
Полезные материалы за все 6 курсов / Учебники, методички, pdf / INBDEBooster Head and Neck Anatomy Notes
.pdf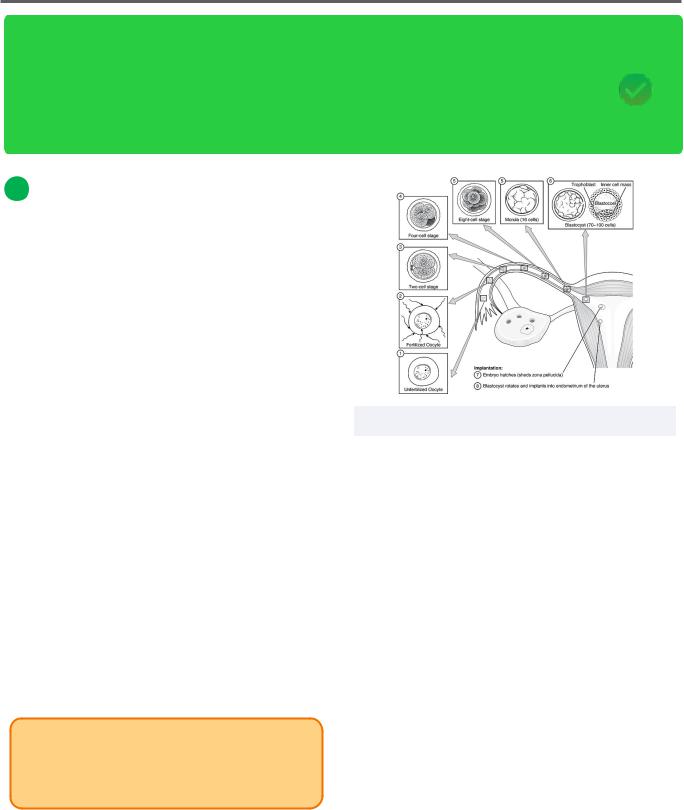
Head and Neck Anatomy |
1 |
Embryology
Head and Neck Anatomy Is one of the most tested topics on the INBDE. This next series reviews high-yield head and neck anatomy topics with key tips and tricks to boost confidence and information retention. Our first chapter is about embryology, this is an important topic on the INBDE that gives candidates an opportunity to share their understanding of human development from fertilization and tissue differentiation to the formation of key organs.
1 The Germinal Stage
Week 1
The process of sperm and an egg fusing together within the Fallopian tube is called fertilization.
•At this point, the two originally haploid cells become a zygote, which is a diploid cell
•After this point, the diploid cell continues to multiply, forming a morula
A morula is a ball of about 8 cells, which has a similar appearance to a mulberry
•The morula then becomes a blastula, a bundle of cells containing an inner cavity known as a blastocoel
•When the blastula begins to fuse with the uterine wall (the endometrium), the process of implantation begins
•After implantation, the blastula will further develop into two predominant structures
The embryoblast is the inner cell mass which will form the majority of the embryo,
The trophoblast is the outer cell mass and will mainly become the placenta
INBDE Pro Tip:
Mnemonic: The embryoblast will form the embryo, while the trophoblast will form the ouTside of the embryo and placenTa.
Figure 1.01 The stages of egg development
Week 2
•At this point, two distinguishing layers of the egg can be seen. Recall that the embryoblast is the inner cell mass. During week two, it forms a bilaminar disc.
•The bilaminar disc contains two parts:
The epiblast will become three major germ layers and will contribute to the further development of the embryo
In contrast, the hypoblast can also be seen, but has little importance as it mostly disappears
•Also visible at this stage includes the amniotic cavity, which will encase the fetus as it develops
•The yolk sac cavity is responsible for nutrient and gas exchange for the fetus before the placenta develops to a point where it can take over this role
INBDE Booster | Booster PrepTM
Head and Neck Anatomy
At the end of week two, the egg is fully Implanted within the endometrium and implantation is complete. The caudal midline can be Identified on the dorsal aspect of the embryo by locating the primitive node and primitive streak.
