
Ghai Essential Pediatrics8th
.pdf
Table 18.10: Etiology of mental retardation
Chromosomal disorders: Trisomies 21, 18, 13; Klinefelter syndrome
Genetic syndromes: Fragile X, Prader-Willi syndrome, tuberous sclerosis
Inborn errors of metabolism: Phenylketonuria, Tay-Sachs disease, mucopolysaccharidoses, galactosemia, organic acidemias
Congenital infections: HIV, toxoplasmosis, rubella, CMV, syphilis, herpes simplex
Perinatal causes: Hypoxic ischemic encephalopathy, intra ventricular hemorrhage, periventricular leukomalacia, fetal alcohol syndrome
Postnatal causes: Trauma, meningitis, hypoglycemia, kernicterus, thrombosis of cerebral vessels
Iodine deficiency
Developmental defects: Microcephaly, craniostenosis, porence phaly, cerebral migration defects
at riskfor cerebral hemorrhage, anoxiaand infections.The small for gestational age infant is subjected to adverse genetic or prenatal environmental influences, which may occasionally result in brain damage.
Advanced maternal age. Chromosomal anomalies such as Down syndrome as well as intrauterine factors, such as fetal deprivation and hypoxia are commoner in offspring of older mothers. Birth trauma is frequent in the infant of the older prirnipara.
Consanguinity of parents is associated with a high incidence of genetically transmitted mental handicap.
Clinical Features
The mental age is below the chronological age. Most of them present with the behavior syndrome of cerebral dysfunction,suchas hyperactivity,shortspanof attention, distractibility, poor concentration, poor memory, impulsiveness, awkward clumsy movements, disturbed sleep, emotional instability, frustration, low tolerance and wide scatter in intellectual function.
Associated defects of the musculoskeletal system, of vision, or speech and hearing are often found in mentally handicapped children. Congenital anomalies of other systems, apart from the neurological system, may be associated. Convulsions are common in the mentally handicapped.
History should include developmental and family history. A complete physical examination will usuallyhelp in the diagnosis. It should include an examination of the fundus and a developmental assessment.
Additional investigations are necessary in some cases, depending on the probable diagnosis. These include urine tests (chromatographyand screening forphenylketonuria, homocystinuria and galactosemia) and chromosomal studies, where indicated. Appropriate tests are required
Central Nervous System -
to diagnose hypothyroidism, storage disorders and intrauterine infections. Computerized tomography and MRI helps define hydrocephalus, porencephaly, absence ofcorpuscallum, tuberoussclerosisandmigrationdefects.
Prevention
Genetic counseling. The risk of disorders with autosomal recessiveinheritance is high in consanguineous marriages. Parents should be counseled about the risk of recurrence in inherited neurometabolic disorders. Mothers older than 35 yr should be screened for Down syndrome during pregnancy.
Vaccination of girls with rubella vaccine should be encouraged to prevent fetal rubella syndrome. During pregnancy, good antenatal care and avoidance of teratogens should be emphasized. Mothers should be protected from contact with patients suffering from viral diseases. When indicated, amniocentesis may be done for study of amniotic fluid for tissue culture, chromosome studies, alpha-fetoprotein and enzyme for prenatal diagnosis. During labor, good obstetric and postnatal supervision is essential to prevent occurrence of birth asphyxia, injuries, jaundice and sepsis.
Postnatally, neonatal infections should be diagnosed and treatedpromptly.Hyperbilirubinemiashouldbemanaged withphototherapyand/orexchange transfusion. Cretinism and galactosemia, if diagnosed and treated in early infancy, have a satisfactory prognosis. Screening of newborn infants by tandem mass spectroscopy helps to diagnose metabolic disorders such as phenylketonuria, biotinidasedeficiency,organicaciduria,hypothyroidismand homocystinuria, permits early treatment thereby averting irreversible brain damage.
Management
The parents should be counseled together. The diagnosis, principles of early stimulation and management should be explained, emphasizing the prognosis. Parental guilt and the home situation should be discussed. Minimal criticism and high appreciation, short-term goals and structuredlearningresults in less withdrawal, aggressive and hostile reactions.
Associated diseases and dysfunctions, e.g. of musculo skeletal system, vision, hearing, locomotion and feeding should be appropriately managed. Anticonvulsive medications such as phenobarbitone should be avoided. Patientswithhyperactivityoftenrespondtoamphetamines including methylphenidate.
Institutionalizationshouldbe avoided. Daycare centers and schools, integrated schools, vocational training centers, sheltered farmsandworkshopsareuseful.Classes should be taken to educate mothers and families in caring for the handicapped and in trying to develop their potential to the maximum, in an effort to make these children as independent as possible.
n i |
i i s |
|
_____________ |
__Ess__e_at_i_P_aectrd- |
_____________ |
_ |
|
|
|||
Suggested Reading
McDonald L, Rennie A, Tolmie Let al. Investigation of global developmental delay. ArchDis Child 2006;91:701-5
Moeschler JB. Genetic evaluation of intellectual disabilities. Semin Pediatr Neurol 2008;15:2-9
Shevell M, Ashwal S, Donley D, et al. Practice parameter: evaluation of the child with global developmental delay: report of the Quality Standards Subcommittee of the American Academy of Neurology and The Practice Committee of theChild Neurology Society. Neurology2003 11;60:367
NEUROCUTANEOUS SYNDROMES
There are five major neurocutaneous syndromes, viz.
