
- •Preface
- •Acknowledgments
- •Contents
- •1.1 Introduction
- •1.2 Normal Embryology
- •1.3 Abnormalities of the Kidney
- •1.3.1 Renal Agenesis
- •1.3.2 Renal Hypoplasia
- •1.3.3 Supernumerary Kidneys
- •1.3.5 Polycystic Kidney Disease
- •1.3.6 Simple (Solitary) Renal Cyst
- •1.3.7 Renal Fusion and Renal Ectopia
- •1.3.8 Horseshoe Kidney
- •1.3.9 Crossed Fused Renal Ectopia
- •1.4 Abnormalities of the Ureter
- •1.5 Abnormalities of the Bladder
- •1.6 Abnormalities of the Penis and Urethra in Males
- •1.7 Abnormalities of Female External Genitalia
- •Further Reading
- •2.1 Introduction
- •2.2 Pathophysiology
- •2.3 Etiology of Hydronephrosis
- •2.5 Clinical Features
- •2.6 Investigations and Diagnosis
- •2.7 Treatment
- •2.8 Antenatal Hydronephrosis
- •Further Reading
- •3.1 Introduction
- •3.2 Embryology
- •3.3 Pathophysiology
- •3.4 Etiology of PUJ Obstruction
- •3.5 Clinical Features
- •3.6 Diagnosis and Investigations
- •3.7 Management of Newborns with PUJ Obstruction
- •3.8 Treatment
- •3.9 Post-operative Complications and Follow-Up
- •Further Reading
- •4: Renal Tumors in Children
- •4.1 Introduction
- •4.2 Wilms’ Tumor
- •4.2.1 Introduction
- •4.2.2 Etiology
- •4.2.3 Histopathology
- •4.2.4 Nephroblastomatosis
- •4.2.5 Clinical Features
- •4.2.6 Risk Factors for Wilms’ Tumor
- •4.2.7 Staging of Wilms Tumor
- •4.2.8 Investigations
- •4.2.9 Prognosis and Complications of Wilms Tumor
- •4.2.10 Surgical Considerations
- •4.2.11 Surgical Complications
- •4.2.12 Prognosis and Outcome
- •4.2.13 Extrarenal Wilms’ Tumors
- •4.3 Mesoblastic Nephroma
- •4.3.1 Introduction
- •4.3.3 Epidemiology
- •4.3.5 Clinical Features
- •4.3.6 Investigations
- •4.3.7 Treatment and Prognosis
- •4.4 Clear Cell Sarcoma of the Kidney (CCSK)
- •4.4.1 Introduction
- •4.4.2 Pathophysiology
- •4.4.3 Clinical Features
- •4.4.4 Investigations
- •4.4.5 Histopathology
- •4.4.6 Treatment
- •4.4.7 Prognosis
- •4.5 Malignant Rhabdoid Tumor of the Kidney
- •4.5.1 Introduction
- •4.5.2 Etiology and Pathophysiology
- •4.5.3 Histologic Findings
- •4.5.4 Clinical Features
- •4.5.5 Investigations and Diagnosis
- •4.5.6 Treatment and Outcome
- •4.5.7 Mortality/Morbidity
- •4.6 Renal Cell Carcinoma in Children
- •4.6.1 Introduction
- •4.6.2 Histopathology
- •4.6.4 Staging
- •4.6.5 Clinical Features
- •4.6.6 Investigations
- •4.6.7 Management
- •4.6.8 Prognosis
- •4.7 Angiomyolipoma of the Kidney
- •4.7.1 Introduction
- •4.7.2 Histopathology
- •4.7.4 Clinical Features
- •4.7.5 Investigations
- •4.7.6 Treatment and Prognosis
- •4.8 Renal Lymphoma
- •4.8.1 Introduction
- •4.8.2 Etiology and Pathogenesis
- •4.8.3 Diagnosis
- •4.8.4 Clinical Features
- •4.8.5 Treatment and Prognosis
- •4.9 Ossifying Renal Tumor of Infancy
- •4.10 Metanephric Adenoma
- •4.10.1 Introduction
- •4.10.2 Histopathology
- •4.10.3 Diagnosis
- •4.10.4 Clinical Features
- •4.10.5 Treatment
- •4.11 Multilocular Cystic Renal Tumor
- •Further Reading
- •Wilms’ Tumor
- •Mesoblastic Nephroma
- •Renal Cell Carcinoma in Children
- •Angiomyolipoma of the Kidney
- •Renal Lymphoma
- •Ossifying Renal Tumor of Infancy
- •Metanephric Adenoma
- •Multilocular Cystic Renal Tumor
- •5.1 Introduction
- •5.2 Embryology
- •5.4 Histologic Findings