Figure 1.02 The bilaminar disc and associated regions
2 The embryo
Week 3
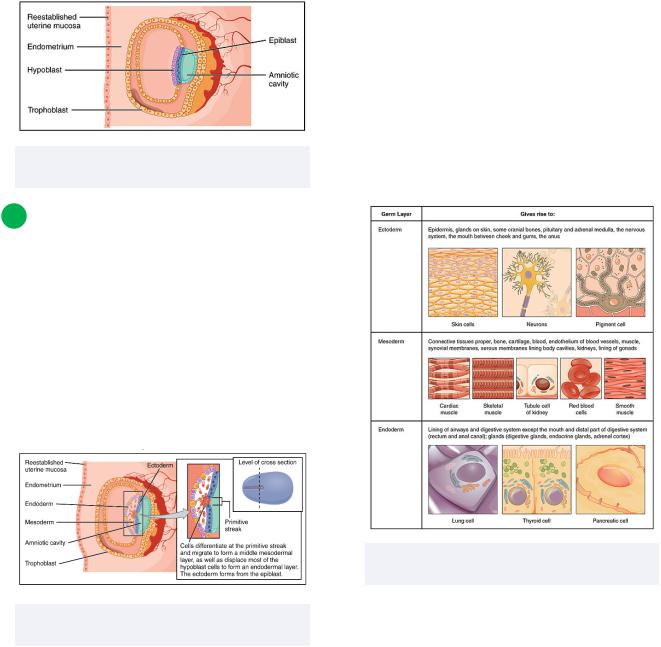
This week is crucial for the development of an embryo. Malformations may occur due to either genetic factors or environmental factors, such as drug consumption. Additionally, gastrulation takes place during the third week, where three distinct germ layers can be seen, the ectoderm, mesoderm and endoderm.
2
The three germ layers are responsible for forming different parts of the body.
•Ectoderm:
Forms epidermis, facial skeleton, nervous system
Forms teeth
-Enamel derived from surface ectoderm
-Majority of tooth derived from neural crest cells
•Mesoderm:
Forms "structural components" of the body like the skeletal system, muscular system, and connective tissue
•Endoderm:
Forms the lining of the foregut, midgut and hindgut
Figure 1.04 The three germ layers and their differentiation options
Figure 1.03 The ectoderm, mesoderm and endoderm layers
INBDE Booster | Booster PrepTM
Head and Neck Anatomy
Week 4
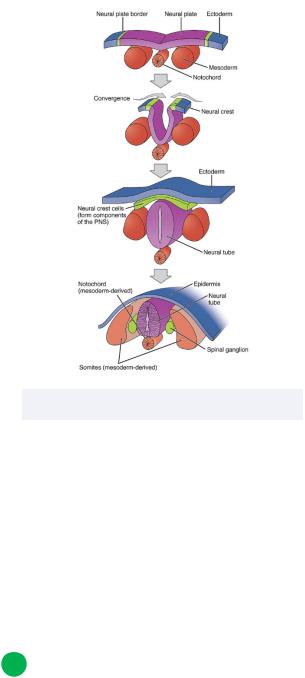
Between weeks three and four, the ectoderm "pinches" down on the endoderm layer, forcing the endoderm layer to form more of an outpouching structure.
Neurulation begins, where the neural plate folds in on itself and forms the neural tube.
•The notochord is derived from mesoderm and is responsible for signalling the start of this process
o Also forms vertebral column
•The neural plate is ectodermal tissue that soon folds into the neural groove
•The neural fold is the joining of the neural plates on either side of the neural plate
•The neural groove is the inner pouch that forms as the neural plate pinches in
•The neural tube is the result of neurulation
o A tube-like structure that sits below the remaining ectodermal layer (soon to be epidermis)
•The neural crest is the former ends of the neural fold
o Neural crest cells migrate throughout the embryo and form various specialized structures
▪Ex. glia, melanocytes
3
Figure 1.05 The process of neurulation
As neurulation ends, aortic arches, pharyngeal arches, and somites begin to form cranially to caudally. Various features can now be seen:
•The buccopharyngeal membrane opens cranially
Forms stomodeum: primitive oral cavity
