
Ghai Essential Pediatrics8th
.pdf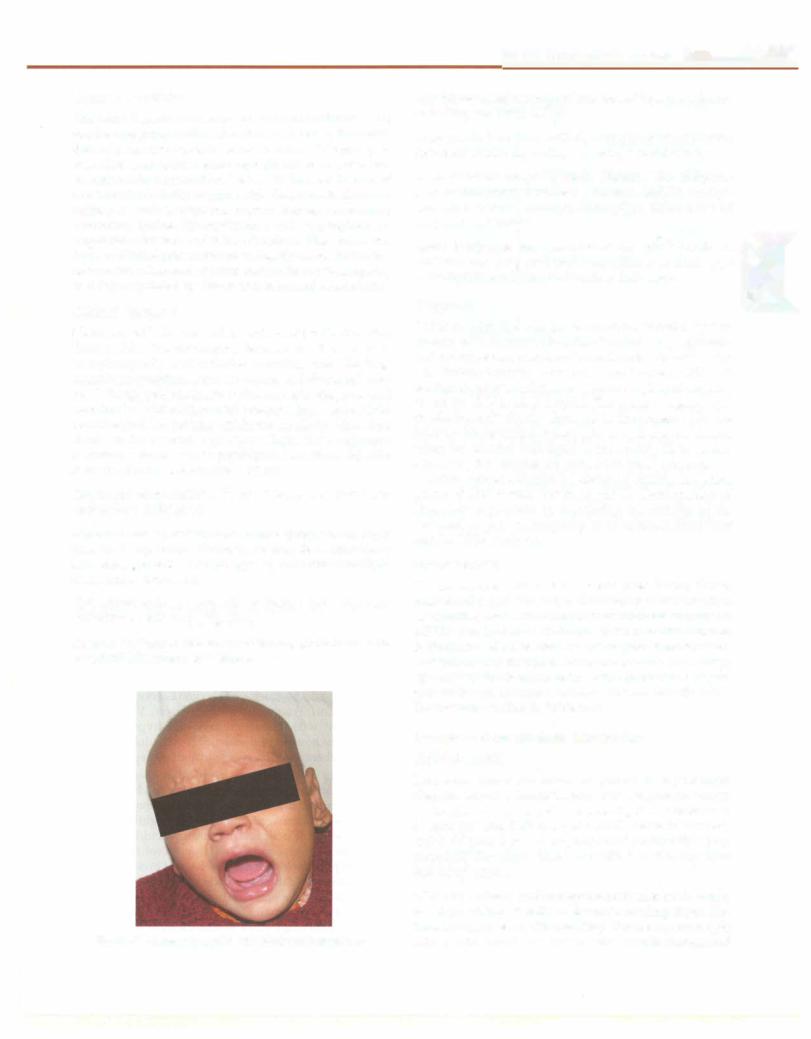
Organic Acidurias
The term "organic acidemia" or "organic aciduria" (OA) applies to a group ofdisorderscharacterizedby the excre tion of nonamino organic acids in urine. This group of disorders results from enzyme deficiencies in pathways of amino acid degradation. Defects in the metabolism of the branched-chain amino acids (leucine, isoleucine, valine) as well as tyrosine, homocysteine, methionine, threonine, lysine, hydroxylysine and tryptophan are responsible for most of these disorders. They have two types of clinical presentations: an insidiousonset with few to no acute crises and an acute metabolic encephalopathy that is precipitated by illness and increased catabolism.
Clinical Features
Neonates with OA are well at birth and for the first few days of life. The presenting features are that of toxic encephalopathy and includes vomiting, poor feeding, neurologic symptomssuchasseizuresandabnormaltone, and lethargy progressing to coma. An early diagnosis and treatment results in improved outcome. In the older child or adolescent, OApresentwithloss of intellectualfunction, ataxia or focal neurologic signs, Reye like syndrome, recurrent ketoacidosis or psychiatric symptoms. Specific features of some OA are listed below.
Cutaneous abnormalities. Perioral eruption (multiple carboxylase deficiency).
Abnormal urinary or body odor. Maple syrup/burnt sugar (maple syrup urine disease), sweaty feet (isovaleric acidemia, glutaric aciduria type 2), cat urine (multiple carboxylase deficiency).
Hair abnormalities. Alopecia or sparse hair suggests biotinidase deficiency (Fig. 23.6).
Dysmorphicfeatures. Mevalonic aciduria, glutaric aciduria type 2,3(0H)isobutyric aciduria.
Fig. 23.6: Alopecia in a child with biotinidase deficiency
Inborn Errors of Metabolism -
Hypoglycemia andneurologicalsymptoms. Organicacidurias, including late onset MSUO.
Acute ataxia. Late onset MSUD, methylmalonic acidemia, isovaleric acidemia, multiple carboxylase deficiency.
Acute metabolic encephalopathies. Glutaryl-CoA dehydro genase deficiency, isovaleric acidemia, MSUD, methyl
malonic acidemia, multiple carboxylase deficiency and I propionic acidurias.
Acute hemiplegia and metabolic stroke. Methylmalonic acidemia and propionic acidemia, glutaric aciduria type 1, methylcrotonyl-CoA carboxylase deficiency.
Diagnosis
Patients with OA can have acidosis, ketosis, hyper ammonemia, abnormal liver function tests,hypoglycemia and neutropenia. Analysis of urine for organic acids using gas chromatography with mass spectrometry (GCMS) enables diagnosisandplasmaorserumacylcarnitineprole tested by TMS is often helpful. The urinary organic acid profile is nearly always abnormal in the presence of acute illness with decompensation.However, it may be normal when the affected individual is not acutely ill; in certain disorders, the analytes are present in small amounts.
