ice water for 20 seconds. After removal from the water, the temperature of the affected digits is immediately recorded. The temperature is taken every five minutes until it returns to the pre-immersion level. Most individuals recover normal temperature within 15 minutes. People with Raynaud disease may require 20 minutes or more to reach their pre-immersion temperature.
Laboratory testing is performed frequently. However, these results are often inconclusive for several rea-
A phenomenon of Raynaud disease occurs when blood flow is temorarily interrupted, causing extremities to become pale due to poor blood circulation. (Custom Medical Stock Photo, Inc.)
980 |
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
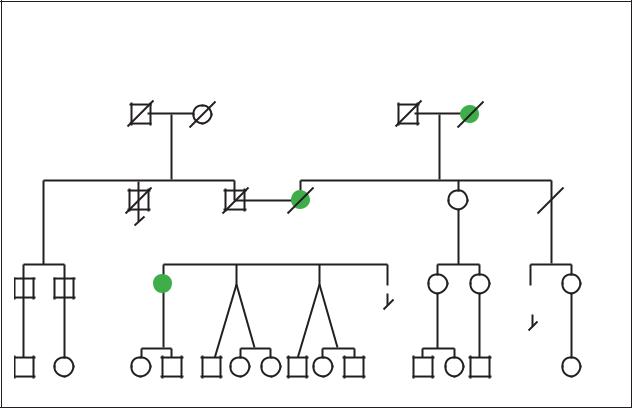
Raynaud Disease
Autosomal Dominant
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
d.61y |
d.76y |
|
|
79y |
d.66y |
||||||
|
|
|
|
|
|
|
Heart attack |
Stroke |
|
|
|
|
Leukemia |
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
52y |
50y |
43y |
41y |
47y |
42y |
2 |
27y 25y 20y 12y 7y 20y 14y 10y
(Gale Group)
sons. Provocative testing such as the ice immersion just described, is difficult to interpret because there is considerable overlap between normal and abnormal results. The antinuclear antibody test of blood is usually negative in Raynaud disease. Capillary beds under fingernails usually appear normal. Erythrocyte sedimentation rates are often abnormal in people with connective tissue diseases. Unfortunately, this finding is not consistent in people with Raynaud disease.
Treatment and management
There is no known way to prevent the development of Raynaud disease. Further, there is no known cure for this condition. Therefore, avoidance of the trigger is the best supportive management available. Most cases of primary Raynaud disease can be controlled with proper medical care and avoidance.
Many people are able to find relief by simply adjusting their lifestyles. Affected individuals need to stay warm and keep their hands and feet well covered in cold weather. Layered clothing, scarves, heavy coats, heavy socks, and mittens over gloves are suggested because gloves alone allow heat to escape. It is also recommended
that patients cover or close the space between their sleeves and mittens. Indoors, they should wear socks and comfortable shoes. Excessive emotional stress should be avoided. Smokers should quit as nicotine worsens the problem. The use of vibrating tools should be avoided as well.
Biofeedback has been used with some success in treating primary Raynaud. This involves teaching people to “think” their fingers and toes to be warm by willing blood to flow through affected arterioles. Biofeedback has had only limited success. Occasionally, medications such as calcium-channel blockers, reserpine, or nitroglycerin may be prescribed to relax artery walls and improve blood flow.
Because episodes of Raynaud disease have also been associated with stress and emotional upset, the condition may be improved by learning to manage stress. Regular exercise is known to decrease stress and lower anxiety. Hypnosis, relaxation techniques, and visualization are also useful methods to help control emotions.
Biofeedback training is a technique during which a patient is given continuous information on the temperature of his or her digits, and then taught to voluntarily
disease Raynaud
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
981 |
