
Полезные материалы за все 6 курсов / Учебники, методички, pdf / INBDEBooster Head and Neck Anatomy Notes
.pdf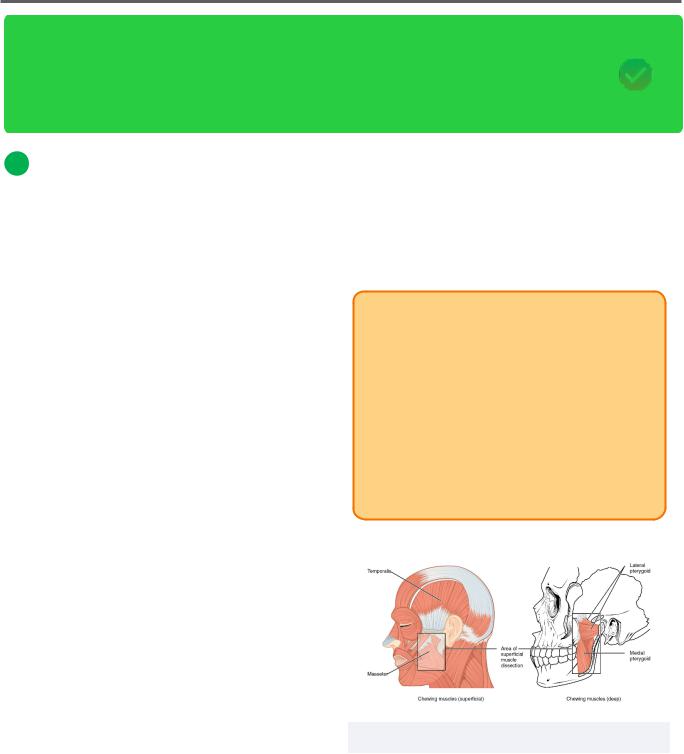
Head and Neck Anatomy |
41 |
Muscles of Mastication
The muscles of mastication are very important to know for the INBDE. Candidates are required to understand the four main muscles involved in mastication, their characteristics, innervation, functions, and actions. These notes will provide high-yield information for the muscles of mastication section of the INBDE, plus some helpful tips and tricks that will serve as a useful guide for studying.
1 Muscles of Mastication Overview
The muscles of mastication are a group of 4 muscles which assist in the process of mastication. Mastication is the act of chewing, where opening and closing of the jaw and associated muscles crush food. This allows saliva to help further break down food and begins the process of digestion.
Embryologically, this group of muscles is derived from the paraxial mesoderm of the first pharyngeal arch. Every muscle of mastication is innervated by the mandibular branch of the trigeminal nerve (CN V3).
Anatomical Terms
•Origin – immobile part of muscle; pulls the insertion region towards it
•Insertion – mobile part of muscle; is pulled towards origin region
•Unilateral – if there are two muscles (one on each side of the body), engagement of muscle on ONE side
•Bilateral – if there are two muscles (one on each side of the body), engagement of muscles on BOTH sides
•Contralateral – action occurring on the OPPOSITE side of the body
•Ipsilateral – action occurring on the SAME side of the body
•Protraction/protrusion – moving a part forward
•Retraction – moving a part backward
•Elevation – moving a part superiorly
•Excursion – side-to-side movement; may be lateral or medial movement
INBDE Pro Tip:
To understand excursion of the mandible, an understanding of contralateral or ipsilateral must also be applied.
•Contralateral excursion: the mandible is moving medially
•Ipsilateral excursion: the mandible is moving laterally
Ex. If the left masseter muscle is engaged (ie. unilaterally), ipsilateral excursion will result. This
means the jaw will move to the left.