Urine samples should be obtained during the acute phase of illness and frozen at -20°C. Confirmation of diagnosis is possible by measuring the activity of the deficient enzyme in lymphocytes or cultured fibroblasts and/or DNA analysis.
Management
The management of OA duringacutecrises followsabove mentioned principles. Adjunctive therapy with cofactors or vitamins, suchas thiamine to treatthiamine-responsive MSUD and hydroxycobalamin to treat methylmalonic acidemia isuseful.Fordisorders ofpropionatemetabolism, intermittent administration of metronidazole (10-15 mg/ kg/day for 10-15 days) reduces the production of pro pionate by gut bacteria. Variouscofactors and adjunctive therapy are detailed in Table 23.4.
Defects of Carbohydrate Metabolism
Galactosemia
There are three disorders of galactose metabolism (Fig. 23.7),butit isthedeficiencyoftheenzyme galactose- 1-phosphate uridyltransferase (GALT), that is referred to as galactosemia. Deficiency of GALT results in accumu lation of galactose-1-phosphate and metabolites (e.g. galactitol) that might have toxic effect on the, e.g. liver and other organs.
Clinical features Patients appear normal at birth, but by 3-4 days of breast milk or formula feeding show life threatening disease with vomiting, diarrhea,poor weight gain, predominant hepatic and renal manifestations and

|
E s s en t ia P ed iat rics |
___________________________ |
|
|
___ |
_ _ _ _ _ _ _ _ _ _ _ _ _ _ ________ |
|
|
|
||
|
Galactitol + - - 1'!95! '!.d':!91 ':... - - - . Galactos e |
Hereditary Fructose Intolerance |
|
= |
' |
""'" |
|
4'wep1merase |
|
p |
hos hat |
p |
|
|
DP |
( |
|
-
glucos
Galactokinase |
The condition occurs due to deficiency of the enzyme, |
|
aldolase B. Symptoms occur following ingestion of |
||
fructose or sucrose and presentwith intractable vomiting |
||
and symptomatic hypoglycemia. Prolonged exposure |
||
|
|
results in failure to thrive, irritability, hepatomegaly, |
|
|
abdominal distension, edema and jaundice. Milder |
e Glalaotooe-::,:::,h::. ,•variantsare common andpresentwith bloating, abdominal |
||
|
undyltransferase |
distension and diarrhea. Investigations show hypo |
Glucose-1-phosphate |
glycemia, marked lactic acidosis, hyperuricemia, hypo |
|
phosphatemia, hyperchloremic metabolic acidosis, |
||
generalized aminoaciduria and deranged prothrombin |
||
and partial thromboplastin time and liver function tests. |
||
1 |
Phosphoglucomutase |
Confirmation is done by demonstration of deficiency of |
aldolase B in fresh liver biopsy sample. Fructose free diet |
||
Glucos e-6-phos phate |
is therapeutic. |
|
Fig. 23.7: Disorders of galactose metabolism |
Glycogen Storage Diseases |
cataract. Jaundice and liver dysfunction are progressive and appear at the end of first or during second week of life. The disease may present initially with indirect hyperbilirubinemia due to hemolysis secondary to high
levels of galactose-1-phosphate in erythrocytes. Many affectedinfants die of Escherichia coli sepsis in the neonatal
period. Untreatedinfants, if survivingtheneonatalperiod, have persistent liver disease, cataracts and severe mental retardation. Alternatively, the effects of acute galactose toxicity may rarely cause predominant neurologic symptoms. Renal tubular disease presentswith metabolic acidosis, galactosuria, glucosuria and aminoaciduria (Fanconi syndrome).
Diagnosis The diagnosis is confirmed by either enzyme or specific mutational analysis. In case of suspected galactosemia, the urine should be tested simultaneously with Benedict reagent and by glucose oxidase method. A negativedipstickbyglucoseoxidase methodwithpositive Benedict reactionindicatesnonglucosereducingsubstances, e.g. galactose or fructose. A negative test does not eliminate the possibility of these disorders, especially if thepatienthasreceivedintravenous glucoseformorethan a few hours. If the diagnosis of galactosemia is suspected, whether or not urinary reducing substances are found, galactose-containing feedingsshould bediscontinuedand replaced by soy based or lactose free formula pending results of confirmatory enzyme assay or genetic studies.
Galactokinase deficiency Galactosemia due to
galactokinase deficiency is rare and has mild mani festations.Theonly significant abnormality iscataract due to accumulation of galactitol. Liver, kidney and brain damage are not seen. Galactose free diet, if started early, leads to clinical improvement and prevents further damage. Mental retardation, if already present does not improvewiththerapy.Galactoserestricteddiet isrequired throughout life.
Glycogen is an extensively branched polysaccharide macromolecule formed by thousands of glucose units joined into chains by o:-1-4 and o:-1-6 bond. Ingested carbohydrate isabsorbedasglucose via theportal system. The glucose isphosphorylatedtointermediatecompounds (glucose-6-phosphate and glucose-1-phosphate) and is storedas glycogen. Glycogen is the mainglucosereservoir in the liver and provides energy between meals or during fasting. In muscle, it provides energy for contraction. Whenperipheral glucose isutilizedandglucoselevelsfall, glycogen is depolymerized, bonds at branch points are split and free glucose is released into blood by hydrolytic dephosphorylation. The final reaction is mediated by the enzyme glucose-6-phosphatase. The series of reactions causing release of glucose are called glycogenolysis (Fig. 23.8). Any defect in the synthesis and degradation of glycogen causes glycogen storage disease (GSD). Several disorders of glycogen metabolism are described; these are subdivided into liver and muscle glycogenoses (Table 23.6).
