
- •Contents
- •1. Cell Biology and Epithelia
- •2. Connective Tissue
- •3. Cartilage and bone
- •5. Nervous Tissue
- •6. Immune Tissues
- •7. Respiratory System
- •8. Gastrointestinal System
- •12. Integument
- •1. Gonad Development
- •4. Embryonic Period (Weeks 3-8)
- •1. Back and Autonomic Nervous System
- •2. Thorax
- •5. Lower Limb
- •4. The Spinal Cord
- •5. The Brain Stem
- •7. Basal Ganglia
- •11. Limbic System
- •Index

Respiratory System |
7 |
The lung is an organ that functions in the intake ofoxygen and exhaling of C02. Approximately 14 times each minute, we take in about 500 ml ofair per breath. Inspired air willbe spread over 120 square meters ofthe surface area ofthe lungs. The air-blood barrier has to be thin enough for air to pass across but tough enough to keep the blood cells inside their capillaries.
Lungs are opened to the outside world so that they are susceptible to environ mental insults in the form ofpollution and infectious bacteria.
The lungs receive the entire cardiac output and are positioned to modify various blood components. The pulmonary endothelium plays an active role in the meta bolic transformation of lipoproteins and prostaglandins. The enzyme that con verts angiotensin I to angiotensin II is produced bythe lung endothelial cells.
Clinical Correlate
•Any disease that affects capillaries also affects the extensive capillary bed ofthe lungs. Bacteria which colonize the lungs may damage the barriers between the alveoli and the capillaries, gaining access to the bloodstream (a common complication of bacterial pneumonia).
•In individuals with allergies, smooth-muscle constriction reduces the diameter of air tubes and results in reduced air intake.
•Lung cancers commonly develop from bronchi (smoking, asbestos, and excessive radiation are the main causes).
•Mesothelioma is a malignant tumor of the pleura (causative agent: asbestos dust).
MEDICAL 77


Chapter 7 • Respiratory System
PULMONARY DEFENSE MECHANISMS
Inhaled air contains hazardous dusts, chemicals, and microorganisms, yet lung tissue is usually sterile. Inhaled particles are deposited on the walls of airways according to size.
•Particles 10 microns in diameter or larger are trapped in the nose and are removed by sneezing, blowing, or swallowing.
•Particles 3-10 microns in diameter are trapped and removed by the tracheobronchial mucociliary escalator.
•Particles 0.5-3 microns in diameter (bacterial size) may reach the alveolar tissue and are removed by alveolar clearance.
•Macrophages that reside in the alveolar spaces phagocytose the small particles and transport them by amoeboid movement into bronchioles, lymphatics, and capillaries. Sometimes they remain trapped in connec tive tissue septa.
TRACHEA
The trachea is a hollow tube, about 10 cm in length (and about 2 cm in diameter), extending from the larynx to its bifurcation at the carina to form a primary bron chus for each lung. The most striking structures of the trachea are the C-shaped hyaline cartilage rings. In the human there are about 16 to 20 ofthem distributed along the length of the trachea. The rings overlap in the anterior part of the tra chea. The free posterior ends of the C-shaped cartilages are interconnected by smooth-muscle cells.
Copyright McGraw-Hill Companies. Used with permission.
Figure 1-7-2. Trachea with a hyaline cartilage ring (arrow) and pseudostratified columnar epithelium
The trachea is composed of concentric rings of mucosa, submucosa, an incom plete muscularis, and an complete adventitia.
•The mucosa has 3 components: a pseudostratified epithelium, an underlying vascularized loose connective tissue (lamina propria) that contains immune cells, and a thin layer of smooth-muscle cells (mus cularis mucosa).
MEDICAL 79