(i) neurofibromatosis; (ii) tuberous sclerosis; (iii) von Hippel-Landau disease; (iv)Sturge-Weber syndrome; and
(v) ataxia telangiectasia. Allof these areinherited disorders except for Sturge-Weber syndrome. Clinical profile of these syndromes is diverse, varying from the mild abortive forms to severe potentially fatal disorders.
Neurofibromatosis
Inheritance is autosomal dominant. There are two types: type NFl (von Recklinghausendisease or peripheral NFl) and type NF2 (central neurofibromatosis). Deletion or inactivation of the NF gene on chromosome 17 is responsible for NFl. Gene for NF2 is located on chromo some 22.
NFl. Two or more of the following are present: (i) six or more cafe au lait spots, each over 5 mm in diameter before pubertyorover 15 mm diameter in olderpersons; (ii) two or moreneurofibromasoroneplexiforrnneuroma; (iii)freckling in axillary or inguinal regions; (iv) optic glioma; (v) two or more Lisch nodules; dysplasia of the sphenoid bone or thinning of the cortex of long bones with or without pseudoarthrosis; and (vi) a first degree relative with NFl.
NF2. Presence of bilateral auditory neuroma; unilateral auditory neuroma along with a first degree relative with meningioma, schwannoma or juvenile posterior sub capsular lenticular opacity.
Management comprises supportive care, surveillance for and treatment of new manifestations and surgical management of spinal deformities. Genetic counseling is necessary.
Tuberous Sclerosis Complex
Tuberous sclerosis is an autosomal dominantly neuro cutaneousdisorder. Thepresentingfeatures varywith age.
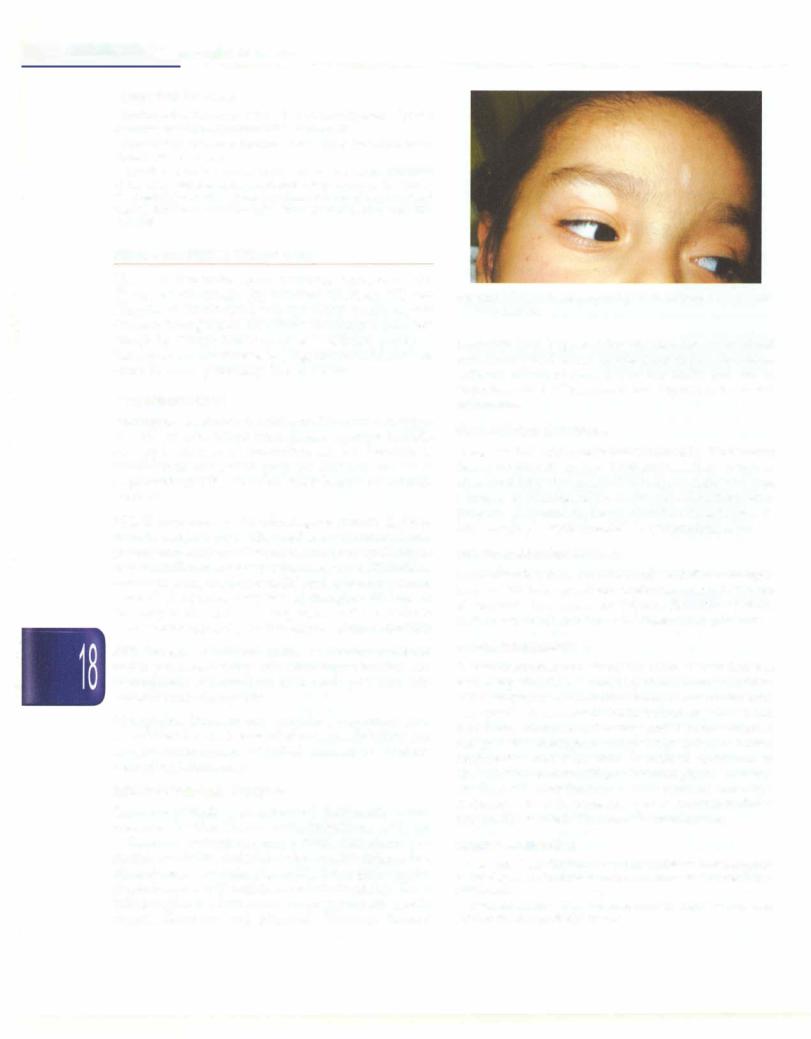
Cardinal features are skin lesions, convulsion and mentalretardation. Early skinlesionsarehypopigmented, ash leaf shaped macules (Fig. 18.11), red or pink papules (angiofibromas) called adenoma sebaceum on face. These enlarge with age. Other lesions are shagreen patches, sub ungual fibromas and gingival fibromas. Retinal
Fig. 18,11: Facial skin showing multiple ash leaf spots in a child with tuberous sclerosis
hamartomamaybepresent. Inearlylifetumorsinheartand kidneys may be detected on ultrasonography. Myoclonic jerks often lead to detection of this entity and are an important cause of West syndrome. Vigabatrin is a useful medication.