Hepatic glycogenoses GSD Ia (von Gierke disease), lb, type IIIa (Cori/Forbes), IIIb, IV(Anderson), VI (Hers) and IX present with hepatomegaly and hypoglycemia. Figure 23.9 shows a childwithGSDIwith'doll like fades' with protuberant abdomen due to marked hepatomegaly.
GSD I is distinguished from other disorders that primarily affect liver by markedly elevated lactic acid as well as elevated uric acid and cholesterol concentrations. GSD III is characterized by normal or slightly increased concentrations of lacticacid, normaluric acid, but a greater elevation of triglycerides and cholesterol than GSD I. Creatinephosphokinasemay be elevatedin olderchildren and adolescents if there is muscle involvement. GSD III is subdividedintopatientswhohave nomuscleinvolvement (IIIb) and those who develop muscle weakness by their teenage years (Illa). GSD VI and IX have more benign courses than GSD I and III. Hypoglycemia is less severe,

Table 23.6: Enzymatic deficiencies in common glycogenoses
Type |
Enzyme defect |
Common name |
Liver glycogenoses |
|
|
Ia |
Glucose-6-phosphatase |
von Gierke |
lb |
Glucose-6-phosphate |
|
|
translocase |
|
Illa |
Liver and muscle |
Cori/Forbes |
|
debrancher deficiency |
|
|
(amylo-1, 6-glucosidase ) |
|
Illb |
Liver debrancher |
|
|
deficiency only |
|
IV |
Brancher enzyme |
Anderson |
|
(a-1, 4 glucan: |
|
|
a-1, 4 glucan-6-a |
|
|
glucosyl transferase) |
|
VI |
Liver phosphorylase |
Hers |
IX |
Phosphorylase kinase |
|
Muscle glycogenoses |
|
|
II |
Lysosomal alpha-1, |
Pompe |
|
4-glucosidase (acid |
|
|
maltase) |
|
V |
Muscle phosphorylase |
McArdle |
VII |
Phosphofructokinase |
Tarui |
and hepatomegaly resolves after puberty. GSD IV (Anderson amylopectinosis-brancher enzyme deficiency) leads to formation of an abnormal glycogen that appears to be noxious to the liver. Severe liver disease develops in the Ist few months afterbirth, leading to cirrhosis. Unlike the other primarily liver disorders, it often causes severe liver failure. Liver failure with portal hypertension sug gests GSD IV.
Work up should be done in patients with hypoglycemia and hepatomegaly. Concentrations of glucose, uric acid, lactic acid, liver transaminases and lipids (cholesterol and triglycerides) are helpful in differentiating type I and III. Enzyme assay in fresh liver tissue confirms the diagnosis of the liver GSD. DNA testing is increasingly available for these disorders, alleviating the need for liver biopsy. Muscle glycogenoses GSD V (McArdle disease), VII (Tarui) and II (Pompe) primarily involve muscle. GSD V and VII often present in adolescence with exercise intolerance and myoglobinuria. These patients may have muscularhypotonia,weakness,easyfatigabilityandmuscle cramps. A muscle biopsy may be necessary to confirm the diagnosis. DNA testing now offers an alternative and helps to distinguish between type V and type VII.
Type II (Pompe), disease results from lysosomal storage of glycogen in skeletal muscles, cardiac muscles and cen tral nervous system. There isprogressivecardiomyopathy. Electrocardiogram shows left axis deviation, short PR interval and large QRS. Heart failure with dyspnea and cyanosis may occur. Skeletal musclesshow hypotonia and marked weakness (Figs 23.lOA to D). The tongue is large
Inborn Errors of Metabolism --
and protruding. Death usually occurs before the age of 1 yr. The diagnosis is suggested by low levels of the enzyme acid maltase in leukocytes, liver, muscles and fibroblasts. Treatment Therapy of hepatic glycogenoses is targeted to maintain normoglycemia and is achieved by continuous nasogastricinfusionofglucoseoruncookedstarch.Depend
ing on response, frequent daytime feeds and continuous I nasogastricfeedingat night may be given. Uncooked starch
acts as a slow release form of glucose. This is especially useful in type I, III and IV but most demanding in type I. The intake of lactose, fructose and sucrose should be restricted, except fruits, vegetables and small amounts of milk products. Enough nutrients, vitamins and minerals should be given. If despite optimizing dietary treatment, serum triglyceride levels remain above 900 mg/dl, trigly ceride-lowering drugs (nicotinic acid, fibrates) should be recommendedtoreduceriskof cholelithiasis andpancreati- tis. Allopurinol (10 mg/kg per day, divided into3 dosages) should be given for hyperuricemia. Enzyme replacement therapy (ERT) isavailableand very effective for typeII GSD but the cost is prohibitive.