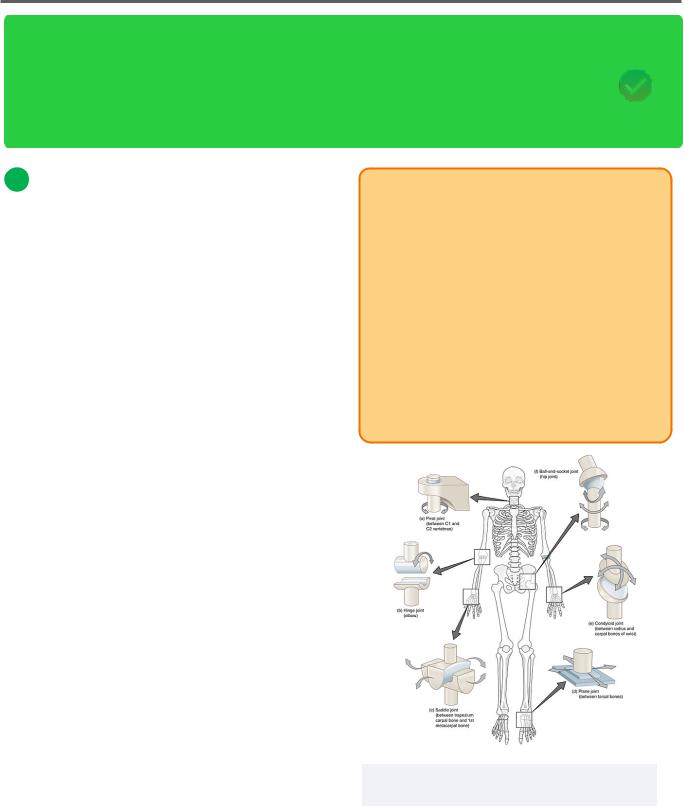
Figure 7.01 The four muscles of mastication
INBDE Booster | Booster PrepTM
Head and Neck Anatomy
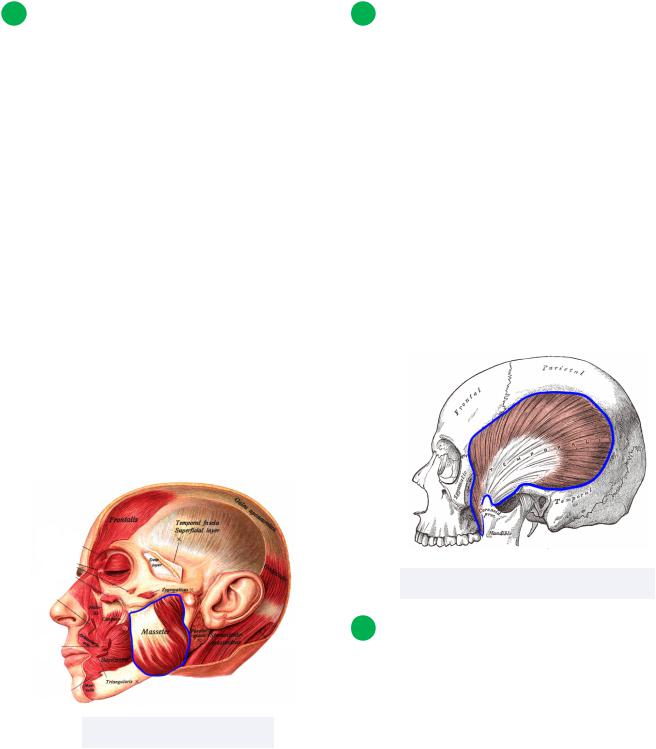
2 The Masseter
Muscle description
The masseter has a superficial part and deep part. The superficial fibers run obliquely (posteroinferiorly). The deep fibers are vertically oriented, running inferiorly.
•Innervation:
Masseteric branch of CN V3
•Superficial part:
Origin: anterior 2/3rds of zygomatic arch
Insertion: lateral part of ramus and angle of mandible
Action: protrudes mandible
•Deep part:
Origin: posterior 1/3rd of zygomatic arch
Insertion: lateral part of ramus and angle of mandible
Action: retracts mandible
•Both:
Action: elevates mandible, unilateral contraction leads to ipsilateral excursion
42
3 The Temporalis
Muscle description
The temporalis is a large muscle whose anterior fibers run vertically (superiorly), and posterior fibers run obliquely (anteroinferiorly). This muscle is deep to the masseter and zygomatic process.