Sturge-Weber Syndrome
Sturge-Weber syndrome is characterized by facial nevus flammens (usually in the distribution of first branch of trigeminal nerve but not limited to it), contralateral focal seizures, calcification of the cortex and subcortical struc tures and glaucoma on the same side as the skin lesions. Early surgery is recommended in symptomatic cases.
von Hippel-Lindau Disease
In thisdisorder, there areretinalandcerebellarhemangio blastomas besides spinal cord angiomas and cystic tumors of pancreas, kidneys and epididymis. Patients may show nystagmus, ataxia and increased intracranial pressure.
Ataxia-Telangiectasia
It is an autosomal recessively inherited disease that has beenmappedtochromosomellq. The syndrome manifests with progressive cerebellar ataxia, oculocutaneous telangiectasia, choreoathetosis, pulmonary and sinus infections, immune deficiency and lymphoreticular malignancies. Telangiectasia appears by 2-7 yr on bulbar conjunctiva and even skin. Increased incidence of abnormalmovements,vitiligo, abnormal glucosetolerance are observed. Investigations reveal decreased serum IgA inthree-fourthsof thepatients.Alpha-fetoproteinisalmost universally elevated. Treatment is symptomatic.
Suggested Reading
Ferner RE, Huson SM, Thomas N, et al. Guidelines for the diagnosis and management of individuals with neurofibromatosis l.J Med Genet 2007;44:81-8
Leung AK, Robson WL. Tuberous sclerosis complex: a review. J Pediatr Health Care 2007;21:108-14

Neuromuscular Disorders
Sheffali Gulati
A motor unit comprises one anterior horn cell and all the musclefibers thatitinnervates. Neuromusculardisorders may be due to lesions anywhere along the motor unit. Theseincludeneuronopathies(primarydisordersofante riorhorncell), neuropathies (primarydisordersofaxonor its myelin), neuromuscularjunction disorders and myo pathies (primarydisorders of muscle). A careful history and physical examination help in localizing the disorder within the motor unit.
APPROACH TO EVALUATION
The predominant presenting complaint of a patient with a neuromuscular disorder is weakness. Weakness may also resultfromdisordersoftheupper motorneuron, e.g. cerebral palsy. Weakness due to an upper motor neuron lesionisassociatedwithincreasedtone,briskreflexesand extensor plantar responses. Additional features that suggest central nervous system involvement include seizures and cognitive impairment.
Lower motor neuron lesions are associatedwith signi ficantweakness, hypotonia, depressedreflexesandflexor plantar responses. Anterior horn cell involvement (e.g. spinal muscular atrophy) is associated with wasting, fasciculations and hyporeflexia. Peripheral nerve involvement (e.g. hereditary sensory and motor neuro pathies)isassociatedwithpredominantlydistalweakness, distal wasting, hyporeflexia and sensory involvement. Neuromuscular junction involvement (e.g. myasthenia gravis) classically leads to fatigable and fluctuating weakness.Musclediseases(e.g.musculardystrophies)are associated with proximal weakness and relatively preserved bulk and reflexes. The mode of inheritance is variable, e.g. X-linked recessive in Duchenne muscular dystrophy and Becker muscular dystrophy; autosomal dominant in facioscapulohumeral dystrophy; and autosomalrecessiveinsarcoglycanopathiesandcongenital muscular dystrophies.
The presentation and pattern of disease over time allows definition of possible conditions. For example, musculardystrophy is associated with inexorable weak ness.Metabolicdiseaseandionchannelopathies (periodic paralysis) are associated with episodic course. Inflam matory disorders such as dermatomyositis are associated with waxing and waning course and pain. Cardiac disease often accompanies Duchenne muscular dystrophy and myotonic dystrophy. Skin rash is seen in dermato myositis, while eye involvement is noted in myotonic dystrophy, congenital muscular dystrophies and mito chondrial diseases. Liver involvement may be seen with mitochondrial disorders, acid maltase deficiency and carnitine deficiency.
Laboratory Evaluation
Creatine phosphokinase (CPK), a muscle enzyme, is elevated in mostmusculardystrophies. Muscle biopsy is a frequently performed test thatenables diagnosis based on specific morphological features, immunohisto chemistry (absentorreducedstainingforspecificprotein) and enzyme histochemistry (absent or reduced enzyme function). Electrophysiological tests, including nerve conduction studies and electromyography, help localize the lesion and assess its severity.
Other diagnostic tests include nerve biopsy, antibody testing (e.g. acetylcholine receptor antibodies in myas thenia gravis). Molecular genetic testing is now available for many neuromuscular disorders (spinal muscular atrophy and Duchenne muscular dystrophy).
Suggested Reading
Steven A, Greenberg, Walsh RJ. Molecular diagnosis of inheritable neuromusculardisorders.Part I:Geneticdeterminantsofinherited disease and their laboratory detection. Muscle Nerve 2005;31:418-30
Steven A, Greenberg, Walsh RJ. Molecular diagnosis of inheritable neuromuscular disorders. Part II: Application of genetic testing in neuromuscular disease. Muscle Nerve 2005;31:431-51
587

E_s_se nt ia i P_ e_d_ ia_ t_r_ic_ s__________________________________
____
Hypotonia
Hypotonia is a common sign of neuromuscular disorders. Any lesion along the motor unit can result in peripheral hypotonia, characterized by depressed muscle stretch reflexes andloss of muscle power. The common causes of floppiness in infancy are shown in Fig. 19.l. Hypotonia in utero may result in hip dislocation or multiple contrac tures (arthrogn;posis). The mother may give a history of reduced fetal movements or polyhydramnios.