- •5.7 Associated Anomalies
- •5.8 Clinical Features
- •5.9 Investigations
- •5.10 Treatment
- •Further Reading
- •6: Congenital Ureteral Anomalies
- •6.1 Etiology
- •6.2 Clinical Features
- •6.3 Investigations and Diagnosis
- •6.4 Duplex (Duplicated) System
- •6.4.1 Introduction
- •6.4.3 Clinical Features
- •6.4.4 Investigations
- •6.4.5 Treatment and Prognosis
- •6.5 Ectopic Ureter
- •6.5.1 Introduction
- •6.5.3 Clinical Features
- •6.5.4 Diagnosis
- •6.5.5 Surgical Treatment
- •6.6 Ureterocele
- •6.6.1 Introduction
- •6.6.3 Clinical Features
- •6.6.4 Investigations and Diagnosis
- •6.6.5 Treatment
- •6.6.5.1 Surgical Interventions
- •6.8 Mega Ureter
- •Further Reading
- •7: Congenital Megaureter
- •7.1 Introduction
- •7.3 Etiology and Pathophysiology
- •7.4 Clinical Presentation
- •7.5 Investigations and Diagnosis
- •7.6 Treatment and Prognosis
- •7.7 Complications
- •Further Reading
- •8.1 Introduction
- •8.2 Pathophysiology
- •8.4 Etiology of VUR
- •8.5 Clinical Features
- •8.6 Investigations
- •8.7 Management
- •8.7.1 Medical Treatment of VUR
- •8.7.2 Antibiotics Used for Prophylaxis
- •8.7.3 Anticholinergics
- •8.7.4 Surveillance
- •8.8 Surgical Therapy of VUR
- •8.8.1 Indications for Surgical Interventions
- •8.8.2 Indications for Surgical Interventions Based on Age at Diagnosis and the Presence or Absence of Renal Lesions
- •8.8.3 Endoscopic Injection
- •8.8.4 Surgical Management
- •8.9 Mortality/Morbidity
- •Further Reading
- •9: Pediatric Urolithiasis
- •9.1 Introduction
- •9.2 Etiology
- •9.4 Clinical Features
- •9.5 Investigations
- •9.6 Complications of Urolithiasis
- •9.7 Management
- •Further Reading
- •10.1 Introduction
- •10.2 Embryology of Persistent Müllerian Duct Syndrome
- •10.3 Etiology and Inheritance of PMDS
- •10.5 Clinical Features
- •10.6 Treatment
- •10.7 Prognosis
- •Further Reading
- •11.1 Introduction
- •11.2 Physiology and Bladder Function
- •11.2.1 Micturition
- •11.3 Pathophysiological Changes of NBSD
- •11.4 Etiology and Clinical Features
- •11.5 Investigations and Diagnosis
- •11.7 Management
- •11.8 Clean Intermittent Catheterization
- •11.9 Anticholinergics
- •11.10 Botulinum Toxin Type A
- •11.11 Tricyclic Antidepressant Drugs
- •11.12 Surgical Management
- •Further Reading
- •12.1 Introduction
- •12.2 Etiology
- •12.3 Pathophysiology
- •12.4 Clinical Features
- •12.5 Investigations and Diagnosis
- •12.6 Management
- •Further Reading
- •13.1 Introduction
- •13.2 Embryology
- •13.3 Epispadias
- •13.3.1 Introduction
- •13.3.2 Etiology
- •13.3.4 Treatment
- •13.3.6 Female Epispadias
- •13.3.7 Surgical Repair of Female Epispadias
- •13.3.8 Prognosis
- •13.4 Bladder Exstrophy
- •13.4.1 Introduction
- •13.4.2 Associated Anomalies
- •13.4.3 Principles of Surgical Management of Bladder Exstrophy
- •13.4.4 Evaluation and Management
- •13.5 Cloacal Exstrophy
- •13.5.1 Introduction
- •13.5.2 Skeletal Changes in Cloacal Exstrophy
- •13.5.3 Etiology and Pathogenesis
- •13.5.4 Prenatal Diagnosis
- •13.5.5 Associated Anomalies
- •13.5.8 Surgical Reconstruction
- •13.5.9 Management of Urinary Incontinence
- •13.5.10 Prognosis
- •13.5.11 Complications
- •Further Reading
- •14.1 Introduction
- •14.2 Etiology
- •14.3 Clinical Features