Mitochondrial Fatty Acid Oxidation Defects
Pathogenesis
Fattyacidoxidationplays amajorrole inenergyproduction during fasting or periods of high-energy demand leading to glycogen depletion. It involves three processes:
a.Mobilization of fatty acids into mitochondria. Long chain fatty acids (C14-20) undergo active transport through carnitine shuttle; whereas short (C4 to 6) and medium chain (Cl2) fattyacidsentersindependentlyofcarnitine andareactivatedtocoenzyme A (CoA)esters.Disorders of carnitine cycleincludescarnitine palmitoyl transferase I and II deficiency.
b.oxidation.This involvesremoval of 2-carbonfragments (i.e. acetyl-CoA) from the transported saturated fatty acids via a four-step enzymatic reaction. Each enzyme has different chain length specificity. Deficiency of various acyl-CoA dehydrogenases (AD) results in short chain AD (SCAD) deficiency, medium chain AD (MCAD) deficiency, long chain AD (LCHAD)andvery long chain AD (VLCAD) deficiency.
c.Electron transfer to the respiratory chain. Acetyl-CoA is utilized as energy substrate in muscle and liver. Exam ple glutaric acidurias type II (multiple acyl-CoA dehy drogenase or MAD deficiency).
Clinical Features
Features may have varying severity and present at any age. Symptoms are precipitated by fasting, exercise or intercurrent illness leading to episodes of metabolic decompensation.
i.Presence of acutehypoketotichypoglycemiaand ence phalopathy, associated with Reye like illness, hepato megaly and liver dysfunction.

|
E |
s s e n t ia P e d i atric s |
|
|
|
|
|
|
|
|
|
______________ |
||||||||
|
|
|
|
____________ |
|
|
|
_ |
||||||||||||
___ |
|
|
|
|
|
|
||||||||||||||
|
_ _ |
_ _ _ _ _ _ _ _ |
_ |
_ _- |
_______ |
|
|
Phosphory ase kinase |
VIII |
|
||||||||||
|
|
|
|
|
|
|
|
|
|
l |
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
G ycogen |
|
|
|
|
l liver |
GSD |
|
|||
Lysosome ..,,-- |
|
|
|
|
|
|
|
|
|
|
+ |
Muscle |
GSDIX |
|
||||||
|
|
|
|
|
|
|
|
|
|
l |
|
|
||||||||
_ |
|
I |
|
|
|
|
|
|
GSDIV |
|
Phosphory ase |
|
|
|
||||||
|
|
|
|
|
|
|
|
Liver |
|
GSDVI |
|
|
|
|||||||
GlycogenI |
|
|
|
UridineGlycogen synthetase |
|
|
|
|
|
|||||||||||
|
|
: a-1, 4-glucosidase |
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
-4, |
GSD11 |
|
diphosphoglucose |
|
|
|
|
|
|
|
|
|
|
|
|
|||
GlucoseI |
|
|
|
|
) |
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
Pyrophosph |
Glucose -1-phosphate |
|
|
|
|
|
|
|
|
|
|||||
|
|
I |
|
|
|
|
a,v |
UTP |
|
|
|
|
Limit dextrins |
|
|
|||||
|
|
I |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
I |
|
|
|
|
|
|
|
I Phosphoglucomutase |
|
|
|
|
Debranching |
|
||||
|
|
.. |
|
|
|
|
|
|
|
|
|
|
|
1 enzyme |
[GSDIll |
|||||
|
|
|
|
|
Glucose |
hos ha ase |
|
|
|
Glucokinase |
|
|
|
|
|
|
||||
|
l |
|
|
____ |
|
-6 -_P_ p |
t |
|
Glucose-6-phosphate |
|
|
|
Glucose |
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||
G ucose |
|
|
GSDI |
|
|
|
I Phosphoglucoisomerase |
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
Fructose-6-phosphate |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
I Phosphofructokinase GSDVII |
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
Fructose-1r-phosphate |
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
Pyruvate------. Lactate |
|
|
|
|
|
||||
Fig. 23.8: Glycogen storage disorders Schematic glucose and glycogen metabolism in the liver and lysosome |
Fig. 23.9:Achildwithglycogen |
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
storage disease type I. Note |
the doll like facies and protu berant abdomen)
Figs 23.10A to D: A child with Pompe disease showing (A to C) signs of marked hypotonia and (D) cardiomegaly
ii.Cardiomyopathy (hypertrophic more common than dilated) andconductiondefectsincludingarrhythmias causing sudden early death.
iii.Myopathy
Diagnosis
This is usually made by performing organic acid analysis on urine and plasma acylcarnitine prole, which is later confirmed by enzyme assay, or mutation analysis.
Treatment
Acute decompensation is managed as mentioned in the above section. Prolonged fasting should be avoided. Medium chain triglyceride (MCT) rich formula can be given in VLCAD, LCHAD and CPT I and II deficiency, but not in MCAD and MAD deficiency.
Mitochondrial Disorders
Mitochondriaaremainlyinvolvedin theenergyproduction
pathway of oxidative phosphorylation (OXPHOS).

Mitochondrial disorders refer to defects in the OXPHOS pathway. Mitochondria are mainly derived from the ovum;hence,mitochondrial DNA (mtDNA)disorders are maternally inherited. Tissues such as brain, liver and kidneyhavehigh-energyrequirements andaresusceptible to injury.
Mitochondrial disorders can occur due to either alterations in mitochondrial DNA (mtDNA) or nuclear DNA (nDNA) mutations. The mutant mtDNA produce less energy; symptoms are apparent when energy production is less than energy requirements. Disorders that are due to nDNA mutations are autosomal recessive, autosomal dominant or X-linked. A mitochondrial disorderisoften suspected withmultisystem involvement such as stroke, hearing loss, muscle weakness, cardio myopathy and/or endocrine dysfunction. The disorders due to mtDNA deletion/duplication mutations are chronic progressive external ophthalmoplegia, Kearns Sayresyndrome, Pearson syndrome. Disorders caused by mtDNA point mutations include (Leber hereditary optic neuropathy LHON), (maternally inherited Leigh syn drome MILS), (mitochondrial encephalopathy, lactic acidosis and stroke MELAS), (myoclonic epilepsy with ragged red fibres MERRF ), (neurogenic weakness, ataxia and retinitis pigmentosa NARP), hypertrophic cardio myopathy, mitochondrial myopathy and (nonsyndromic aminoglycoside-induced sensory neural hearing loss SNHL).