•Innervation:
Deep temporal nerve branches of CN V3
•Origin: temporal line of temporal fossa
•Insertion: coronoid process of mandible
•Anterior fibers:
Action: elevation of mandible
•Posterior fibers:
Action: retraction of mandible
Figure 7.03 The temporalis muscle
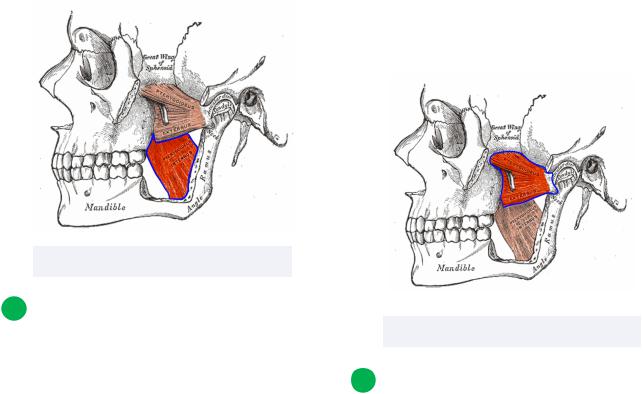
4 The Medial Pterygoid
Figure 7.02 The masseter
Muscle description
The medial pterygoid is a smaller muscle, whose fibers descend posterolaterally. This muscle is found within the infratemporal fossa. It is deep to the masseter, zygomatic process, and temporalis.
INBDE Booster | Booster PrepTM
Head and Neck Anatomy |
43 |
• Innervation: |
• Innervation: |
Pterygoid nerve branches of CN V3 |
Pterygoid nerve branches of CN V3 |
• Superficial part: |
• Superior head: |
Origin: tuberosity of the maxilla and |
Origin: superior border of infratemporal |
pyramidal process of palatine bone |
fossa at the infratemporal crest (sphenoid |
• Deep part: |
bone) |
Origin: medial region of lateral pterygoid |
Insertion: articular disc and joint capsule |
plate |
of the temporomandibular joint |
• Both: |
• Inferior head: |
Insertion: medial region of ramus and |
Origin: lateral region of lateral pterygoid |
angle of mandible |
plate (sphenoid bone) |
Action: elevation and protrusion of |
Insertion: pterygoid fovea of the |
mandible; unilateral contraction leads to |
condylar neck (mandible) |
contralateral excursion |
• Both: |
|
Action: depression and protrusion of |
|
mandible; unilateral contraction leads to |
|
contralateral excursion |
Figure 7.04 The medial pterygoid
5 The Lateral Pterygoid
Muscle description
The lateral pterygoid is another small muscle whose muscle fibers run horizontally (laterally). Its unilateral action is the same as the medial pterygoid muscle.
Figure 7.05 The lateral pterygoid
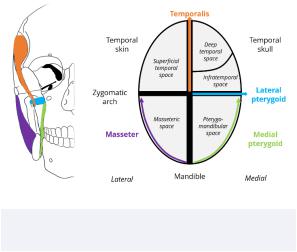
6 Understanding Anatomical Planes
Putting it all together
Placing the muscles of mastication into a diagram may help with understanding their location relative to one another, in addition to their actions (elevation/depression and direction of excursion).
INBDE Booster | Booster PrepTM
Head and Neck Anatomy |
44 |
Main takeaways:
•The masseter's action mirrors that of the pterygoid muscles
•The pterygoid muscles are responsible for moving the mandible medially
•The masseter moves the mandible laterally
•The masseter, temporalis, and medial pterygoid all elevate the mandible
•The medial pterygoid and masseter muscles are both mixed in terms of their movements: horizontal and vertical
Figure 7.06 Planes of motion within the masticator space
Note: Although the above diagram can be helpful in visualizing the actions of each muscle of mastication, it is not exhaustive. The x and y axis movements are displayed, but does not include the z axis (which would include actions such as protraction and retraction).
Watch INBDE Booster's Muscles of Mastication Video from 14:33 to 16:17 for a more in-depth explanation of the diagram above.
INBDE Booster | Booster PrepTM
Head and Neck Anatomy |
45 |
Temporomandibular Joint
The temporomandibular joint is involved in the masticatory process, speech, and providing structural support to the mandible. For this topic, candidates will need to relate information on the temporomandibular joint to their knowledge of masticatory and surrounding muscles, vasculature, and connective tissue. These notes will provide a good basis on the temporomandibular joint, so you are feeling well-prepared for the INBDE.