•Blastopore: primitive anus
Located caudally
•Otic placode: primitive ear
•Optic placode: primitive eye
2 The aortic arch and major branches
Week 4
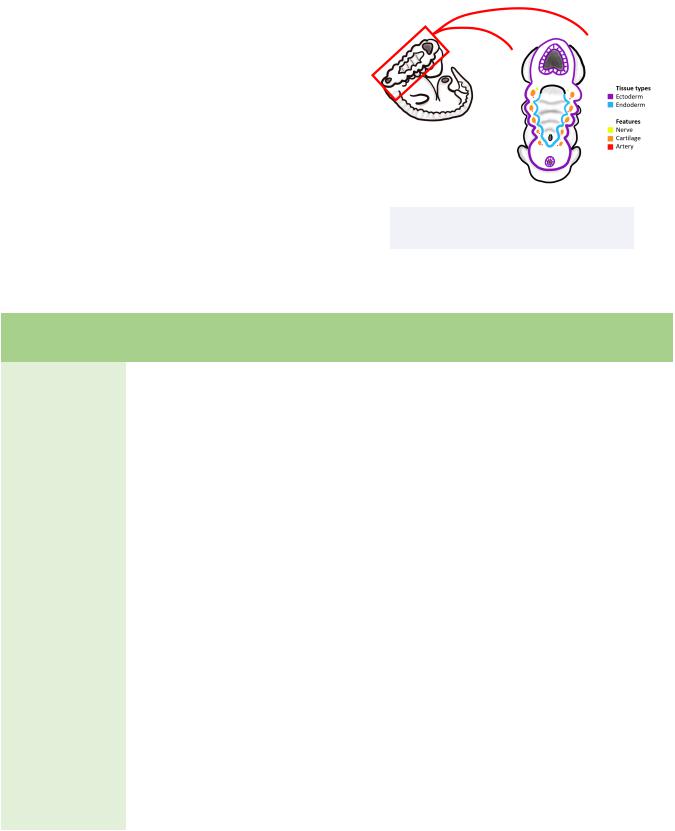
The pharyngeal arches are visible outpouchings that are the precursors to various head and neck structures.
INBDE Booster | Booster PrepTM
Head and Neck Anatomy
•There are six arches in total, but the fifth arch does not derive any structures
•The sixth arch is located deep within the embryo and is not visible
•Have distinct anatomical features:
Endodermal pouch
Mesenchymal core
-Mesoderm
-Neural crest
-Artery
-Nerve
-Muscle
-Cartilage
External ectodermal cleft
4
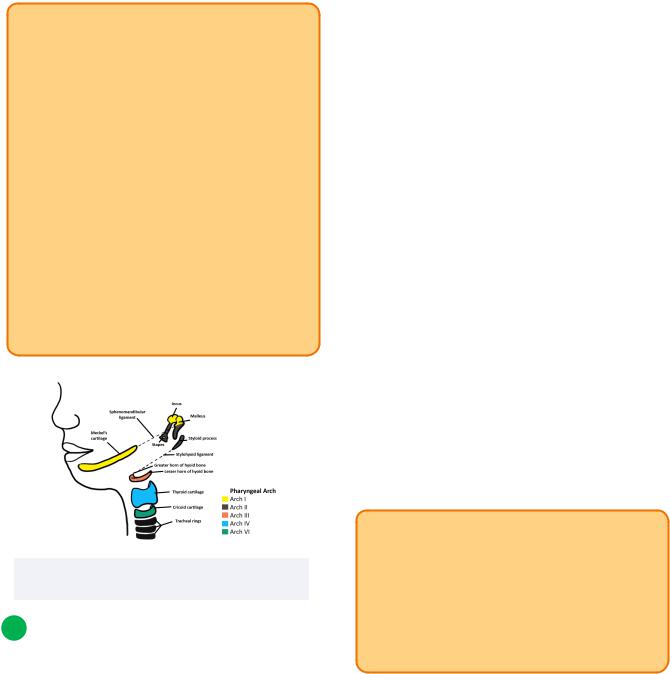
Figure 1.06 The pharyngeal arches and tissue types
Pharyngeal Arch |
Innervation |
Muscular derivatives |
Skeletal and Ligament |
|
|
|
derivatives |
|
|
|
|
I |
V3 |
Muscles of mastication |
Meckel's cartilage |
(Mandibular) |
|
Tensor veli palatini |
Maxilla |
|
|
Tensor tympani |
Mandible |
|
|
Mylohyoid |
Temporal |
|
|
Anterior belly of digastric |
Zygomatic |
|
|
|
Incus |
|
|
|
Malleus |
|
|
|
Sphenomandibular ligament |
|
|
|
|
II |
VII |
Muscles of facial expression |
Reichert's cartilage |
(Hyoid) |
|
Stapedius |
Styloid process |
|
|
Stylohyoid |
Superior half of hyoid body and |
|
|
Posterior belly of digastric |
lesser horns |
|
|
|
Stapes |
|
|
|
Stylohyoid ligament |
|
|
|
|
III |
IX |
Stylopharyngeus |
Inferior half of hyoid body and |
|
|
|
greater horns |
|
|
|
|
IV |
X |
Levator veli palatini |
Thyroid cartilage |
|
|
Pharyngeal constrictors |
|
|
|
Palatoglossus |
|
|
|
Cricothyroid |
|
|
|
|
|
VI (Deep) |
X |
Laryngeal muscles |
Cricoid cartilage |
|
|
|
|
INBDE Booster | Booster PrepTM
Head and Neck Anatomy
INBDE Pro Tip:
There are various ways to remember general information for each pharyngeal arch:
•1st arch:
Many structures are associated with the mandible and anterior ear
•2nd arch:
Many structures associated with posterior ear and regions on an axis moving anteroinferiorly
-Ex. styloid process to anterior hyoid
•3rd arch:
- Inferior hyoid region, few structures
•4th arch:
The "Adam’s apple" cartilage
CN X muscles of deep pharyngeal region
•6th arch:
Most inferior cartilage before trachea