Diagnosis
A markedly elevated lactate level raises the possibility of amitochondrialdisorder. An elevated lactate-to-pyruvate ratio of greater than 30 suggests an OXPHOS defect. CSF lactate and pyruvate values also are helpful in some patients. The definite method is muscle biopsy where presence of ragged red bers as well as subsarcolernrnal accumulation of mitochondria confirms mitochondro pathy.Stainingforsuccinatedehydrogenaseandcytochrome C oxidase is useful.
Inborn Errors of Metabolism -
Treatment
No specific therapy is available. Supportive treatment includes symptomatic therapy, supplementation with cofactors such as riboflavin, Co-Q, folinic acid, vitamin E, vitaminC, carnitine,highlipid, lowcarbohydratediet and avoiding mitochondrial toxins such as sodium valproate and statins.
Lysosomal Storage Disorders
Lysosomes are one of the important cellular organelles responsible fordegradationofcomplexcellularmolecules using various acid hydrolases. Deficiency of these enzymes results in the accumulation or storage of an intermediatecompound. Depositionof this storedmaterial in several body tissues leads to cellular damage and disease symptoms. Common categories of lysosomal storage disorders are discussed below.
Enzyme deficiencies in the degradation pathway of glycosaminoglycans cause mucopolysaccharidoses. In some glycolipid storage disorders, neurological functions are impaired due to abnormal deposition in the brain. The second category of oligosaccharidoses is the result of defici encies of enzymes responsible for degradation of glyco proteins with a less complex polysaccharide (oligo saccharides)thanglycosarninoglycans.The thirdcategory, sphingolipidoses is caused by deficiency of sphingolipid degradingenzymes. Accumulationoflipidinsidethecells gives them a foamy appearance. Foamy cells appear in liver, spleen, lungs and marrow, resulting in enlargement of these organs. All conditions have autosomal recessive inheritance except mucopolysaccharidosis II and Fabry disease which are (X-linked). Common disorders are discussed below and summarized in Table 23.7.
Mucopolysaccharidoses
Mucopolysaccharides constitute a majorpart of connective tissue and consist of units of disaccharides, nitrogen and esters. In mucopolysaccharidoses, acid mucopoly-
|
Table 23.7: Clinical features of common lysosomal storage disorders |
|
|||
Disorder |
Cherry-red spot |
Visceromegaly |
Skeletal changes |
Mental retardation |
Bu/bar signs |
Gangliosidosis GMl |
+ |
+ |
+ (Variable) |
+ |
|
Gaucher disease |
|
+ |
+ |
+ |
+ (in types II, III) |
Krabbe disease |
|
|
|
+ |
|
Metachromatic |
Rare |
|
|
+ |
|
leukodystrophy |
|
|
|
|
|
Multiple sulfatase |
+ |
+ |
+ |
+ |
|
deficiency |
|
|
|
|
|
Niemann-Pick |
+ |
+ |
|
+ (Type A, C) |
|
disease |
|
|
|
|
|
Sandhoff disease |
+ |
+ |
+ (Variable) |
+ |
+ (in late stages of |
|
|
|
|
|
infantile forms) |
Tay-Sachs disease |
+ |
|
|
+ |
+ (in late stages of |
|
|
|
|
|
infantile forms) |

__e_ss_ _e_n_t _ia_i_P_e_d_ i_at_r_ic_s_________________________________
saccharides are deposited in thetissuesand excretedin the urine. Due to lack of degradation, mucopolysaccharides accumulate in the lysosomes causing disorganization of the cell structure and function. Partially degraded muco polysaccharides are excreted in urine. At least 8 genetic variants of mucopolysaccharidoses are recognized (Table 23.8) with phenotypic differences (Figs 23.llA to H).
LJ
Mental retardation is severe in type III (Sanfilippo) and VII (Sly), moderate in type I (Hurler, IH), mild in type II
(Hunter), rare in type IV (Morquio) and type I (Scheie, IS) and not seen in type VI (Maroteaux Lamy).
Cloudy cornea is observed in types I, IS and VI but it may occur in some cases of type IV, cloudiness of cornea is minimal in type III and is not seen in type II.
Figs 23.11A to H: Mucopolysaccharidoses. (A) Patient with type IH disease showing corneal clouding and coarse facial features; (B) patient with MPS type II without corneal clouding but with facial coarseness; (C) patient with MPS IHS (milder phenotype) demonstrating restriction ofjoint movements; (D) mild facial coarseness in a child with MPS Ill; (E) chest deformity in a patient with MPS IV (Morquio disease); (F) patient with MPS VI (Maroteux-Lamy) with abnormal skull and facial coarseness; (G) beaking of the inferior margins of vertebrae and proximal pointing of metacarpals in MPS type I; CH) central beaking of the lumber vertebrae along with proximally pointed metacarpals and short ulnae in MPS IV

Inborn Errors of Metabolism -
Table 23.8: Clinical features of mucopolysaccharidoses
MPS type |
Mental retardation |
Coarse facies |
Visceromegaly |
Joint contractures Dysostosis multiplex Corneal clouding |
Hurler/IH |
+ |
+ |
+ |
Scheie/IS |
|
+ (Mild) |
|
Hunter/II |
+ |
+ |
+ |
Sanfilippo/III |
+ |
+ (Mild) |
± |
Morquio/IV |
|
+ (Mild) |
|
Maroteaux- |
|
+ |
+ |
Lamy/VI |
|
|
|
Sly/VII |
+ |
+ |
+ |
Skeletal changes are most marked in type IV, marked in type I, II, VI and VII but are mild in typesIII and IS.Skeletal changes observed include thickening of the skull, marked deformity of sella turcica, broad spatula like ribs, beak shaped vertebrae (around Ll vertebra) and proximal tapering of metacarpals; these abnormalities are referred to as dysostosis multiplex. In Morquio disease (type IV) the trunk is short with flattened narrow vertebrae, barrel shaped chest with sternum protruding forwards. Other features include short neck, broad mouth, widely spaced teeth, prominent maxilla and joint laxity.