Section I • Histology and Cell Biology
Clinical Correlate
If mucosa! clearance is ineffective, or the mechanism overwhelmed, infection (pathogenic bacteria) or
pneumoconiosis (dust-related disease) may follow.
In cystic fibrosis, the secreted mucus is thick or viscous and the cilia have a difficult time moving it toward the pharynx. Patients with this disease have frequent infections of the respiratory system.
Clinical Correlate
Patients lacking dynein have immotile cilia or Kartagener syndrome.
With immotile cilia, patients are subject to many respiratory problems because their cilia cannot move this mucus layer with its trapped bacteria. Males also possess immotile sperm.
80 MEDICAL
•The submucosa is a vascular service area containing large blood vessels. Collagen fibers, lymphatic vessels and nerves are also present in this layer.
•The outside covering of the trachea, the adventitia, is composed of several layers of loose connective tissue.
The epithelial lining of the trachea and bronchi is pseudostratified columnar in which all cells lie on the same basal membrane but only some reach the luminal surface. The only other place in the body with this epithelium is the male repro ductive tract.
Copyright McGraw-Hill Companies. Used with permission.
Figure 1-7-3. Pseudostratified columnar epithelium with goblet cells (arrowhead) surrounded by ciliated cells (arrow)
Tracheal Epithelial CellTypes
Columnar cells extend from the basal membrane to the luminal surface. These cells contain approximately 200 to 300 apical cilia per cell that are intermingled with microvilli. The cilia are motile and beat to help move the secreted mucus layer over the lining of the trachea and out of the respiratory system.
Goblet cells secrete a polysaccharide mucous material into the lumen of tra chea. Mucus production is supplemented by secretions of the submucosal mixed glands. The mucus layer of the respiratory system traps particulate substances (dust, bacteria, and viruses) and absorbs noxious water-soluble gases such as ozone and sulfur dioxide. The mucus sticky layer is moved by the beating cilia toward the pharynx where it is swallowed. This movement is known as the mu cociliary escalator system. Most material (dust and bacteria) is trapped in the mucus layer, and is removed and digested.
Pulmonary neuroendocrine (PNE) cells are comparable to the endocrine cells in the gut. These epithelial neuroendocrine cells have been given various names:
•APUD cells (Amino-Precursor-Uptake-Decarboxylase) , DNES cells (Diffuse Neuro Endocrine System) and K (Kulchitsky) cells. The granules in these neuroendocrine cells contain hormones and active

peptides, bombesin (gastrin-releasing factor), leu-enkephalin, sero tonin, and somatostatin. These cells occur in clusters and are often located at airway branch points.
•Brush cells may represent goblet cells that have secreted their products or intermediate stages in the formation of goblet or the tall ciliated cells. They have short microvilli on their apical surfaces. Some of these cells have synapses with intraepithelial nerves, suggesting that these cells may be sensory receptors.
Basal cells are stem cells for the ciliated and goblet cells. The stem cells lie on the basal membrane but do not extend to the lumen ofthe trachea. These cells, along with the epithelial neuroendocrine cells, are responsible for the pseudostratified appearance ofthe trachea.
BRONCHI
The bronchial tree forms a branching airway from the trachea to the bronchioles. When the primary bronchi enter the lung, they give rise to 5 secondary or lobar bronchi-3 for the right lung and 2 for the left. The 5 lobes are further subdivided into 10 tertiary or segmental bronchi in each lung, which form bronchopulmo nary segments.
Chapter 7 • Respiratory System
Clinical Correlate
The columnar and goblet cells are sensitive to irritation. The ciliated cells become taller, and there is an increase in the number of goblet cells and submucosal glands.
Intensive irritation from smoking leads to a squamous metaplasia where
the ciliated epithelium becomes a squamous epithelium. This process is reversible.
Clinical Correlate
Bronchial metastatic tumors arise from Kulchitsky cells.
CopyrightMcGraw-Hi/I Companies. Used with permission.
Figure 1-7-4. Bronchus with a plate of cartilage (arrow)
The epithelial lining of the bronchi is also pseudostratified. It consists of cili ated columnar cells, basal cells, mucus cells, brush cells and neuroendocrine
(APUD,gul DNES, or K) cells. There are also seromucous glands in the submucosa that empty onto the epithelial surface via ducts. The walls of bronchi contain ir re ar plates of cartilage and circular smooth-muscle fascicles bound together by elastic fibers. The number ofgoblet cells and submucosa glands decreases from the trachea to the small bronchi.
Clinical Correlate
Cystic fibrosis that results in abnormally thick mucus is in part due to defective chloride transport by Clara cells.
MEDICAL 81