1 Overview of the TMJ
Introduction
The temporomandibular joint (TMJ) is a complex joint that connects the mandible to the rest of the skull. The TMJ is classified as a synovial joint (or diarthrosis). Typically, synovial joints are the meeting of bones or cartilage in the presence of a fibrous capsule filled with synovial fluid that supports and protects the movement of articulating bones.
The TMJ is unique because unlike most synovial joints that are composed of hyaline cartilage, it contains fibrocartilage instead. Hyaline cartilage is a softer, more flexible cartilage than fibrocartilage because there are less collagen fibers present.
The TMJ is bilaterally located and must coordinate with the contralateral side in order to function properly. It contains two main aspects, a hinging joint (ginglymus) and a sliding joint (arthrodia). As a result, the TMJ is considered a ginglymoarthrodial joint.
INBDE Pro Tip:
The TMJ is susceptible to damage, injury, or disease just like any other joint. When there is a disorder of the TMJ or muscles of mastication, individuals are said to have a temporomandibular (joint) disorder (TMD).
Since this is a general term that describes many different symptoms (such as headaches, tinnitus, and ear pain), understanding the components of the TMJ will be helpful in diagnosing and understanding a patient's case. Posture, stress, bruxism, and diet can also be important factors to consider.
Figure 8.01 Various types of synovial joints, such as the hinge and plane joints
INBDE Booster | Booster PrepTM
Head and Neck Anatomy
Articular disc
The articular disc is a fibrocartilaginous surface that stabilizes the mandibular condyle and minimizes friction between its articulating surfaces and acts as a shock absorber during movement. It separates the TMJ into a superior compartment and an inferior compartment. It is comprised mainly of Type I collagen and has a biconcave shape.
•The superior compartment is located inferior to the mandibular fossa and superior to the articular disc
Produces translational movement
(uniform movement in the same direction)
•The inferior compartment is found inferior to the articular disc and superior to the mandibular condyle
Produces rotational movement
(movement around a fixed circular or orbital path)
Proprioceptive fibers in the anterior and posterior aspects of the disc send signals to the brain which unconsciously assist in positioning the mandible.
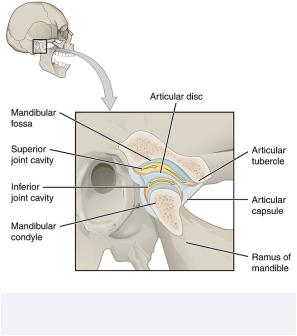
Figure 8.02 The temporomandibular joint and its components
46
Articular cartilage
Articular surfaces of the mandibular fossa and condyle contain fibrocartilage. The rigidity of the articular cartilage is due to the presence of cartilage-like proteoglycans which promote mechanical and compressional resilience.
Retrodiscal tissue
The retrodiscal tissue is found posterior to the TMJ disc and has three main divisions:
•Temporal or superior lamina: connects the superior region of the disc to the temporal bone
Covered in synovial membrane
Contains elastin
•Intermediate: contains nerves and blood vessels
•Condylar or inferior lamina: connects inferior region of the disc to the posterior condylar surface
Covered in synovial membrane
Contains collagen
Synovial membrane
The synovial membrane covers the TMJ capsule. It contains the synovial fluid and is comprised of vascularized connective tissue. The synovial membrane is responsible for creating synovial fluid, which reduces friction and provides nutrition to surrounding tissues (especially those that lack a blood supply). The membrane also plays a role in immune response by housing macrophage-like cells. The synovial fluid contains plasma filtrate, proteins, and mucins
Bones
The TMJ is an articulation between the temporal bone and the mandibular condyle. Specifically, the mandibular or glenoid fossa and articular tubercle or eminence of the temporal bone.
INBDE Booster | Booster PrepTM
Head and Neck Anatomy
There are some variations in condylar size and shape across individuals, although condyles should demonstrate bilateral symmetry. Condyles may be convex, flat, angled, or round. Asymmetrical condylar shapes or drastic changes to condylar shapes may cause temporomandibular disorders (TMDs) or signify other health concerns such as arthritis.
Figure 8.03 The relation of the TMJ to the temporal bone and mandible
2 Ligaments
Overview
Recall that ligaments joint bones and/or cartilages together. There are two major classifications of ligaments associated with the TMJ, the intrinsic or functional and the extrinsic or accessory.