An alert hypotonic infant with absent deep tendon reflexes, predominantly distal movements and fasci culations is the typical phenotype of spinal muscular atrophy. Neuropathies usually present later in childhood. Atrophy out of proportion to weakness, depressed or absent reflexes and predominantly distal weakness sug gests a nerve disorder. Fatigability, ptosis, proximal mus cle weakness and history of myasthenia gravis in the mother may indicate an underlying neuromuscular junc tion disorder. Predominantly proximal muscle weakness, normal or depressed tendon reflexes and static or impro ving course may indicate a muscle disease. Deep tendon reflexes are preserved in muscle disease or if reduced, are in proportion to the degree of muscle wasting and weak ness. Atrophy is less prominent in muscle disorders.
Central hypotonia is characterized by preserved muscle power and normal or brisk deep tendon reflexes. Some times a child may display features of both central and peripheral hypotonia; common causes of mixed hypotonia include hypothyroidism, motor unit disorders with
superimposed hypoxia, acid maltase deficiency, mito chondrial disorders and infantile neuronal degeneration.
Muscle Weakness in Older Children
Distal weakness is predominantly seen in neuropathies and some muscle disorders like myotonic dystrophy. Proximal weakness has broad differential diagnosis. The child may complain of difficulty in rising from the chair, going up and down the stairs or reaching with their arms. A clinical approach to a child to proximal weakness is summarized in Fig. 19.2. Some disorders such as chronic inflammatory demyelinating polyneuropathy (CIDP) and certain muscular dystrophies show both proximal and distal weakness.
DISORDERS AFFECTING ANTERIOR HORN CELLS
Spinal muscular atrophy and poliomyelitis are the two most common anterior horn cell disorders encountered in children. Besides these, other enteroviruses (e.g. coxsa ckievirus and echovirus), juvenile form of amyotrophic lateral sclerosis and neurometabolic disorders like Tay Sach disease, neuronal ceroid lipofuscinosis and Pompe disease may also involve anterior horn cells.
Spinal Muscular Atrophy
This is an autosomal recessive disease caused by muta tional in the SMN 1 gene, encoding the SMN protein essential for survival of anterior motor horn cells. Three clinical types are recognized. Patients with type 1 disease
Infections
Sepsis/Meningitis; intrauterine infections
P eripheral Hypotonia
Nerve
Charcot-Marie-Tooth disease Congenital hypomyelinating neuropathy Giant axonal neuropathy
Neuromuscular junction
Congenital myasthenia
Transitory myasthenia
Botulism
Neurometabolic condition
Acid maltase deficiency
Biotinidase deficiency
GM1/GM2 gangliosidosis
Lowe syndrome
Peroxisomal disorders
Familial dysautonomia
Benign congenital hypotonia
Anterior horn cell
Spinal muscular atrophy
Muscle
Congenital myopathies Congenital muscular dystrophy
Fig. 19.1: Common etiologies of 'floppy infant'. Maintenance of normal tone requires an intact central and peripheral nervous system

Neuromuscular Disorders -
|
|
|
Proximal muscle weakness |
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
_ |
|
|
|
+ |
+ |
|
|
|
|
- |
|
|
|||||
|
Absent deep tendon reflexes |
!- |
|
|
|
|
|
|
Ptosis |
||||
|
|
-.- |
|||||||||||
|
!Progressive disorder |
|
Reduced or absent |
||||||||||
|
Fasciculations |
± calf hypertrophy |
|
|
deep tendon reflexes |
Ophthalmoplegia |
|||||||
|
Tremors |
- |
|
|
|
Contractures |
I Fatigability |
||||||
|
I Static course |
|
|
|
|
StaticFacialcourseweakness |
Diurnal variation |
||||||
|
|
|
|
||||||||||
|
|
|
Muscular dystrophy |
|
|
Myopathy |
Neuromuscular junction |
||||||
|
|
|
|
|
+_ |
( |
|
|
|
|
disorders |
||
|
|
|
r Rash |
1 |
|
mic fin |
|||||||
|
|
|
|
|
|
||||||||
|
|
|
Systemic features J |
- |
|
|
|||||||
|
|
|
|
Episodic.worsening1 |
|
||||||||
|
|
|
Inflammatory myopathy |
|
Metabolic myopathy |
||||||||
Fig. 19.2: Clinical approach to a child with proximal muscle weakness
(Werdnig-Hoffmann disease) present with profound hypotonia,flaccidweaknessandglobalareflexia (Fig. 19.3). Respiratory weakness, poor swallowing and tongue fasciculations are common. These children usually never learntosit. Aspiration pneumoniaisanimportant causeof morbidity and mortality. Patients with type 2 disease (Dubowitz disease) have onset of illness at6-18months of ageandareusuallyable tositunaided. Theymaydevelop kyphoscoliosis, tremors (polyminimyoclonus), poor swallowing and respiratory insufficiency. Patients with type 3 disease (Kugelberg-Welander disease) present later in childhood (>18 months) and are usually able to walk. These children are often misdiagnosed as limb girdle muscular dystrophy or myopathy. Global areflexia, fasciculations, tremors and electrophysiology may give a clue towards underlying anterior horn cell pathology.