Facies are coarse in type IH. Lips are thick, tongue is enlarged and teeth are peg-like and separated; nasal bridge is depressed. The features are coarse and often mistaken for cretinism.
Hepatosplenomegaly is present in types I, II, VI and VII and multiple sulfatase deficiency.
Diagnosis Urinaryexcretionof glycosaminoglycans (GAG) by 2D electrophoresis is a useful screening test. Specific enzyme assays and DNA analyses confirm the diagnosis.
i.Accumulation of dermatan sulfate and heparan sulfate in tissues and their urinary excretion occurs in Hurler syndrome (type IH), Scheie syndrome (type IS), Hunter syndrome (type II) and type VII.
ii.Heparan sulfate accumulatesin tissues and is excreted in urine in Sanfilippo disease (all varieties of MPS III).
iii.Keratan sulfate and chondroitin sulfate are excreted in Morquio syndrome (type IV).
iv.Dermatansulfateisexcretedin theurinein Maroteaux Lamy syndrome (type VI).
v.Keratan sulfate likematerial accumulates in tissue and is excreted in urine in type VIII.
Treatment Palliative care andmultidisciplinarymanage ment are important. Enzyme replacement therapyis avail able for type I, II and type VI but the cost is prohibitive. Trials are underway for other types of MPS. Bone marrow transplantation has been found to be effective in MPS I.
0/igosaccharidoses
This group is characterized by developmental delay with orwithoutregression,facialcoarsening,enlargedliver and spleen, and ocular (cherry-red spot, corneal clouding)
+ |
+ |
+ |
+ |
± |
+ |
+ |
+ |
|
|
± |
|
- (Laxity) |
+ |
+ |
+ |
+ |
+ |
+ |
+ |
± |
changes. Oligosaccharidoses include-pyknodysostosis, p, I P mannosidosis, fucosidosis, aspartyl glucosaminuria,
Schindler disease and sialidosis I and II. Urine screening for oligosaccharides provides clue for diagnosis. Radio logical evidence of dysostosis multiplex may be present. Enzyme assay and DNA analysis is confirmatory.
Sphingo/ipidoses
TheseareclinicallyheterogeneousdisordersandincludeGMl and GM2 gangliosidoses, Gaucher disease, Niemann-Pick diseases, Fabry disease, Farber disease, and Krabbe and metachromaticleukodystrophies.Themostconsistentfeature is enlarged liver and spleen, with or without neurological involvement(GaucherdiseaseI andIII,Niemann-Pickdisease A and B, and GMl gangliosidosis). Metachromatic leukodystrophyandKrabbediseasearecharacterizedbywhite matter involvement and demyelination.
Gaucher disease Gaucher disease is the commonest lysosomal storage disease. Inherited in an autosomal recessive manner, there is deficiency of thetissue enzyme glucocerebrosidase that splits glucose from glucosyl ceramide, resulting in accumulation of the latter in cells of the reticuloendothelial system. The cerebroside-laden cells are large and have eccentric nuclei with vacuolated cytoplasm and 'wrinkled tissue paper' appearance (Gaucher cells).
The spleen is markedly enlarged and there are signs of hypersplenism, e.g. leukopenia and thrombocytopenia. The liver is enlarged and the marrow cavity is widened, due to deposits of Gaucher cells. Expansion of the bone is prominent, especially at the lower end of the femur and humerus. It manifests as a spectrum and has two variants: non-neuronopathic (type I) and neuronopathic (type II: acute; type III: chronic form).
Non-neuronopathic (type I) is the commonest form and characterized by absence of neurological symptoms. Signs and symptoms candevelopat any age andinclude anemia, fatigue, poor growth, delayed puberty, easy bleeding and bruising, weak bones, bone and joint pain, fractures and enlarged liver and spleen (Fig. 23.12A). The earlier the onset of first symptoms, the more severe is the disease and rapid progression if left untreated.

|
Essent iaiPed iatrics |
_______________________ |
|
|
__ |
_ _ _ _ _ _ _ _ _ _ _ _ _ _ _ __________ |
|
|
|
||
Neuronopatlzic forms show involvement of the central nervous system. Two types are distinguished by the rate of neurological progression. TypeII (acute neuronopathic) presentsearly in fetal life ashydrops (excess accumulation of fluid in subcutaneous tissue and other cavities) or in early infancy. Infants are normal during first few months of life before showing neurological signs andinvolvement of spleen and liver. They can also have skin involvement. Course is rapidly progressive leading to early death by 2-4 yr. Type III Gaucher disease (chronic neuronopathic, Fig. 23.12B)representsa chronic form with a more indolent course and manifestations in early childhood before the age of 2 yr. Signs and symptoms are the same as in type 1 exceptthat neurological involvementisslowlyprogressive and leads to death by 2nd or 3rd decade. Neurological symptoms include developmental delay, stridor, squint andswallowingdifficulty, opisthotonus,headretroflexion, spasticity and trismus, abnormal eye movements, oculomotor apraxia (trouble in moving eyes to look side to-side, need to turn head to see things on the side), saccadic initiation failure (failure in starting fast eye movements) and optokinetic nystagmus, dementia and ataxia, generalized tonic-clonic seizures and progressive myoclonic epilepsy.