The intrinsic ligaments include the capsular, lateral and collateral. The extrinsic ligaments include the stylomandibular and sphenomandibular.
47
Capsular ligament
The capsular ligament is a fibrous connective tissue that encapsulates the TMJ and contains the synovial fluid within the joint. Borders the temporal bone near the articular fossa and eminence superiorly and the neck of the condyloid process inferiorly.
Lateral/temporomandibular ligament
The lateral ligament is the outer, thicker layer of the capsule. It is located by the zygomatic arch and runs obliquely and posteriorly to the posterolateral aspect of the condylar neck.
This ligament is responsible for ensuring posterior and lateral displacement of the mandible does not occur. Excess medial displacement is also prevented by the contralateral lateral ligament.
Figure 8.04 The capsular and temporomandibular ligaments
INBDE Booster | Booster PrepTM

Head and Neck Anatomy
Collateral/discal ligament
Connected to the articular disc medially and laterally are the collateral ligaments, which provide further support to the articular disc.
Stylomandibular ligament
As evident from its name, the stylomandibular ligament attaches from the styloid process to the angle of the mandible. It is found posterior to the TMJ and tenses during excessive protrusion of the mandible. This ligament is thought to be a thickening of the deep cervical fascia.
Sphenomandibular ligament
The sphenomandibular ligament spans from the superior angular spine of the sphenoid bone to the lingula of the mandible. It plays a role in mandibular support by reducing the extent to which the jaw can be opened (excessive condylar translation). This ligament is a remnant from the embryological Meckel's cartilage.
Figure 8.05 The capsular and stylomandibular, and sphenomandibular ligaments
48
Additional ligaments
There are a few other cervical ligaments associated with TMJ region:
•Pterygomandibular ligament (or raphe)
Thickening of buccopharyngeal fascia
Courses from pterygoid hamulus to the posterior aspect of the myohyoid line of the mandible
Contacts the buccinator and pharyngeal constrictor muscle
Ensures jaw movements are not too excessive
•Stylohyoid ligament
Attachment of the styloid process to the lesser horn of the hyoid bone
Contains a small amount of cartilage in the center; Eagle Syndrome occurs when this becomes ossified, or may also occur due to an elongated styloid process
-Pain is experienced in the oropharynx and facial regions
3 Neuromuscular supply
Overview
The TMJ is supplied as follows:
•Blood supply:
Superficial temporal, maxillary, and masseteric arteries
•Drainage:
Pterygoid plexus
•Innervation:
The anterolateral articular aspect of the capsule is supplied by CN V2, the masseteric branch
The lateral aspect of the capsule is supplied by CN V3, the auriculotemporal branch
INBDE Booster | Booster PrepTM
Head and Neck Anatomy |
49 |
Muscles of Facial Expression
The muscles of facial expression are good to know for the INBDE because they can be used clinically to explain nerve damage or other neurological conditions. Candidates will gain a strong understanding of these muscle groups, their location, orientation, and action. More attention should be given to the application of these muscles and their function to best prepare for the board exam. These notes will simplify everything you need to know for this section so that you're ready to answer any question related to these muscles.
1Muscles of Facial Expression Overview
The muscles of facial expression are a group of muscles involved in various facial movements or expressions. They can be grouped into 5 different sections based on their general location and function. These muscles originate from the bone or fascia and are fairly unique because they insert directly onto the skin.
Embryologically, this group of muscles is derived from the same origin, the 2nd pharyngeal arch. As such, all of the muscles are innervated by the facial nerve (CN VII).
It's best not to try and memorize each muscle function individually. Try to group muscles together based on whatever works for you: shape, function, action, or general location. It's unlikely that the origin and insertion of a muscle would be more important than its function and clinical relevance on the INBDE. The origin and insertion can be useful to help you understand how the muscle will contract when it's activated.
INBDE Pro Tip:
The names of the facial muscles will often give away their function. Usually, the name of a muscle will have something to do with its associated region, relative location to another structure, function, or point of origin. Here's a quick overview of some Latin words and their meanings:
•Levator: to lift or raise
•Labii: lip
•Anguli: an angle or corner
•Depressor: to depress or push down
•Corrugator: to wrinkle
•Supercilii: the eyebrows
•Procerus: tall or extended
•Risorius: laughing/ridiculous
•Mentalis: chin
•Buccinator: trumpeter
•Oris: the mouth
•Oculi: the eyes
Don’t mix up oris and oculi! The oris deals with the mouth, which can be used to give a kiss (orkiss), while the oculi deal with the "ocul-eye."