Treatmentis usuallysupportiveandincludesrespiratory care, management of problems in feeding andswallowing,
Fig. 19.3: A 5-month-old boy presented with motor delay and repeated chest in fections. Examination revealed generalized hypotonia, absent deep tendon reflexes, poor muscle power and tongue fasciculations. Note the 'frog-like' posture and subcostal retractions due to respiratory muscle weakness. A diagnosis of spinal muscular atrophy type 1 was made
ensuring adequate nutrition, treatment for gastroeso phageal reflux, orthopediccareand rehabilitation, appro priateimmunizationandfamilyeducationandcounseling. Therapeutic agents undergoing evaluation include valproate, gabapentin, aminoglycosides and riluzole.
Suggested Reading
Lunn MR, Wang CH Spinal muscular atrophy. Lancet 2008; 371:2120--33 Wirth B, Brichta L, Hahnen E. Spinal muscular atrophy: from gene to
therapy. Sernin Pediatr Neurol 2006;13:121-31
PERIPHERAL NEUROPATHIES
Most neuropathies are chronic. Guillain-Barre syndrome is the most common cause of acute neuropathy. A clinical approach to a childwithsuspected peripheralneuropathy is shown in Fig. 19.4. The clinical presentation, electro physiological characteristics and ancillary laboratory studies may help narrow down the differential diagnosis in a child with suspected peripheral neuropathy, as discussed below.
Type of neuropathy. Most neuropathies are primarily axonal. Finding a demyelinating pattern narrows the differential diagnosis. Clinical pointers to a demyelinating process include: (i) presence of global areflexia; (ii) mode rate to severe muscle weakness with relative preservation of bulk; (iii) predominantly motor symptoms; and (iv) hypertrophy of nerves. The differentiation between the two types of neuropathy is mainly electrophysio logical. Electrophysiologically, demyelination is suggested by: (i) decreased conduction velocity; (ii) prolonged distal latencies and late responses; (iii) asymmetry; (iv) presence of conduction block; and (v) abnormal temporal disper sion (suggesting an acquired process). Axonal disorders show decreased compound muscle action potentials with preserved conduction velocity and distal latencies.
Pattern ofneuropathy. Most polyneuropathies show distal to-proximal gradient of symptoms and signs ('length

-.._E_ssentia l e at s
P__id irc__----------------------------------
Suspected peripheral neuropathy
|
|
|
|
|
|
|
|
|
|
|
|
|
|
t-----i |
|||
|
|
|
|
|
I |
|
|
|
---* |
|
|
Demyelinating |
|
|
|||
|
|
|
|
|
|
|||
---... |
-----*--- |
|||||||
Acquired |
|
Hereditary |
||||||
AIDP orCIDP |
Charcot-Marie-Tooth |
|||||||
Diphtheria |
|
disease 1 and 3 |
||||||
Toxic, e.g. arsenic |
|
Metachromatic |
||||||
|
|
|
|
|
leukodystrophy |
|||
|
|
|
|
|
Krabbe'disease |
|||
|
|
|
|
|
Adrenoleukodystrophy |
|
||
' MononeuropathyJ
Trauma
Focal compression Entrapment
tern! |
|
||
|
I |
|
Polyneuropathy |
mmetric with |
|||
stepwise progression |
I (involvement of 22 nerves) |
||
_ |
|
||
Mono!euritis multiplex , |
-i |
||
Vasculitis |
Guillain-Barre syndrome |
||
Leprosy |
Charcot-Marie-Tooth disease type2 |
||
Leukemia, lymphoma |
Human immunodeficiency virus |
||
Porphyria |
Deficiency of vitamin 612 or E |
||
Cryoglobulinemia |
Induced by chemotherapy |
||
|
|
|
Porphyria |
|
|
|
Diabetes |
Fig. 19.4: Approach to peripheral neuropathies in childhood. Mononeuritis multiplex refers to the involvement of multiple separate non contiguous peripheral nerves, either simultaneously or serially. AIDPacute inflammatorydemyelinating polyneuropathy; CIDP chronic inflammatory demyelinating polyneuropathy
dependent' or'dying back' pattern). More proximal nerves may be involved rarely, e.g. inflammatory demyelinating polyneuropathy and porphyria. The presence of asym metry and a stepwise progression may point towards mononeuritis multiplex. Mononeuropathies are rarely encountered in pediatric practice and are usually due to trauma, focal compression or entrapment.
Typeofnervefiberinvolved.Neuropathiesthatpredominantly affect large fibers result in sensory deficits (impaired touch or vibration), weakness and loss of deep tendon reflexes. Small fiber neuropathies present withdistalsensorydeficit, painful burning dysesthesias and autonomic dysfunction. Pure sensory neuropathies are unusual.