Figure 1.07 The pharyngeal arches, and their eventual derivatives
3 Other Features of Pharyngeal Arches
Week 4
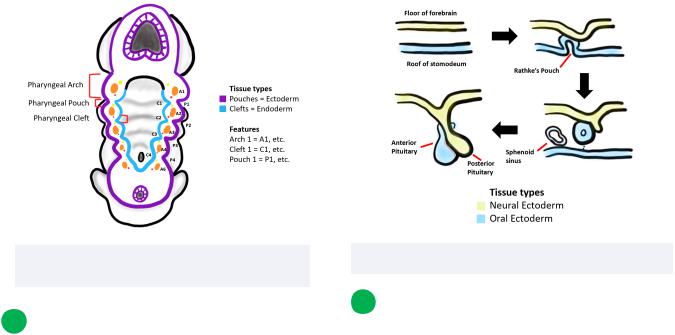
Pharyngeal arches have other distinct regions that are associated with them. Pharyngeal clefts are grooves on the ectodermal side between adjacent pharyngeal arches. Any issues in cleft formation results in a brachial cyst. In contrast, pharyngeal pouches are grooves found on the endodermal side between pharyngeal arches. If pharyngeal pouches fail to develop correctly, brachial fistulas may result.
5
•Arch 1:
Placode: Trigeminal ganglion (CN V)
Cleft: External auditory meatus
Pouch: Eustachian tube and tympanic cavity
•Arch 2:
Placode: Geniculate ganglion (CN VII)
Cleft: Cervical sinus
Pouch: Palatine tonsil
•Arch 3:
Placode: Inferior sensory ganglion (CN IX)
Cleft: Cervical sinus
Pouch: Thymus and inferior parathyroids
*Note: pouch derivatives eventually migrate inferiorly by the lungs
•Arch 4:
Placode: Inferior sensory ganglion (CN X)
Cleft: Cervical sinus
Pouch: Superior parathyroids and ultimobranchial body (parafollicular cells)
*Note: pouch derivatives eventually migrate inferiorly by the lungs, but remain superior to arch 3 pouch
INBDE Pro Tip:
There are only four pharyngeal pouches, placodes, and clefts. This is because they are located directly below each pharyngeal arch. Since there are really only 5 functional arches and the last of these is not visible (and thus does not have any features below it), this makes sense.
INBDE Booster | Booster PrepTM
Head and Neck Anatomy
Figure 1.08 The pharyngeal arches, clefts, and pouches
5 The Pituitary Gland
Week 4
The development of the pituitary gland has a series of steps.
•Roof of oral cavity (stomodeum) forms an evagination superiorly, known as Rathke's pouch
Forms the anterior pituitary gland
Oral ectodermal origin
•Floor of forebrain (diencephalon) evaginates inferiorly
Forms posterior pituitary gland
Neural ectodermal origin
Recall that physiologically, the anterior pituitary gland (adenohypophysis) and posterior pituitary gland (neurohypophysis) secrete hormones to organs indirectly and directly, respectively. Embryologically we can now appreciate why the endocrine system is wired this way!