- •14.4 Associated Anomalies
- •14.5 Diagnosis
- •14.6 Treatment and Prognosis
- •Further Reading
- •15: Cloacal Anomalies
- •15.1 Introduction
- •15.2 Associated Anomalies
- •15.4 Clinical Features
- •15.5 Investigations
- •Further Reading
- •16: Urachal Remnants
- •16.1 Introduction
- •16.2 Embryology
- •16.4 Clinical Features
- •16.5 Tumors and Urachal Remnants
- •16.6 Management
- •Further Reading
- •17: Inguinal Hernias and Hydroceles
- •17.1 Introduction
- •17.2 Inguinal Hernia
- •17.2.1 Incidence
- •17.2.2 Etiology
- •17.2.3 Clinical Features
- •17.2.4 Variants of Hernia
- •17.2.6 Treatment
- •17.2.7 Complications of Inguinal Herniotomy
- •17.3 Hydrocele
- •17.3.1 Embryology
- •17.3.3 Treatment
- •Further Reading
- •18: Cloacal Exstrophy
- •18.1 Introduction
- •18.2 Etiology and Pathogenesis
- •18.3 Associated Anomalies
- •18.4 Clinical Features and Management
- •Further Reading
- •19: Posterior Urethral Valve
- •19.1 Introduction
- •19.2 Embryology
- •19.3 Pathophysiology
- •19.5 Clinical Features
- •19.6 Investigations and Diagnosis
- •19.7 Management
- •19.8 Medications Used in Patients with PUV
- •19.10 Long-Term Outcomes
- •19.10.3 Bladder Dysfunction
- •19.10.4 Renal Transplantation
- •19.10.5 Fertility
- •Further Reading
- •20.1 Introduction
- •20.2 Embryology
- •20.4 Clinical Features
- •20.5 Investigations
- •20.6 Treatment
- •20.7 The Müllerian Duct Cyst
- •Further Reading
- •21: Hypospadias
- •21.1 Introduction
- •21.2 Effects of Hypospadias
- •21.3 Embryology
- •21.4 Etiology of Hypospadias
- •21.5 Associated Anomalies
- •21.7 Clinical Features of Hypospadias
- •21.8 Treatment
- •21.9 Urinary Diversion
- •21.10 Postoperative Complications
- •Further Reading
- •22: Male Circumcision
- •22.1 Introduction
- •22.2 Anatomy and Pathophysiology
- •22.3 History of Circumcision
- •22.4 Pain Management
- •22.5 Indications for Circumcision
- •22.6 Contraindications to Circumcision
- •22.7 Surgical Procedure
- •22.8 Complications of Circumcision
- •Further Reading
- •23: Priapism in Children
- •23.1 Introduction
- •23.2 Pathophysiology
- •23.3 Etiology
- •23.5 Clinical Features
- •23.6 Investigations
- •23.7 Management
- •23.8 Prognosis
- •23.9 Priapism and Sickle Cell Disease
- •23.9.1 Introduction
- •23.9.2 Epidemiology
- •23.9.4 Pathophysiology
- •23.9.5 Clinical Features
- •23.9.6 Treatment
- •23.9.7 Prevention of Stuttering Priapism
- •23.9.8 Complications of Priapism and Prognosis
- •Further Reading
- •24.1 Introduction
- •24.2 Embryology and Normal Testicular Development and Descent
- •24.4 Causes of Undescended Testes and Risk Factors
- •24.5 Histopathology
- •24.7 Clinical Features and Diagnosis
- •24.8 Treatment
- •24.8.1 Success of Surgical Treatment
- •24.9 Complications of Orchidopexy
- •24.10 Infertility and Undescended Testes
- •24.11 Undescended Testes and the Risk of Cancer
- •Further Reading
- •25: Varicocele
- •25.1 Introduction
- •25.2 Etiology
- •25.3 Pathophysiology
- •25.4 Grading of Varicoceles
- •25.5 Clinical Features
- •25.6 Diagnosis
- •25.7 Treatment
- •25.8 Postoperative Complications
- •25.9 Prognosis
- •Further Reading
- •26.1 Introduction
- •26.2 Etiology and Risk Factors
- •26.3 Diagnosis
- •26.4 Intermittent Testicular Torsion