Hereditary Neuropathy
A slowly progressive course, prominent sensory signs in absence of sensory symptoms, foot deformities and a family history point towards an inherited neuropathy. The hereditary neuropathies encountered in children are listed in Table 19.1. Charcot-Marie-Tooth disease is the most common hereditary neuropathy, and the most common peripheral neuropathy in children.
The phenotype of a child with Charcot-Marie-Tooth diseaseconsists of distal weakness and wasting, especially of the peroneal compartment ('stork leg' appearance; Fig. 19.5), some distal sensory impairment, skeletal deformities, contractures and diminished or absent deep tendon reflexes. The clinical features, electrophysiological characteristics, inheritance pattern and, occasionally, features on nerve biopsy, suggest a specific hereditary neuropathy and guide further evaluation.
Guillain-Barre Syndrome
This is a common cause of acute flaccid paralysis (AFP) in children. It is an immune-mediated, rapidly progressive, predominantly motor,symmetric polyradiculoneuropathy that often leads to bulbar and respiratory compromise. Many subtypes are described and include acute inflam matory demyelinating polyradiculoneuropathy, acute motor axonal neuropathy, acute motor and sensory neuropathy, acute sensory neuropathy, acute pan dysautonomia and the Miller Fisher syndrome.
The condition can occur at any age. About two-thirds patients have an antecedent infection within 6 weeks prior
Table 19.1: Hereditary neuropathies Primary disease
Charcot-Marie-Tooth disease
Hereditary neuropathy with liability to pressure palsies Hereditary sensory and autonomic neuropathies Distal hereditary motor neuropathies
Hereditary neuralgic amyotrophy Familial amyloid polyneuropathy
Multisystem disorder
Lipid metabolism
Leukodystrophies
Phytanic acid storage disorder Sphingomyelin lipidoses Porphyria
Defective DNA repair: Ataxia-telangiectasia, xeroderma pigmentosa
Hereditary ataxias: Friedrich ataxia, spinocerebellar ataxia Miscellaneous: Neuroacanthocytosis, mitochondrial disorders

Figs 19,SA and B: A 7-yr-old boy presented with progressive gait difficulties, frequenttwisting ofankles, foot deformities and progressive thinning of legs. Examination revealed distal weakness and wasting, absent anklereflexes and enlarged common peroneal nerves. (A) Note the 'stork leg' appearance of legs with foot deformities; and (B) hand deformities. A diagnosis of Charcot-Marie-Tooth disease was made
to symptom onset, generally an upper respiratory tract infection or gastroenteritis. The clinical manifestations include acute onset of symmetrical ascending weakness that is both proximal and distal. Facial weakness is fre quent, and involvement of respiratory muscles occurs in one-fourthcases. Dysautonomiais common and issugges tedbytachycardia, arrhythmia,ileus,bladderdysfunction, labile blood pressure and impaired thermoregulation. The weakness usually reaches a nadir 2-4 weeks after onset of symptoms and is followed by gradual recovery over weeks to months. The illness is usually monophasic but 7-16% patients may suffer from recurrent episodes of worsening after an initial improvement. As compared to demyelinating forms, the axonal form of Guillain-Barre syndrome exhibits a more rapid and severe course, with frequent involvement of respiratory muscles and cranial nerves and infrequent and mild involvement of the autonomic nervous system. The Miller Fisher syndrome is characterized by the triad of ophthalmologica1 abnor malities, ataxia and areflexia.
Diagnosis depends on clinical features, e1ectrophysio logical findings and cerebrospinal fluid examination. Electrophysiology may reveal absent F-responses or H-reflexesandreduced compound muscle actionpotential
Neuromuscular Disorders -
or sensory nerve action potential in axonal forms of the illness. Prolonged distal latencies, reduced conduction velocities, abnormaltemporal dispersion and conduction blocksare notedin demyelinating types. The cerebrospinal fluid protein concentration is raised in 80% cases, while mononuclear cell count is either normal (albuminocyto logic dissociation) or below 50 cells/mm3. Electrophysio logical studies and cerebrospinal fluid analysis may be normal during the first week of the illness.
Immunotherapy is the mainstay of treatment. Intra venous immunoglobulin (IVIG, 2 g/kg over 2-5 days) should be administered orplasmaexchangesperformedif the child presentswithin 2-4 weeks of onset of symptoms. Suchtreatmentisindicatedinnonambulatorypatients, but their role in mildly affected patients who are mobile is unclear. Plasmaexchangesmayhastenrecoverycompared to supportivetreatment alonein adultpatients. Inpatients with severe disease, therapy with IVIG (if initiated within twoweeksfromonset)hastensrecoveryasmuchasplasma exchange and is more likely to be completed than plasma exchange. Further, giving IVIG after plasma exchange did not confer significant extra benefit. Low quality evidence suggests that IVIG probably hastens recovery in children compared with supportive care alone. Information on appropriate therapy is limited for patients with mild diseaseandinthose where treatment startsmorethan two weeks after onset. Patients who do not respond to initial treatment with IVIG may benefit from a second course of therapy. General supportive care includes cardiorespi ratory care, physical therapy, nutritional management, management of neuropathic pain, care of bladder and bowel and prevention of deepvein thrombosis.
