
- •Preface
- •Acknowledgments
- •Contents
- •1.1 Introduction
- •1.2 Normal Embryology
- •1.3 Abnormalities of the Kidney
- •1.3.1 Renal Agenesis
- •1.3.2 Renal Hypoplasia
- •1.3.3 Supernumerary Kidneys
- •1.3.5 Polycystic Kidney Disease
- •1.3.6 Simple (Solitary) Renal Cyst
- •1.3.7 Renal Fusion and Renal Ectopia
- •1.3.8 Horseshoe Kidney
- •1.3.9 Crossed Fused Renal Ectopia
- •1.4 Abnormalities of the Ureter
- •1.5 Abnormalities of the Bladder
- •1.6 Abnormalities of the Penis and Urethra in Males
- •1.7 Abnormalities of Female External Genitalia
- •Further Reading
- •2.1 Introduction
- •2.2 Pathophysiology
- •2.3 Etiology of Hydronephrosis
- •2.5 Clinical Features
- •2.6 Investigations and Diagnosis
- •2.7 Treatment
- •2.8 Antenatal Hydronephrosis
- •Further Reading
- •3.1 Introduction
- •3.2 Embryology
- •3.3 Pathophysiology
- •3.4 Etiology of PUJ Obstruction
- •3.5 Clinical Features
- •3.6 Diagnosis and Investigations
- •3.7 Management of Newborns with PUJ Obstruction
- •3.8 Treatment
- •3.9 Post-operative Complications and Follow-Up
- •Further Reading
- •4: Renal Tumors in Children
- •4.1 Introduction
- •4.2 Wilms’ Tumor
- •4.2.1 Introduction
- •4.2.2 Etiology
- •4.2.3 Histopathology
- •4.2.4 Nephroblastomatosis
- •4.2.5 Clinical Features
- •4.2.6 Risk Factors for Wilms’ Tumor
- •4.2.7 Staging of Wilms Tumor
- •4.2.8 Investigations
- •4.2.9 Prognosis and Complications of Wilms Tumor
- •4.2.10 Surgical Considerations
- •4.2.11 Surgical Complications
- •4.2.12 Prognosis and Outcome
- •4.2.13 Extrarenal Wilms’ Tumors
- •4.3 Mesoblastic Nephroma
- •4.3.1 Introduction
- •4.3.3 Epidemiology
- •4.3.5 Clinical Features
- •4.3.6 Investigations
- •4.3.7 Treatment and Prognosis
- •4.4 Clear Cell Sarcoma of the Kidney (CCSK)
- •4.4.1 Introduction
- •4.4.2 Pathophysiology
- •4.4.3 Clinical Features
- •4.4.4 Investigations
- •4.4.5 Histopathology
- •4.4.6 Treatment
- •4.4.7 Prognosis
- •4.5 Malignant Rhabdoid Tumor of the Kidney
- •4.5.1 Introduction
- •4.5.2 Etiology and Pathophysiology
- •4.5.3 Histologic Findings
- •4.5.4 Clinical Features
- •4.5.5 Investigations and Diagnosis
- •4.5.6 Treatment and Outcome
- •4.5.7 Mortality/Morbidity
- •4.6 Renal Cell Carcinoma in Children
- •4.6.1 Introduction
- •4.6.2 Histopathology
- •4.6.4 Staging
- •4.6.5 Clinical Features
- •4.6.6 Investigations
- •4.6.7 Management
- •4.6.8 Prognosis
- •4.7 Angiomyolipoma of the Kidney
- •4.7.1 Introduction
- •4.7.2 Histopathology
- •4.7.4 Clinical Features
- •4.7.5 Investigations
- •4.7.6 Treatment and Prognosis
- •4.8 Renal Lymphoma
- •4.8.1 Introduction
- •4.8.2 Etiology and Pathogenesis
- •4.8.3 Diagnosis
- •4.8.4 Clinical Features
- •4.8.5 Treatment and Prognosis
- •4.9 Ossifying Renal Tumor of Infancy
- •4.10 Metanephric Adenoma
- •4.10.1 Introduction
- •4.10.2 Histopathology
- •4.10.3 Diagnosis
- •4.10.4 Clinical Features
- •4.10.5 Treatment
- •4.11 Multilocular Cystic Renal Tumor
- •Further Reading
- •Wilms’ Tumor
- •Mesoblastic Nephroma
- •Renal Cell Carcinoma in Children
- •Angiomyolipoma of the Kidney
- •Renal Lymphoma
- •Ossifying Renal Tumor of Infancy
- •Metanephric Adenoma
- •Multilocular Cystic Renal Tumor