6
Figure 1.09 The formation of the pituitary gland
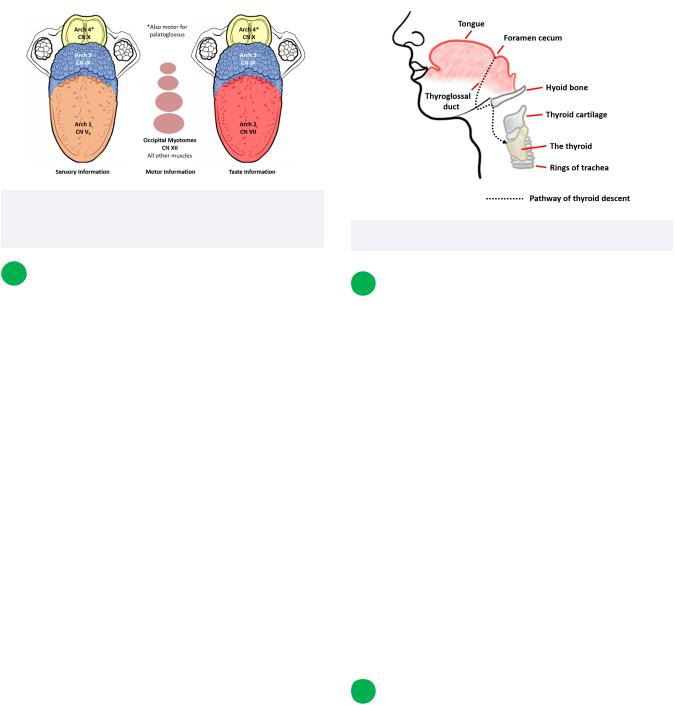
6 The Tongue
Week 4
The tongue is said to be segmented based on its development from four different pharyngeal arches plus contributions from the occipital myotomes. Various arches and nerves contribute to different segments.
•Arch 1:
Innervation: CN V
Modality: Sensory
Region of tongue: Anterior 2/3
•Arch 2:
Innervation: CN VII
Modality: Taste
Region of tongue: Anterior 2/3
•Arch 3:
Innervation: CN IX
Modality: Sensory and taste
Region of tongue: Posterior 1/3
•Arch 4:
Innervation: CN X
Modality: Taste, both sensory and motor (palatoglossus muscle)
Region of tongue: Base
•Occipital myotomes (from somites):
Innervation: Motor (remaining muscles of tongue)
INBDE Booster | Booster PrepTM
Head and Neck Anatomy |
7 |
Figure 1.10 The development of the tongue, segmented into anterior 2/3, posterior 1/3, and base
7 The Thyroid Gland
Week 4
The thyroid gland is derived from tissues located at the tongue's base. Specifically, it develops from a depression known as the foramen cecum.
The thyroid gland descends caudally and ventrally to the pharynx. This is made possible via the presence of the thyroglossal duct. This duct allows for the temporary connection of the foramen cecum of the tongue and the thyroid gland.
Clinically, a lingual thyroid may be present at the base of a patient's tongue if the thyroid did not descend properly during embryological development.
Figure 1.11 The descent of the thyroid gland
8 The ear
The first and second pharyngeal arches are responsible for the formation of the ear. These two arches form six auricular hillocks per side of the embryo.
•Each pharyngeal arch contributes three auricular hillocks
The opening of the ear canal (external auditory meatus) will be located between these two groups of hillocks
•Each hillock contributes to a different region of the ear
•Clinically, if a pregnant mother takes drugs containing retinoic acid (like Accutane for acne), defects in first and second arches may occur
Microtia: small ears
Micrognathia: small mandible
9 The aortic arch and major branches
Between weeks 4 to 8
The lips are developed when numerous structures of the embryological face come together.