Chronic Inflammatory Demyelinating
Polyradiculoneuropathy
Thisuncommonconditionisslowlyprogressive (>4 weeks) or relapsing and has symmetric proximal and distal weakness in the upper and lower extremities with concomitant sensory loss. Asymmetric forms, distal predominant forms and sensory predominant forms also occur. The minimum duration of symptoms to reach the troughinpatientswith chronicinflammatorydemyelinating polyradiculoneuropathy is 2 months. This helps to distinguish this condition from Guillain-Barre syndrome, which usually evolves in less than 4 weeks. Electro physiology and nerve biopsyhelpin diagnosis. Treatment modalities for chronic inflammatory demyelinating polyradiculoneuropathy include IVIG, plasma exchange and prednisolone. Spontaneous remission of chronic inflammatory demyelinating polyradiculoneuropathy is rare, and most patients require longterm immuno modulating therapy.
Suggested Reading
Hughes RA. Give or take? Intravenous immunoglobulin or plasma exchange for Guillain-Barre syndrome. Crit Care 2011;15(4):174

__E_s e_stn__ial__P e idatri_sc__________________________________
Joint Task Force of the EFNS and the PNS. European Federation of Neurological Societies/Peripheral Nerve Society Guideline on management of chronic inflammatory demyelinating polyradiculo neuropathy. Report of aJoint Task Force of the European Federation of NeurologicalSocietiesand thePeripheralNerveSociety.J PeripherNerv Syst 2005; 10:220-8
Vavra MW, Rubin DI. The peripheral neuropathy evaluation in an office based neurlogy setting. Semin Neurol 2011;31:102-4
Wilrnshurst JM, Ouvrier R. Hereditary peripheral neuropathies of childhood: a brief overview for clinicians. Neurornuscul Disord 2011;21:763-7
ACUTE FLACCID PARALYSIS
Acute flaccid paralysis (AFP) is a clinical syndrome char acterized by rapid onset of weakness, progressing to maximum severity within severaldays toweeks. The term 'flaccid' refers to the absence of spasticity or other upper motorneuronsigns.At the41stWorldHealthAssemblyin May 1988, the resolution to eradicate polio was passed. In the Global Polio Eradication Initiative, acute flaccid paralysis is defined asanycase ofAFPin a child aged <15 yr, or any case of paralytic illness in a person of any age when polio is suspected. It can result from involvement at anypointinthemotorunit. Commoncausesofacuteflaccid paralysis include Guillain-Barre syndrome, poliomyelitis, transverse myelitis, traumatic neuritis, postdiphtheric neuropathy and nonpolio enteroviral illnesses.
Over the last few years the number of cases of polio myelitis has been going down. In 2009, there were 741 cases of poliomyelitis and in 2010, there were 42 cases. The last case of confirmed wild poliovirus (Pl type) was reported from West Bengal in 2011.
The differential diagnosis of acuteflaccidparalysisvaries considerablywith age. The commoncauses are enumerated in Table 19.2. The differentiating features between the common causes of acute flaccid paralysis are summarized in Table 19.3.
Acute Flaccid Paralysis (AFP) Surveillance
Allpatientswith acute flaccidparalysisshould bereported to Surveillance Medical Officer of World Health Organi zation. Every case of AFP within the last 6 months has to be reported. Additionally, other conditions which need
Table 19.2: Differential diagnoses of acute flaccid paralysis
Muscle disorders |
Inflammatory myopathy |
|
Periodic paralysis |
|
Hypokalemia |
|
Infections |
Neuromuscular |
Myasthenia gravis |
junction disorders |
Botulism |
|
Eaton-Lambert syndrome |
Neuropathies |
Guillain-Barre s.yndrome |
|
Traumatic neuritis |
|
Postdiphtheric neuropathy |
|
Porphyria |
|
Vasculitis |
Anterior horn |
Poliomyelitis |
cell disorders |
Nonpolio enteroviruses |
Spinal cord disease |
Transverse myelitis |
|
Spinal cord compression |
|
Trauma |
Table 19.3: Differentiating among common causes of acute flaccid paralysis
|
Poliomyelitis |
Gui/lain-Barre syndrome |
Transverse myelitis |
Traumatic neuritis |
Fever |
Present; may be |
May have a prodromal |
May have a |
Absent |
|
biphasic |
illness |
prodromal illness |
|
Symmetry |
Asymmetric |
Symmetrical |
Symmetrical |
Asymmetric |
Sensations |
Intact; may have |
Variable |
Impaired below the |
May be impaired in |
|
diffuse myalgias |
|
level of the lesion |
distribution of the affected |
|
|
|
|
nerve |
Respiratory |
May be present |
May be present |
May be present |
Absent |
insufficiency |
|
|
|
|
Cranial |
Affected in bulbar |
Usually affected |
Absent |
Absent |
nerves |
and bulbospinal |
|
|
|
|
variants |
|
|
|
Radicular |
May be present |
Present |
Absent |
Absent |
signs |
|
|
|
|
Bladder, |
Absent |
Transient; due to |
Present |
Absent |
bowel complaints |
|
autonomic dysfunction |
|
|
Nerve |
May be abnormal |
Abnormal |
Normal |
Abnormal |
conduction |
|
|
|
|
CerebrospinaI |
Lymphocytic |
Albumino-cytologic |
Variable |
Normal |
fluid |
pleocytosis; |
dissociation |
|
|
|
normal or |
|
|
|
|
increased protein |
|
|
|
MRI spine |
Usually normal |
Usually normal |
Characteristic* |
Normal |
* Local enlargement of the spinal cord and increased signal intensity over several spinaJ segments


___E_s_s__en_t_ai_1_P_e_d_ai_t_r_ic_s _______________________________
Transitory neonatal myasthenia may occur in about 15% of babies born to myasthenic mothers. Symptoms usually start within few hours afterbirth but may be delayed till the third day. These include difficulty in feeding, weak cry, hypotonia, lack of facial expression and respiratory insufficiency. Supportive care suffices in majority of the cases. Oral or intramuscular pyridostigmine, usually for 4-6 weeks, may be warranted in severe cases.