- •5.1 Introduction
- •5.2 Embryology
- •5.4 Histologic Findings
- •5.7 Associated Anomalies
- •5.8 Clinical Features
- •5.9 Investigations
- •5.10 Treatment
- •Further Reading
- •6: Congenital Ureteral Anomalies
- •6.1 Etiology
- •6.2 Clinical Features
- •6.3 Investigations and Diagnosis
- •6.4 Duplex (Duplicated) System
- •6.4.1 Introduction
- •6.4.3 Clinical Features
- •6.4.4 Investigations
- •6.4.5 Treatment and Prognosis
- •6.5 Ectopic Ureter
- •6.5.1 Introduction
- •6.5.3 Clinical Features
- •6.5.4 Diagnosis
- •6.5.5 Surgical Treatment
- •6.6 Ureterocele
- •6.6.1 Introduction
- •6.6.3 Clinical Features
- •6.6.4 Investigations and Diagnosis
- •6.6.5 Treatment
- •6.6.5.1 Surgical Interventions
- •6.8 Mega Ureter
- •Further Reading
- •7: Congenital Megaureter
- •7.1 Introduction
- •7.3 Etiology and Pathophysiology
- •7.4 Clinical Presentation
- •7.5 Investigations and Diagnosis
- •7.6 Treatment and Prognosis
- •7.7 Complications
- •Further Reading
- •8.1 Introduction
- •8.2 Pathophysiology
- •8.4 Etiology of VUR
- •8.5 Clinical Features
- •8.6 Investigations
- •8.7 Management
- •8.7.1 Medical Treatment of VUR
- •8.7.2 Antibiotics Used for Prophylaxis
- •8.7.3 Anticholinergics
- •8.7.4 Surveillance
- •8.8 Surgical Therapy of VUR
- •8.8.1 Indications for Surgical Interventions
- •8.8.2 Indications for Surgical Interventions Based on Age at Diagnosis and the Presence or Absence of Renal Lesions
- •8.8.3 Endoscopic Injection
- •8.8.4 Surgical Management
- •8.9 Mortality/Morbidity
- •Further Reading
- •9: Pediatric Urolithiasis
- •9.1 Introduction
- •9.2 Etiology
- •9.4 Clinical Features
- •9.5 Investigations
- •9.6 Complications of Urolithiasis
- •9.7 Management
- •Further Reading
- •10.1 Introduction
- •10.2 Embryology of Persistent Müllerian Duct Syndrome
- •10.3 Etiology and Inheritance of PMDS
- •10.5 Clinical Features
- •10.6 Treatment
- •10.7 Prognosis
- •Further Reading
- •11.1 Introduction
- •11.2 Physiology and Bladder Function
- •11.2.1 Micturition
- •11.3 Pathophysiological Changes of NBSD
- •11.4 Etiology and Clinical Features
- •11.5 Investigations and Diagnosis
- •11.7 Management
- •11.8 Clean Intermittent Catheterization
- •11.9 Anticholinergics
- •11.10 Botulinum Toxin Type A
- •11.11 Tricyclic Antidepressant Drugs
- •11.12 Surgical Management
- •Further Reading
- •12.1 Introduction
- •12.2 Etiology
- •12.3 Pathophysiology
- •12.4 Clinical Features
- •12.5 Investigations and Diagnosis
- •12.6 Management
- •Further Reading
- •13.1 Introduction
- •13.2 Embryology
- •13.3 Epispadias
- •13.3.1 Introduction
- •13.3.2 Etiology
- •13.3.4 Treatment
- •13.3.6 Female Epispadias
- •13.3.7 Surgical Repair of Female Epispadias
- •13.3.8 Prognosis
- •13.4 Bladder Exstrophy
- •13.4.1 Introduction
- •13.4.2 Associated Anomalies
- •13.4.3 Principles of Surgical Management of Bladder Exstrophy
- •13.4.4 Evaluation and Management
- •13.5 Cloacal Exstrophy
- •13.5.1 Introduction
- •13.5.2 Skeletal Changes in Cloacal Exstrophy
- •13.5.3 Etiology and Pathogenesis
- •13.5.4 Prenatal Diagnosis
- •13.5.5 Associated Anomalies
- •13.5.8 Surgical Reconstruction
- •13.5.9 Management of Urinary Incontinence