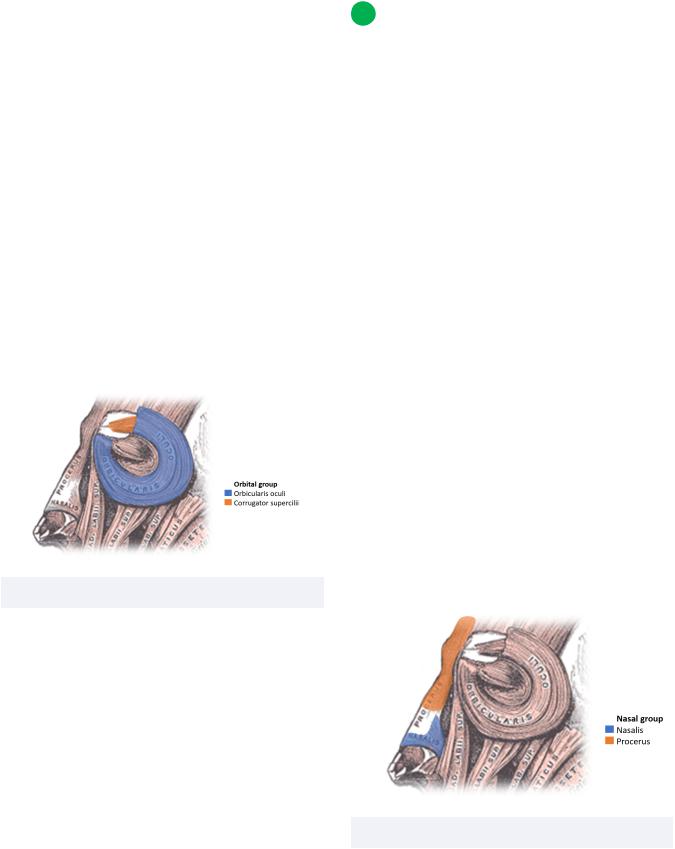
2 The Orbital Group
Orbicularis oculi
This muscle surrounds the orbit of the eye and contains three parts: orbital, palpebral and lacrimal.
INBDE Booster | Booster PrepTM
Head and Neck Anatomy
•Origin:
Orbital: medial palpebral ligament and frontal process of maxilla
Palpebral: medial palpebral ligament
Lacrimal: between medial palpebral ligament and lacrimal sac
•Insertion:
Orbital: soft tissue of surrounding region
Palpebral: lateral palpebral ligament
Lacrimal: superior and inferior tarsal plates and the lateral palpebral ligament
•Action:
Orbital: tightly closes eyelids
Palpebral: gently closes eyelids (fine control)
Lacrimal: dilates lacrimal sac and compresses the lacrimal gland and ducts to facilitate tear drainage
Figure 9.01 The orbital muscle group
Corrugator supercilii
This muscle is relevant to the eyebrow region and is relatively thin in shape.
•Origin: frontal bone (superciliary arch)
•Insertion: oriented superolaterally towards skin of eyebrows
•Action: moves the eyebrows medially, resulting in vertically oriented wrinkles on nose bridge
50
3 The nasal Group
Nasalis
This muscle covers the majority of the nose and is bilaterally located through the midline of the face. It contains two parts, the alar and transverse, which cover the nostrils and dorsum of the nose, respectively.
•Origin:
Alar part: frontal part of maxilla
Transverse part: frontal region of maxilla, lateral to alar part
•Insertion:
Alar part: alar skin
Transverse part: dorsum of nose
•Action:
Alar part: dilates the nostrils, may facilitate deep breathing
Transverse part: compresses the nares
Procerus
This upside-down triangular-shaped muscle covers the glabella of the nose (where one might find a uni-brow).
•Origin: nasal bone
•Insertion: skin of lower medial forehead and medial eyebrows
•Action: depresses medial ends of eyebrows and creates transverse wrinkle over glabella
Figure 9.02 The nasal muscle group
INBDE Booster | Booster PrepTM