- •26.6 Effects of Testicular Torsion
- •26.7 Clinical Features
- •26.8 Treatment
- •26.9.1 Introduction
- •26.9.2 Etiology of Extravaginal Torsion
- •26.9.3 Clinical Features
- •26.9.4 Treatment
- •26.10 Torsion of the Testicular or Epididymal Appendage
- •26.10.1 Introduction
- •26.10.2 Embryology
- •26.10.3 Clinical Features
- •26.10.4 Investigations and Treatment
- •Further Reading
- •27: Testicular Tumors in Children
- •27.1 Introduction
- •27.4 Etiology of Testicular Tumors
- •27.5 Clinical Features
- •27.6 Staging
- •27.6.1 Regional Lymph Node Staging
- •27.7 Investigations
- •27.8 Treatment
- •27.9 Yolk Sac Tumor
- •27.10 Teratoma
- •27.11 Mixed Germ Cell Tumor
- •27.12 Stromal Tumors
- •27.13 Simple Testicular Cyst
- •27.14 Epidermoid Cysts
- •27.15 Testicular Microlithiasis (TM)
- •27.16 Gonadoblastoma
- •27.17 Cystic Dysplasia of the Testes
- •27.18 Leukemia and Lymphoma
- •27.19 Paratesticular Rhabdomyosarcoma
- •27.20 Prognosis and Outcome
- •Further Reading
- •28: Splenogonadal Fusion
- •28.1 Introduction
- •28.2 Etiology
- •28.4 Associated Anomalies
- •28.5 Clinical Features
- •28.6 Investigations
- •28.7 Treatment
- •Further Reading
- •29: Acute Scrotum
- •29.1 Introduction
- •29.2 Torsion of Testes
- •29.2.1 Introduction
- •29.2.3 Etiology
- •29.2.4 Clinical Features
- •29.2.5 Effects of Torsion of Testes
- •29.2.6 Investigations
- •29.2.7 Treatment
- •29.3 Torsion of the Testicular or Epididymal Appendage
- •29.3.1 Introduction
- •29.3.2 Embryology
- •29.3.3 Clinical Features
- •29.3.4 Investigations and Treatment
- •29.4.1 Introduction
- •29.4.2 Etiology
- •29.4.3 Clinical Features
- •29.4.4 Investigations and Treatment
- •29.5 Idiopathic Scrotal Edema
- •29.6 Testicular Trauma
- •29.7 Other Causes of Acute Scrotum
- •29.8 Splenogonadal Fusion
- •Further Reading
- •30.1 Introduction
- •30.2 Imperforate Hymen
- •30.3 Vaginal Atresia
- •30.5 Associated Anomalies
- •30.6 Embryology
- •30.7 Clinical Features
- •30.8 Investigations
- •30.9 Management
- •Further Reading
- •31: Disorders of Sexual Development
- •31.1 Introduction
- •31.2 Embryology
- •31.3 Sexual and Gonadal Differentiation
- •31.5 Evaluation of a Newborn with DSD
- •31.6 Diagnosis and Investigations
- •31.7 Management of Patients with DSD
- •31.8 Surgical Corrections of DSD
- •31.9 Congenital Adrenal Hyperplasia (CAH)
- •31.10 Androgen Insensitivity Syndrome (Testicular Feminization Syndrome)
- •31.13 Gonadal Dysgenesis
- •31.15 Ovotestis Disorders of Sexual Development
- •31.16 Other Rare Disorders of Sexual Development
- •Further Reading
- •Index
576 |
27 Testicular Tumors in Children |
|
|
•Teratomas are the most common benign tumors in children.
•Recent reports found that teratomas were more common than endodermal sinus tumors in children.
•The gonadal stromal tumors are usually benign, there has been the very rare case of malignant gonadal stromal tumor.
•Juvenile granulosa cell tumors are the most common tumors among neonatal tumors. These tumors are benign.
27.3Histologic Classification of Seminomas
Classification of Testicular Tumors
•Germ Cell Tumors
–Seminomas
–Teratomas
–Embryonal carcinoma
–Choriocarcinomas
–Yolk sac tumors (Endodermal sınus tumor)
–Mixed germ cell tumors.