Diagnosis ismade by measuringglucocerebrosidaselevels in leukocytes or skin fibroblasts. Serum chitotriosidase levels areelevated.Volumeassessmentof liver andspleen byMRI orultrasoundisadvised. Neuro-ophthalmological investigations, hearing assessment by brain evoked response audiometry, EEG and neuropsychometry tests are required. DNA analysis is helpful in assessment of phenotype and prenatal diagnosis.
Treatment. This was the first storage disorder for which treatment was available. Options include: enzyme replacement therapy (ERT)andsubstratereductiontherapy.
Figs 23.12A and B: (A) Gaucher Type 1: Note protuberant abdo men due to hepatosplenomegaly; (B) Gaucher Type Ill. Note trismus and ophthalmoplegia
ERT means providing deficient enzyme through IV route to allow breakdown of fat in cerebroside laden cells,so that they function normally and size of spleen and liver is restored, with improved quality of life. While ERT does not have much effect on neurons, it is efficacious first line of therapy for the hematological, visceral and skeletal manifestations. Thedoseof ERTis60IU/kg/every2weeks, but dose is individualized depending upon the clinical status. Substrate reduction therapy (SRT) means reducing the production of fatty material, thereby avoiding cellular accumulation.Miglustatisoraltreatment foradultpatients with type I Gaucher disease with mild to moderate manifestations forwhich enzyme therapy isnotan option. Both forms of treatment are expensive. Splenectomy increases the risk of progressive skeletal and pulmonary disease. Stem cell transplantation is another option.
Metachromatic leukodystrophy Sulfated glyco sphingolipids accumulate in white matter of the central nervous system, peripheral nerves, liver and kidney. The myelin degenerates but neuronal cellsare affected to lesser degree. Granular masses accumulate in the white matter of the brain. Acidified cresyl violet stains them purple with a brown background, resulting in metachromatic staining.
Clinical features. This disorder has infantile and juvenile forms. Early manifestationsincluding disturbancesofgait, incoordination and progressive mental deterioration appear in the second year of life. Knee jerk is brisk but ankle reflex and plantar response may be absent because of involvement of peripheral nerves. Death occurs before the age of 10 yr. Diagnosis is confirmed by level of the enzyme, arylsulphatase A in white cells.
Treatment. There is no effective treatment; bone marrow transplantation has been used.
GM1 gang/iosidosis In type I, the onset is at birth. There is severe cerebral degeneration. Facial features resemble mucopolysaccharidosis type IH. Hepatosplenomegaly andcherry red spot on themacularregion are present. X ray of the bones show mild dysostosis. These children die of respiratory infections before the age of 2 yr. In type II, the onset of illness is between 1 and 2 yr and death occurs before the age of 10 yr. Liver and spleen are not enlarged. Radiological abnormalities are minimal but psychiatric and motor disturbances are severe.
GM2 gang/iosidosis Inborn errors of GM2 ganglioside metabolism result in accumulation of the metabolite within lysosomes of nerve cells. Most infants with Tay Sachs form (type I) of the disease have severe deficiency of -N-acetylhexosaminidase A (hexosaminidase A). Hexosaminidase A and B are deficient in
(type II).
Tay-Sachs disease is an autosomal recessively inherited defect, common in Ashkenazi Jews, but reported from all

over theworldincluding India. A history ofconsanguinity isobtained.Deficiencyofhexosaminidase leadstoaccumu lation of ganglioside GM2 within ganglion cells of the nervoussystem; myelin isdegenerated.Thedisorder mani fests by 6 months. Apathy, hypotonia, visual defects and developmental retardation occur early. The child pro gressively becomes spastic, blind and demented. Fundus showscherry-redspotoverthemacularregion.Deathoccurs within 3-4 yr. In Sandhoff disease, visceral involvementis present in addition to features of Tay-Sachs disease.
Niemann-Pick disease This is an autosomal recessive disorder of sphingomyelin and cholesterol in the lysosomes. In the classical form (type A), clinical features begin in early life withfeeding difficulties,failure to thrive and developmental delay and later neuroregression. There is protuberant abdomen with hepatosplenomegaly. Cherry-red spot on fundus examination is seen in about half the cases. Diagnosis is confirmed by measurement of sphingomyelinase levels. Type B disease is a milder form with hepatosplenomegaly but no neurological involve ment. Late onset variants (type C) are associated with extrapyramidal manifestations. There is no specific treatment. Table 23.7 summarizes the clinical features of common sphingolipidosis.
Neuronal ceroid /ipofuscinosis (NCL) These are one of
the most frequent and progressive neurodegenerative disorders of childhood. It is characterized by progressive psychomotor retardation, seizures, visual loss and early death. Depending upon the age of onset and severity, it can be divided into infantile, late infantile, juvenile and adult NCL. Confirmation is done by enzyme assay and mutation analysis. No specific therapy is available at present. Antiepileptic such as lamotrigine and leveti racetam are preferred.