Section I • Histology and Cell Biology
Clinical Correlate
Chronic obstructive pulmonary disease (COPD) affects the bronchioles and includes emphysema and asthma.
•Emphysema is caused by a loss of elastic fibers and results in chronic airflow obstruction.
•Asthma is a chronic process characterized by a reversible narrowing of airways.
•Asthma is reversible; emphysema is not.
BRONCHIOLES
The wall ofabronchioledoes not contain cartilage or glands. The smooth-muscle fascicles are bound together by elastic fibers. The epithelium is still ciliated, but is a simple cuboidal or columnar epithelium rather than pseudostratified. The epi thelial lining of the airway is composed of ciliated cells (goblet and basal cells are absent in the terminal bronchioles) and an additional type called the Clara cell.
Clara cells (also called bronchiolar secretory cells) are nonciliated and secrete a serous solution similar to surfactant. They aid in the detoxificationofairborne toxins, and serve as a stem cell for the ciliated cells and for themselves. The num ber of Clara cells increases in response to increased levels of pollutants like ciga rette smoke. Clara cells are most abundant in the terminal bronchioles, where theymake up about 80 % ofthe epithelial cell lining; they are also involved with chloride ion transport into the lumens of the terminal bronchioles.
Copyright McGraw-Hill Companies. Used with permission.
Figure 1-7-5. Terminal bronchiole lumen (asterisk) with epithelium containing ciliated cells and Clara cells (arrows)
Terminal Bronchioles
The terminalbronchiole is the last conducting bronchiole. This bronchiole is fol lowed by respiratory bronchioles which are periodically interrupted by alveoli in their walls. The goblet cells are absent from the epithelial linings of the respi ratory bronchioles, but are still lined with a sparse ciliated cuboidal epithelium that prevent the movement of mucous into the alveoli. After the last respiratory bronchiole, the wall of the airway disappears and air enters the alveoli.
82 MEDICAL