•Surrounding the nasal pits is the lateral nasal prominence and medial nasal prominence
INBDE Booster | Booster PrepTM
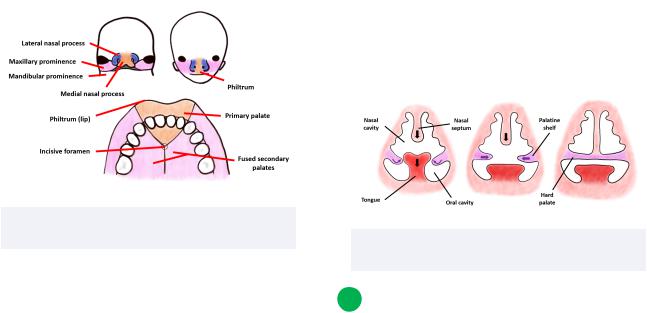
Head and Neck Anatomy
•Laterally and inferiorly, the maxillary prominence can be found
•Process:
Maxillary prominences move ventrally and medially
-Forms cheeks and lateral aspects of the upper lip
-Medial nasal prominences forced medially and fuse togetherForm crest and tip of nose and
philtrum
The mandibular prominence contributes to the jaw and lower lip
•Clinically, failure of the medial nasal prominence and maxillary prominence to fuse results in a cleft lip
May occur unilaterally, bilaterally, or at the midline
Figure 1.12 Components of lip and palate development
The palate begins to develop at the sixth week, following formation of the lips.
•The primary palate is comprised of the philtrum of the lip anteriorly and forms via fusion of the two medial nasal prominences at midline
Triangular in shape when viewed inferiorly
This is where the 4 maxillary incisors will grow after birth
•The palatine shelves on either side of the embryo will also develop during week six
Move caudally and medially on both sides
8
•During week seven, the tongue moves inferiorly into the expanding oral cavity through the palatine shelves
•The palatine shelves can now move horizontally and medially to fuse at the midline
Fusion occurs in a cranial-to-caudal fashion
•The collective fusion of the palatine shelves is called the secondary palate
•The fusion of the primary and secondary palates at the midline is called the incisive foramen
•Clinically, patients with cleft palate may have missing or malformed lateral incisors
Incomplete cleft palate: failure of palatal shelves to fuse
Complete cleft palate: failure of primary palate to fuse with palatal shelves
After week 8, the embryo is now considered a fetus.
Figure 1.13 Direction of palate formation and tongue migration (coronal view)
10 DiGeorge Syndrome
Clinical relevance
DiGeorge Syndrome is a developmental disorder caused by either genetic or environmental factors. Also called third and fourth pouch syndrome.
INBDE Booster | Booster PrepTM

Head and Neck Anatomy |
9 |
•Affects neural crest cells
•Affects third and fourth pharyngeal pouches
Thymus and parathyroid gland development severely impacted
INBDE Pro Tip:
An important mnemonic to remember is CATCH 22.
Cardiac abnormalities
Abnormal facies (hypertelorism, short philtrum, small mandible)
Thymic aplasia Cleft palate
Hypocalcemia (from lack of PTH via parathyroid)
22q11 deletion (on chromosomes)
INBDE Booster | Booster PrepTM
Head and Neck Anatomy |
10 |
Bones of the Skull
The bones of the skull are a good foundation to have for your board exam. Candidates must understand the gross anatomy of skull, categorization of its regions, its features, specific bones, and characteristics of major bony structures. These notes include high-yield information relating to everything you need to know regarding the bones of the skull for the INBDE, plus some useful mnemonics as an aid during studying.
1 Overview of the Skull
The skull is a major protective structure comprised of bone that primarily functions as a cavity for the brain and other supportive neurological components. Another major function is to support the face. There are two main components:
•The neurocranium – includes the calvaria or skullcap and encases the brain
This posterior region of the skull is formed by the paraxial mesoderm
•The viscerocranium – contains aspects of the skull not included in the calvaria, like the bones of the face
This anterior portion of the skull is formed by the neural crest cells
The skull is not a singular bone. It is made up of numerous bones through the presents of fibrous joints called sutures. Their purpose is to allow brain growth during childhood and even adolescence, until they finally fuse in adulthood.
The neurocranium
This region is formed by 8 bones in total. It has two major subdivisions, known as the roof and the base.
•The roof: functions to protect the brain superiorly and posteriorly
Include the frontal, parietal, and occipital bones
•The base: protects the brain inferiorly
Includes the frontal, ethmoid, sphenoid, temporal, parietal, and occipital bones
The viscerocranium
Contains many more bones than the neurocranium (14 total). Although this region does not protect the brain, it functions to:
•Support the soft tissues of the face
•House and protect numerous key functional areas of the skull
The sinuses, nasal and oral cavities, and even the orbits
•Include the maxilla, zygomatic, lacrimal, nasal, palatine, ethmoid (superior and middle nasal conchae), inferior nasal conchae, mandible, and vomer
Figure 2.01 Two major regions of the Skull |
INBDE Booster | Booster PrepTM |