- •13.5.10 Prognosis
- •13.5.11 Complications
- •Further Reading
- •14.1 Introduction
- •14.2 Etiology
- •14.3 Clinical Features
- •14.4 Associated Anomalies
- •14.5 Diagnosis
- •14.6 Treatment and Prognosis
- •Further Reading
- •15: Cloacal Anomalies
- •15.1 Introduction
- •15.2 Associated Anomalies
- •15.4 Clinical Features
- •15.5 Investigations
- •Further Reading
- •16: Urachal Remnants
- •16.1 Introduction
- •16.2 Embryology
- •16.4 Clinical Features
- •16.5 Tumors and Urachal Remnants
- •16.6 Management
- •Further Reading
- •17: Inguinal Hernias and Hydroceles
- •17.1 Introduction
- •17.2 Inguinal Hernia
- •17.2.1 Incidence
- •17.2.2 Etiology
- •17.2.3 Clinical Features
- •17.2.4 Variants of Hernia
- •17.2.6 Treatment
- •17.2.7 Complications of Inguinal Herniotomy
- •17.3 Hydrocele
- •17.3.1 Embryology
- •17.3.3 Treatment
- •Further Reading
- •18: Cloacal Exstrophy
- •18.1 Introduction
- •18.2 Etiology and Pathogenesis
- •18.3 Associated Anomalies
- •18.4 Clinical Features and Management
- •Further Reading
- •19: Posterior Urethral Valve
- •19.1 Introduction
- •19.2 Embryology
- •19.3 Pathophysiology
- •19.5 Clinical Features
- •19.6 Investigations and Diagnosis
- •19.7 Management
- •19.8 Medications Used in Patients with PUV
- •19.10 Long-Term Outcomes
- •19.10.3 Bladder Dysfunction
- •19.10.4 Renal Transplantation
- •19.10.5 Fertility
- •Further Reading
- •20.1 Introduction
- •20.2 Embryology
- •20.4 Clinical Features
- •20.5 Investigations
- •20.6 Treatment
- •20.7 The Müllerian Duct Cyst
- •Further Reading
- •21: Hypospadias
- •21.1 Introduction
- •21.2 Effects of Hypospadias
- •21.3 Embryology
- •21.4 Etiology of Hypospadias
- •21.5 Associated Anomalies
- •21.7 Clinical Features of Hypospadias
- •21.8 Treatment
- •21.9 Urinary Diversion
- •21.10 Postoperative Complications
- •Further Reading
- •22: Male Circumcision
- •22.1 Introduction
- •22.2 Anatomy and Pathophysiology
- •22.3 History of Circumcision
- •22.4 Pain Management
- •22.5 Indications for Circumcision
- •22.6 Contraindications to Circumcision
- •22.7 Surgical Procedure
- •22.8 Complications of Circumcision
- •Further Reading
- •23: Priapism in Children
- •23.1 Introduction
- •23.2 Pathophysiology
- •23.3 Etiology
- •23.5 Clinical Features
- •23.6 Investigations
- •23.7 Management
- •23.8 Prognosis
- •23.9 Priapism and Sickle Cell Disease
- •23.9.1 Introduction
- •23.9.2 Epidemiology
- •23.9.4 Pathophysiology
- •23.9.5 Clinical Features
- •23.9.6 Treatment
- •23.9.7 Prevention of Stuttering Priapism
- •23.9.8 Complications of Priapism and Prognosis
- •Further Reading
- •24.1 Introduction
- •24.2 Embryology and Normal Testicular Development and Descent
- •24.4 Causes of Undescended Testes and Risk Factors
- •24.5 Histopathology
- •24.7 Clinical Features and Diagnosis
- •24.8 Treatment
- •24.8.1 Success of Surgical Treatment
- •24.9 Complications of Orchidopexy
- •24.10 Infertility and Undescended Testes
- •24.11 Undescended Testes and the Risk of Cancer
- •Further Reading
- •25: Varicocele
- •25.1 Introduction
- •25.2 Etiology
- •25.3 Pathophysiology
- •25.4 Grading of Varicoceles
- •25.5 Clinical Features
- •25.6 Diagnosis
- •25.7 Treatment