Edrophonium testing is usually the first test performed in a suspected case of myasthenia gravis. The dose used is 0.1-0.2 mg/kg [may be repeated every minute to a total maximum dose of 5 mg (weight <34 kg) or 10 mg (weight >34 kg)]. Effects are seen within 10 seconds and persist till 120 seconds. A positive result consists of transient resolution of the clinical sign (ptosis/ophthalmoplegia/ dysarthria)underobservation.Edrophoniumis notrecom mended for use in infants due to high risk of arrhythmias and short duration of action which precludes objective assessment. Neostigmine can be used as a diagnostic test by intramuscular injection. The dose used is 0.125 mg/kg in an infant and 0.04 mg/kg in an older child. It is slower in action, with anticipated response in 10-15 min and maximum in 30 min (Fig. 19.6). If the result is equivocal or negative, the dose may be repeated in 4 hr.
Repetitive nerve stimulation studies are abnormalin 50-70% cases with generalized myasthenia gravis. A decrement of >10% is characteristic. Electromyography may be normal or may show unstable or myopathic muscle unit action potentials. Single fiber electromyography is more sensitive and may show increased jitter or blocking.
Acetylcholine receptor (AChR) antibodies may be positiveinchildrenwith myastheniagravis. Thepositivity rates are lower in periand prepubertalchildren(50-60%). Antibodies to muscle specific kinase (Anti-MuSK) antibodies may be demonstrable in 40% seronegative
Figs 19.6A and B: A 9-yr-old boy presented with drooping of eyelids, more in the evening than morning, and restricted eye movements. Examination revealed asymmetric ptosis, external ophthalmoplegia, normal pupils and normal motor examination. Neostigmine challenge test was performed. Note the improvement in ptosis between (A) before and (B) after administration of neostigmine. A diagnosis of juvenile myasthenia gravis was made
myasthenia gravis patients. X-ray chest or CT of antt mediastinummay show thymoma or thyrnic hyperpl.
Congenital Myasthenia Syndromes
The congenital myasthenia syndromes are exception. rare.Theyshouldbesuspectedinseronegativemyasthe gravis, floppyinfantwith underdevelopedmuscles anc adults with childhood history of difficulties affecti cranial, respiratory, truncalorlimb muscles. CommonfE tures include hypotonia, limb weakness, feedi1 difficulties, respiratorydifficulties, arthrogryposis, ptosi ophthalmoparesis, dysphagiaand dysarthria. The clinic. presentation, electrophysiological features and geneti studies help to differentiate betweenthese subtypes. The. do not respond to steroids and other immunosuppres sants. Conditions like endplate acetylcholinesterast deficiency and slow channel congenital myasthenia may worsen with pyridostigmine.
Treatment
Cholinesterase inhibitors are usually the initial treatment for myasthenia gravis. Pyridostigmine is commonly used at doses of 1-7 mg/kg/day in 4 divided doses. Oral ste roids may also be usedin anonacutesetting.Prednisolone is started at low doses (0.5 mg/kg/day) and titrated according to clinicalresponse.Azathioprine, cyclosporine, cyclophospharnide and mycophenolate mofetilhave been used as steroidsparingdrugs or forrefractorycases. Drugs that interfere with neuromuscular transmission (Table 19.4) should be used with caution. Thymectomy in seropositive patients may be beneficial.
A myasthenic crisis necessitates cardiorespiratory monitoring and support. It should be differentiated from cholinergic crises due to overdosage of acetylcholine esterase inhibitors. Antecedent events, predominance of cholinergic symptoms, ice pack test and edrophonium challenge test may help to differentiate between the two entities. IVIG or plasmapheresis may be required.
Suggested Reading
Chiang LM, Darras BT, Kang PB. Juvenile myasthenia gravis. Muscle Nerve 2009; 39:423-31
Finsterer J, Papi.-e L, et al. Motor neuron, nerve and neuromuscular junction disease. Curr Opin Neural 2011;24:469-74
Patwa HS, Chaudhry V, Katzberg H, Rae-Grant AD, So YT. Evidence based guideline: intravenous immunoglobulin in the treatment of neuromuscular disorders: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neural 2012;78:1009-15
MUSCLE DISORDERS
Congenital Myopathies
The congenital myopathies are a diverse group of muscle disorders caused by genetic defects in the contractile apparatus of the muscle and defined by distinctive histo chemical or ultrastructural changes on muscle biopsy. Majority of these disorders present as 'floppy infant'