Peroxisomal Disorders
Peroxisomes are involved in the oxidation (P-oxidation of phytanic acid and p oxidation of very long-chain fatty acids, VLCFAs) as well as synthesis of plasmalogens. Based upon their functioning, peroxisomal disorders can be divided into two major groups.
Disorders of peroxisomalbiogenesis or importationare
caused by defects in the transfer of proteins produced in the cytosol into the peroxisomes. This includes Zellweger syndrome, neonatal adrenoleukodystrophy and infantile Refsum disease and rhizomelic chondrodysplasia punc tata. These disorders have autosomal recessive inheritance and are caused by defects in genes coding for peroxins (PEX). Defects in these genes interfere with peroxisomal biogenesis and import of proteins into peroxisome. Approximately 65% of the patients harbor mutations in PEXl gene.
Zellweger syndrome (Fig. 23.13), also known as cerebro hepatorenal syndrome is characterized by dysmorphic
Inborn Errors of Metabolism -
facies (high forehead, large anterior fontanelle, at occiput, |
|
|
hypoplastic supraorbital ridges, broad nasal bridge, |
|
|
epicanthal folds, anteverted nostrils, micrognathia), |
|
|
central nervous system defects (neuronal migration defect, |
|
|
dysmyelination, seizures), hepatic dysfunction and |
|
|
cirrhosis, adrenal insufficiency and renal microcysts. |
|
|
Prognosis is poor and patients usually die in infancy. |
I |
|
Diagnosis is suggested by high plasma levels of very long |
||
|
||
chain fatty acids (VLCFA) and phytanic acid, and low |
|
|
erythrocyte plasmalogen levels. |
|
Fig. 23.13: An infant with Zellweger syndrome. Note flat facial profile
Rhizomelic chondrodysplasia punctata is characterized by altered phytanic acid a-oxidation and plasmalogen synthesis. Type 1 is a peroxisomal biogenesis defect, while types 2 and 3 are disorders of individual peroxisomal enzymes.Patientsshow rhizomelia and joint contractures along with extensive epiphyseal stippling of long bones (Figs 23.14A and B). They have congenital cataract, developmental delay and growth failure. In contrast to Zellweger syndrome, patients with this disorder have normal VLCFA concentrations and low red blood cell plasmalogens. Phytanic acid concentrations are either elevated (in type 1) or normal (type 2 or 3).
Figs 23.14A and B: (A) Child with rhizomelic chondrodysplasia punctata; CB) epiphyseal stippling

Essent iaiPed iatrics |
______________________ |
|
__ |
_ _ _ _ _ _ _ _ _ _ _ _ _ _ _ ___________ |
|
|
|
|
Fig. 23.15: Brain MRI findings in X-linked adrenoleukodystrophy. T2 weighted axial images show symmetrical hyperintense signal changes in the bilateral parieto-occipital white matter and splenium of corpus callosum (Courtesy: Dr. Atin Kumar, Deptt. of Radiodiagnosis, AIIMS, New Delhi)
Disorders of individual peroxisomal enzymes include
X-linked adrenoleukodystrophy and classical Refsum disease.
X-linked adrenoleukodystrophy (ALO) is an X-linked recessive disorder caused by tissue accumulation of VLCFA with a carbon chain length of 24 or more due to
deficient peroxisomal degradation of fatty acids. The defective gene (ABCDl gene) is located on Xq28. The three
neurological forms are:
The childhood cerebralform usually manifests between 4 and 8 yr of age with subtle initial manifestations of worsening school performance and behavioral problems such as hyperactivity and emotional !ability. Auditory and visual disturbances may be associated. Seizures are often the initial manifestation. In most patients, adrenal dysfunction is noticed after the cerebral symptoms. Soon rapid neurological progression ensues causing increasing spasticity, visual and hearing impairment. Progression is due to an inflammatory response, which is most intense in the parieto-occipital areas. MRI brain typically shows demyelination in these areas (Fig. 23.15). In adolescents, the usual age of manifestation is between 10 and 21 yr and progression is much slower than the above form. Adrenomyeloneuropathy is a milder form with onset in late
adolescence or adulthood and is characterized by progressive paraparesis due to long tract degeneration in the spinal cord.
Elevated plasma levels of VLCFA can identify patients and 85% of female carriers of X-adrenoleukodystrophy. Mutation analysis is the most reliable method to identify carriers. Corticosteroid replacement should be given for adrenal insufficiency. Bone marrow transplantation can be considered in neurologically asymptomatic or mildly involved patients. Lorenzo oil is recommended in neurologically asymptomatic and boys who are less than 8-yr-old with normal MRI.
Suggested Reading
Burton BK. Inborn errors of metabolism in infancy: A guide to diagnosis. Pediatrics 1998;102:£69
Clarke JTR. General principles. In: A clinical guide to inherited metabolic diseases, 3rdedn. NewYork: CambridgeUniversityPress, 2006 Lyon G, Kolodny EH, Pastores GM. Neurology of Hereditary Metabolic Diseases of Children, 3rd edn New York. McGraw Hill, 2006 Saudubray JM, Chappentier C. Clinical phenotypes: diagnosis/ algorithms. In: Scriver CR, Beaudet AL, Sly WS, et al. eds. Metabolic and molecularbases ofinheriteddisease, 8th edn. New York: McGraw
Hill, 2001;pp 1327-403
Saudubray JM, van den Berghe G, Walter JH. Inborn metabolic diseases: Diagnosis and treatment, 5th edn. Springer Medizin; 2011