- •25.8 Postoperative Complications
- •25.9 Prognosis
- •Further Reading
- •26.1 Introduction
- •26.2 Etiology and Risk Factors
- •26.3 Diagnosis
- •26.4 Intermittent Testicular Torsion
- •26.6 Effects of Testicular Torsion
- •26.7 Clinical Features
- •26.8 Treatment
- •26.9.1 Introduction
- •26.9.2 Etiology of Extravaginal Torsion
- •26.9.3 Clinical Features
- •26.9.4 Treatment
- •26.10 Torsion of the Testicular or Epididymal Appendage
- •26.10.1 Introduction
- •26.10.2 Embryology
- •26.10.3 Clinical Features
- •26.10.4 Investigations and Treatment
- •Further Reading
- •27: Testicular Tumors in Children
- •27.1 Introduction
- •27.4 Etiology of Testicular Tumors
- •27.5 Clinical Features
- •27.6 Staging
- •27.6.1 Regional Lymph Node Staging
- •27.7 Investigations
- •27.8 Treatment
- •27.9 Yolk Sac Tumor
- •27.10 Teratoma
- •27.11 Mixed Germ Cell Tumor
- •27.12 Stromal Tumors
- •27.13 Simple Testicular Cyst
- •27.14 Epidermoid Cysts
- •27.15 Testicular Microlithiasis (TM)
- •27.16 Gonadoblastoma
- •27.17 Cystic Dysplasia of the Testes
- •27.18 Leukemia and Lymphoma
- •27.19 Paratesticular Rhabdomyosarcoma
- •27.20 Prognosis and Outcome
- •Further Reading
- •28: Splenogonadal Fusion
- •28.1 Introduction
- •28.2 Etiology
- •28.4 Associated Anomalies
- •28.5 Clinical Features
- •28.6 Investigations
- •28.7 Treatment
- •Further Reading
- •29: Acute Scrotum
- •29.1 Introduction
- •29.2 Torsion of Testes
- •29.2.1 Introduction
- •29.2.3 Etiology
- •29.2.4 Clinical Features
- •29.2.5 Effects of Torsion of Testes
- •29.2.6 Investigations
- •29.2.7 Treatment
- •29.3 Torsion of the Testicular or Epididymal Appendage
- •29.3.1 Introduction
- •29.3.2 Embryology
- •29.3.3 Clinical Features
- •29.3.4 Investigations and Treatment
- •29.4.1 Introduction
- •29.4.2 Etiology
- •29.4.3 Clinical Features
- •29.4.4 Investigations and Treatment
- •29.5 Idiopathic Scrotal Edema
- •29.6 Testicular Trauma
- •29.7 Other Causes of Acute Scrotum
- •29.8 Splenogonadal Fusion
- •Further Reading
- •30.1 Introduction
- •30.2 Imperforate Hymen
- •30.3 Vaginal Atresia
- •30.5 Associated Anomalies
- •30.6 Embryology
- •30.7 Clinical Features
- •30.8 Investigations
- •30.9 Management
- •Further Reading
- •31: Disorders of Sexual Development
- •31.1 Introduction
- •31.2 Embryology
- •31.3 Sexual and Gonadal Differentiation
- •31.5 Evaluation of a Newborn with DSD
- •31.6 Diagnosis and Investigations
- •31.7 Management of Patients with DSD
- •31.8 Surgical Corrections of DSD
- •31.9 Congenital Adrenal Hyperplasia (CAH)
- •31.10 Androgen Insensitivity Syndrome (Testicular Feminization Syndrome)
- •31.13 Gonadal Dysgenesis
- •31.15 Ovotestis Disorders of Sexual Development
- •31.16 Other Rare Disorders of Sexual Development
- •Further Reading
- •Index
23.9 Priapism and Sickle Cell Disease |
521 |
|
|
saline and injecting 20 mL in repeated boluses, until a maximum of ten injections (200 mL).
•Etilefrine:
–5–10 mg per intracavernosal injection, without dilution.
•All patients who arrive at the emergency department within 36 h of priapism respond to the treatment regimen.
•Etilefrine can be used to treat priapism in patients with SCD.