•Gonadal Stromal Tumors
–Leyding cell
–Sertoli cell
–Juvenile granuloza gell
•Mixed form
•Gonadoblastoma
•Tumors of Supporting Tissues
–Fibroma
–Leimiyoma
–Hemangioma
•Lymphomas and Leukemias
•Tumor like Lesions
•Epidermoid cysts
•Hyperplastic nodule secondary to congenital adrenal hyperplasia
•Secondary Tumors
•Grossly, seminomas are pale gray–to-yellow nodules that are uniform or slightly lobulated.
•Pure seminomas are subdivided into three subtypes based on histopathologic characteristics:
Histologic Classification of Seminomas
•Classic seminomas (85 %)
•Anaplastic seminoma (10 %)
•Spermatocytic seminoma (5 %)
•Classic seminomas (85 %):
–They demonstrate a monotonous sheet of large cells with abundant cytoplasm and round hyperchromatic nuclei with prominent nucleoli.
–A lymphocytic infiltrate or granulomatous reaction with giant cells or both is frequently present.
–Trophoblastic giant cells capable of producing hCG are present in 15–20 % of tumors.
–Mitoses are infrequent.
•Anaplastic seminoma (10 %):
–This is an older term used to describe seminomas with three or more mitotic figures per high-power field.
–This finding has no clinical or prognostic significance because the response of anaplastic seminomas to standard therapy is equivalent to that of classic seminomas.
•Spermatocytic seminoma (5 %):
–This is a rare histologic variant that is not associated with carcinoma in situ.
–These well-differentiated tumors usually contain cells resembling secondary spermatids or spermatocytes.
–Spermatocytic seminomas rarely metastasize, and they occur almost exclusively in elderly men.
–The only recommended treatment is orchiectomy.
27.4Etiology of Testicular Tumors
•The exact etiology of testicular cancer is not clearly known.
•There is a dramatic increase in the incidence rate of testicular cancer in developed countries and the reason for this is not known.

27.4 Etiology of Testicular Tumors |
577 |
|
|
•Most testicular tumors occur sporadically, but familial cases have been observed and some cases occur because of a predisposing history.
Risk Factors for Testicular Cancer
•Cryptoorchidism
•Testicular microlithiasis
•Disorders of sexual development
•Familial predisposition
•Other associations:
–Iguinal hernias
–Klinefelter syndrome
–Mumps orchitis
–Hypospadias and hydrocele
–Chromosome 12 abnormalities
–Prior testicular cancer increases the risk on the contralateral testis
–Human immunodeficiency virus (HIV) infection
–History of testicular trauma
–Immunosuppression after organ transplant
–Prior vasectomy
–The use of cannabis and marijuana
–An association with prenatal exposure to diethylstilbestrol (DES) has been postulated but not demonstrated
•A major risk factor for the development of testis cancer is cryptorchidism (undescended testicles).
–The risk of testicular cancer in men with a history of undescended testis has been estimated at 10 to 40-fold greater than the general population.
–More recent studies have found the risk to be fivefold greater than that of the general population.
–The life-time risk for testicular cancer in those with undescended testis is 1–2 %.
–7–10 % of testis tumors occur in association with cryptorchidism.
–25 % of the cancers found in association with cryptorchidism occur in the contralateral, normally descended testis. This
suggests that an inherent developmental defect is responsible for both the undescended testes and the tumor development.
–It has been found that the risk of developing testicular cancer in patients with undescended testes is directly related to the degree of maldescent.
•The risk is 1 in 20 if the testis is intra-abdominal.
•The risk is 1 in 80 if it is within the inguinal canal.
–Whether early orchidopexy can ameliorate that risk is unclear. Currently, it is believed that orchiopexy performed before puberty reduces the risk of germ cell tumors and improves the ability to observe the testis.
–The increased risk of germ cell tumors is reflected in the finding of carcinoma in situ in 2–4 % of men with a history of cryptorchidism.
•Testicular microlithiasis:
–Testicular microlithiasis refers to the presence of microcalcifications, usually diffuse, within the parenchyma of the testis on ultrasound.
–Testicular microlithiasis is defined as ≥5 or more microcalcifications within a testicle.
–Teticular microlithiasis is found incidentally in approximately 2% of boys and men undergoing testicular ultrasound evaluation.