–5 mg of undiluted intracavernosal etilefrine (if priapism was present for less than 6 h) or aspiration followed by irrigation with intracavernosal etilefrine (if priapism had been present for greater than or equal to 6 h).
•If the priapism continues beyond approximately 12 h, shunt procedure should be considered.
•The shunt procedure should be the last option, as it is associated with higher rates of impotence, and most pediatric patients respond well to pharmacologic treatments.
•To prevent relapse of priapism, patients can be treated with oral etilefrine 0.25 mg/kg twice a day for 1 month.
•Other less commonly used medications to treat priapism include:
–Phosphodiesterase inhibitors: A single oral dose of 50 mg is used
–Ketamine injections (0.5–1 mg/kg)
–Hydralazine
–Calcium-channel blockers
–Anticoagulants
–Corticosteroids
–Continuous epidural anesthesia
–Inhaled nitric oxide
•Surgery (Figs. 23.14 and 23.15):
–Most authors would indicate surgery only in low flow priapism episodes, after 12 h, if conventional medical treatment and injection of the corpora cavernosa with adrenergics could not solve the problem.
–This can be performed by a distal cavernosa-spongiosum shunt:
•Winter shunt: This creates a cavernosaspongiosum shunt by puncturing the glans with a Tru-Cut needle
•Al-Ghorab shunt: This suture the distal extremity of the corpora cavernosa to the spongiosum into the glans (spongiosumcavernous anastomoses)
–Or a proximal shunt:
•Grayhack shunt: laterolateral spongiosum to proximal penile corpora cavernosa suture
•A cavernosa-venous diversion to the saphenous vein (saphenous-cavernous) shunts or to the dorsal vein of the penis.
–The placement of a penile prosthesis should be considered in adulthood, so that patients with erectile dysfunction as a consequence of prior crises can become sexually active.
23.9.7Prevention of Stuttering Priapism
•Prophylaxis of recurrence of acute episodes or of occurrence of acute episodes in patients with recurrent self-limited priapism include the following therapeutic proposals:
–First-line treatment should begin with an oral adrenergic agonist, as they seem to have the best efficacy and safety profiles.
–Etilefrine is the best evidence-supported treatment available.
–Stuttering priapism is treated with oral etilefrine 0.5 mg/kg for 1 month. A dose is given once every evening in patients with nocturnal priapism or divided into two doses for priapism occurring during the day and at night. The treatment is continued for 1 month after eventual resolution with no recurrence.
–This can be combined with intracavernosal self-injection in cases of acute episodes lasting more than 1 h.
–Phenylpropanolamine is an acceptable alternative.
–Phenylephrine and epinephrine are not available in an orally active formulation.
522 |
23 Priapism in Children |
|
|
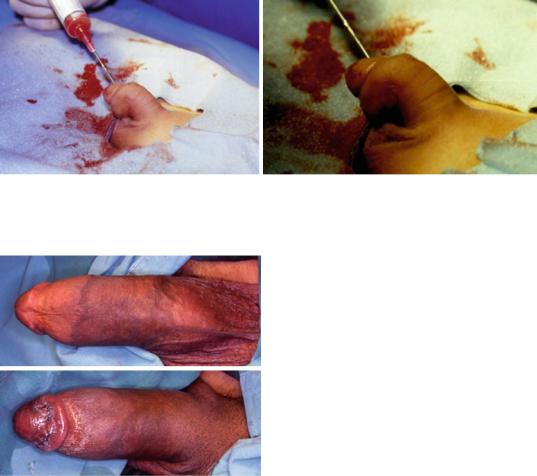
Figs. 23.12 and 23.13 Clinical photographs showing priapism in a child with SCA being treated with aspiration and irrigation. Note the response to the treatment with resolution of priapism
Figs. 23.14 and 23.15 Clinical photograph showing priapism in an adult with SCA being treated with a distal glans-cavernosal shunt
–Pseudoephedrine is the only preferred oral adrenergic agonist available. It may be given as a once-daily dose at bedtime or as two doses given in the morning and at bedtime
–Terbutaline is an alternative, but it should be considered a second-line therapy behind pseudoephedrine, as there is less evidence supporting its efficacy.
–Other oral agents that may be tried if pseudoephedrine fails include hydralazine, pentoxifylline, and diltiazem, although evidence for the use of these three drugs is weak, and their routine use cannot be fully advocated.
–The third step that should be considered is the use of a gonadotropin-releasing hormone analogue plus flutamide.
•Leuprolide is the agent of choice.
•Flutamide should be given initially to minimize the testosterone flare often seen upon initiation of gonadotropinreleasing hormone analogues.
–Hormonal manipulation is also used in the treatment of recurrent priapism.
–Gonadotropin-releasing hormone analogues have fewer risks and adverse effects than those seen with diethylstilbestrol.
–Overall, gonadotropin-releasing hormone analogues appear to be relatively safe and well tolerated by most patients.
–Gonadotropin-releasing hormone analogues also offer the convenience of monthly or quarterly administration rather than the daily or weekly administration needed with oral medications.
–Use of anti-androgenic hormonal manipulation, using gonadotrophin inhibitors (goserelin, leuprolide) or finasteride to reduce androgen levels.
–This treatment, although efficacious, is associated with side effects (loss of libido and erectile function). Those drugs are second- or third-line treatment options.
–Adverse effects have been reported in over 2 % of pediatric patients using leuprolide and include injection-site reactions, generalized pain, rash, and acne. The concern
23.9 Priapism and Sickle Cell Disease |
523 |
|
|
with using them in pediatric patients is that sexual maturation may be delayed secondary to the reduction of circulating androgens, which can cause the reproductive organs to return to a prepubertal state.
–Other agents which may be considered are diethylstilbestrol and hydroxyurea.
•Diethylstilbestrol is effective but has side effects.
•Hydroxyurea should decrease the degree of sickling, which is thought to be the major cause of priapism in patients with SCD. However, its adverse effects also limit its use.
–Diethylstilbestrol:
•This is used to abort and prevent stuttering priapism.
•The exact mechanism by which diethylstilbestrol works is unknown.
•Its use is limited by the recurrence of symptoms 6–8 weeks after discontinuation of the medication and because of the side effects (loss of libido and erectile function, gynecomastia, testicular atrophy).
•It should be considered a last resort medication, not appropriate for use in pre-pubescent patients.
• Diethylstilbestrol 5 mg daily for 3–4 days could abort attacks of priapism, and individualized dosages lower than 5 mg daily could be used to prevent priapism.
•Other adverse effects commonly experienced with diethylstilbestrol include breast tenderness and enlargement, nausea, vomiting, abdominal cramps, headache, dizziness, weight changes, edema, changes in libido, hirsutism, and testicular atrophy.
–Hydroxyurea:
•It induces the synthesis of fetal hemoglobin, modifying the mechanisms of endothelial activation and resulting in general improvement of SCD.
•It may also reduce neutrophil and reticulocyte counts, thereby decreasing the interaction of sickle cells with vascular
endothelium resulting in blood “trapping” and, thus, priapism.
•It is often used to treat patients with SCD who have recurrent pain crises.
•Hydroxyurea maybe useful in the treatment of sickle-cell-induced priapism.
•Given the side effects and risks, this approach has been reserved for serious cases.
•Its adverse effects preclude its use as a first-line drug to treat priapism.
•Major adverse effects of hydroxyurea include myelosuppression (leukopenia, anemia, and occasionally thrombocytopenia), elevation of hepatic enzymes, gastrointestinal symptoms (nausea, vomiting, diarrhea, constipation, stomatitis, anorexia), renal impairment, fever, chills, malaise, edema, erythema, and rash.
–There have been case reports describing the isolated but successful use of other pharmacologic agents to induce detumescence in patients with prolonged erection such as ketamine and hydralazine.
–Methylene blue injected intracavenously has also been reported to be effective in the treatment of priapism. Methylene blue can however cause necrotic abscess.
– The use of erythrocyte transfusions for 6 months, followed by pentoxifylline for
6 months.
•Blood transfusion:
–Both simple and exchange transfusions have been used in attempts to increase the hemoglobin and hematocrit, decrease the number of sickled red blood cells, decrease hemoglobin S levels, and increase the number of oxygenated, normal erythrocytes.
–Exchange transfusions have been questioned for three main reasons:
• Absence of good quality scientific evidence of its efficacy.
• The well-known risks associated with transfusion.
• Availability of blood and difficulties in obtaining blood for emergency exchange and noncompliance of parents when it is used to prevent recurrent attacks.