–This has been identified as a possible risk factor for the development of testicular cancer but the reason for this association is not clear.
–The association with testicular malignancies was suggested by the finding that approximately 25 % of adult testes harboring cancer are found to have testicular microlithiasis.
•Disorders of sexual development (Figs. 27.3, 27.4, 27.5, 27.6, 27.7, 27.8, 27.9, and 27.10):
–Disorders of sexual development are a very significant risk for the development of gonadal tumors.
–Some disorders, such as complete androgen insensitivity syndrome, have an increased risk of testicular cancer.

578 |
27 Testicular Tumors in Children |
|
|
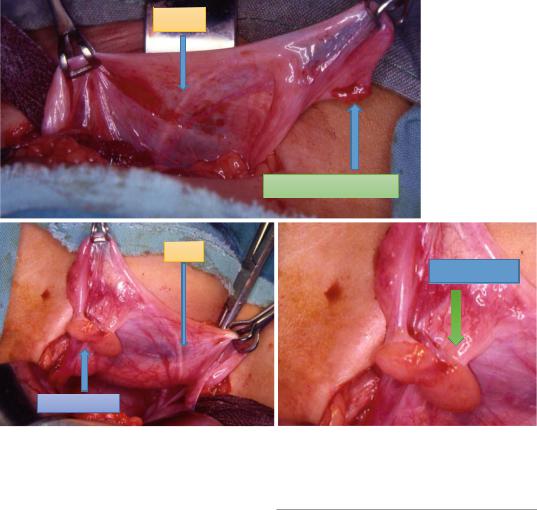
Figs. 27.3, 27.4, 27.5, 27.6, and 27.7 Clinical intraoperative photographs showing patients with testicular feminization syndrome. These are genotypically males with
phenotypic female external genitalia. These patients usually have intraabdominal testes which are at increased risk of malignant transformation and must be removed
–There is an increased risk in those with dysgenetic or streak gonads.
–This risk seems to exist almost exclusively in patients with Y chromatin.
–Patients with pure gonadal dysgenesis and Y chromatin as well as the “streak” gonad of patients with mixed gonadal dysgenesis are at a 15–30 % risk for tumor development.
–The tumors arising in those with gonadal dysgenesis are usually gonadoblastomas.
–While gonadoblastomas are benign, they are prone to the development of malignant degeneration and when malignancies
occur, dysgerminoma is the most common histological type. .
–While most cases of malignancy occur after puberty, there have been case reports in children as well.
–Prophylactic removal of dysgenetic gonads should be undertaken early in life to avoid malignant transformation in these patients.
•Other risk factors include:
–Inguinal hernias
–Klinefelter syndrome
–Mumps orchitis
–Hypospadias and hydrocele
27.5 Clinical Features |
579 |
|
|
VAS
FALLOPIAN TUBE
VAS
OVOTESTES
OVOTESTES
Figs. 27.8, 27.9, and 27.10 Clinical intraoperative photographs of a patient with ovotesticular DSD. Note the presence of an ovotestis on this side. The testis or testicu-
lar part of an ovotestis is likely to be dysgenetic with a risk of developing dysgerminomas, seminomas, gonadoblastomas, and yolk sac carcinomas
–Chromosome 12 abnormalities are seen in nearly all adult malignant germ cell tumors, but are not seen in prepubertal yolk sac tumors.
–Prior testicular cancer is a major risk factor for a contralateral malignancy. The cumulative risk 25 years after original diagnosis is 3.6% for patients with seminoma.
–Human immunodeficiency virus (HIV) infection
–History of testicular trauma
–Immunosuppression after organ transplant
–Prior vasectomy
–The higher rates of testicular cancer in western nations have been linked to use of cannabis. Long term use of cannabis and marijuana is linked to an increased risk for testicular cancer.
27.5Clinical Features
•The incidence of pediatric testicular tumors peaks in children aged 2–4 years.
•Most yolk-sac tumors occur in children younger than 2 years.
•About 85 % of children with testicular tumors present with painless scrotal swelling.
•A few present with a hydrocele, scrotal pain, or a history of trauma, any of which probably alerts the child to the presence of a painless and enlarged testicle.
•10 % may give a history of hernia or hydrocele
•15–50 % have hydrocele on physical exam
•Rarely, they may present with acute abdominal pain