Section I • Histology and Cell Biology
Clinical Correlate
Surfactant is synthesized after week 35 of gestation. Coricosteroids
induce the fetal synthesis of surfactant. High insulin levels in diabetic
mothers antagonize the effects of corticosteroids.
Infants of diabetic mothers have a higher incidence of respiratory distress syndrome.
84 MEDICAL
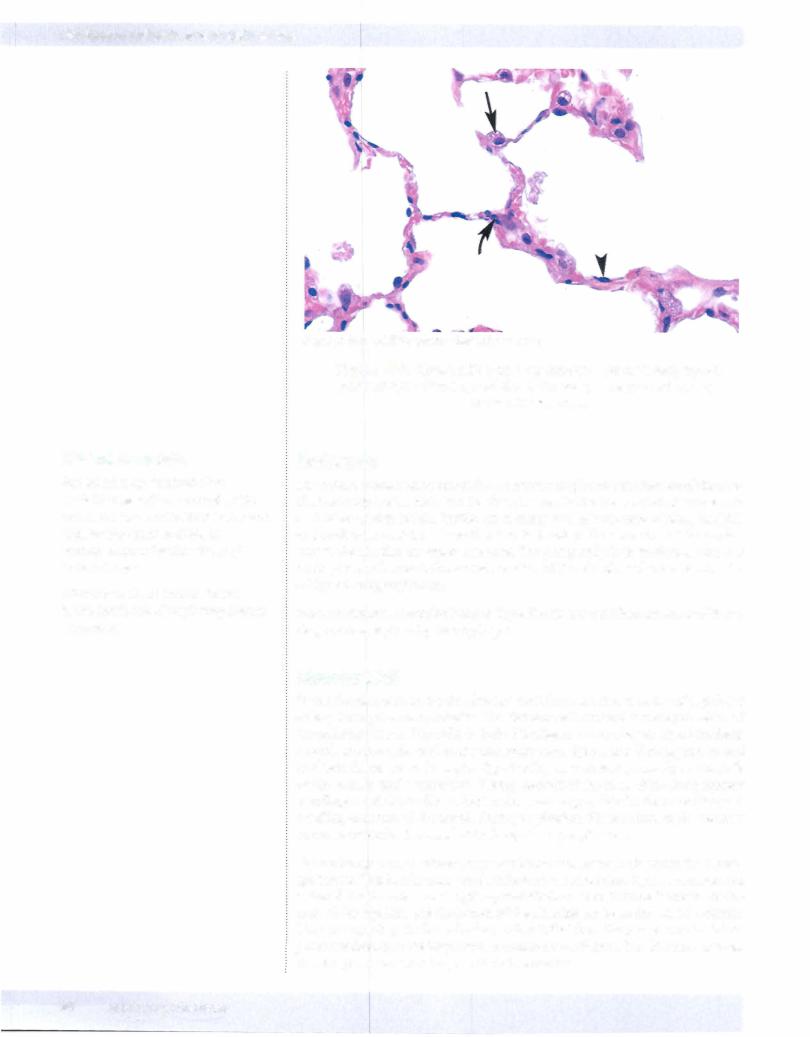
Copyright McGraw-Hill Companies. Used with permission.
Figure 1-7-7. Alveoli with type I pneumocytes (arrowhead), type II pneumocytes (arrow), and alveolar macrophage (curved arrow) in the alveolar wall.
Surfactant
Surfactant is essential to maintain the normal respiratory mechanics ofthe alve oli. Production ofsurfactant in the fetus is essential for the survival ofthe neonate as it takes its first breath. Surfactant is composed of a mixture of phospholipids and surfactant proteins whose function is to aid in the spreading of the surfac tant at the alveolar air-water interface. The phospholipid in surfactant acts as a detergent which lowers the surface tension of the alveoli, and prevents alveolar collapse during expiration.
Most surfactant is recycled back to Type II cells for reutilization; some of it un dergoes phagocytosis by macrophages.
AlveolarWall
In the alveolarwallunder the alveolar epithelium is a rich network of capillaries arising from pulmonary arteries. The alveolar wall contains a variety of cells and extracellular fibers. The cells include fibroblasts, macrophages, myofibroblasts, smooth-muscle cells, and occasional mast cells. Type I and II collagens, as well as elastic fibers, are in the septa. Type I collagen is present primarily in the walls of the bronchi and bronchioles. Twenty percent of the mass of the lung consists of collagen and elastic fibers. Elastic fibers are responsible for the stretching and recoiling activities of the alveoli during respiration. These microscopic elements are responsible for the recoil of the lungs during expiration.
Gas exchange occurs between capillary blood and alveolar air across the blood gas barrier. This barrier consists ofsurfactant, the squamous Type I pneumocytes, a shared basal lamina, and capillary endothelium. The distance between the lu men of the capillary and the lumen of the alveolus can be as thin as 0. 1 microns. There are openings in the wall of most alveoli that from the poresofKohn. These pores are thought to be important in collateral ventilation. The diameter ofthese alveolar pores can be as large as l 0 to 15 microns.

Alveolar Macrophages
The alveolarmacrophages are derived from monocytes that exit the blood vessels in the lungs. The resident alveolar macrophages can undergo limited mitoses to form additional macrophages. These cells can reside in the interalveolar septa as well as in the alveoli. Alveolar macrophages that patrol the alveolar surfaces may pass through the pores of Kohn.
There are about 1 to 3 macrophages per alveolus. Alveolar macrophages vary in size from 15 to 40 microns in diameter. These macrophages represent the last defense mechanism of the lung. Macrophages can pass out of the alveoli to the bronchioles and enter the lymphatics or become trapped in the moving mucus layer and propelled toward the pharynx to be swallowed and digested. About 100 million lung macrophages are swallowed each day.
ChapterSummary
•The nasal cavities have 2 major areas: respiratory and olfactory.
•The respiratory area is lined by pseudostratified, ciliated columnar epithelium. Goblet cells are present as well. The olfactory area is in the posterosuperior area and contains bipolar neurons. Olfactory neurons are constantly replenished. Paranasal sinuses are located in the frontal, maxillary, ethmoid, and sphenoidal bones. They communicate with the nasal cavities. The nasopharynx is composed of stratified, squamous
nonkeratinized epithelium. The pharyngeal tonsil is an aggregate of nodular and diffuse lymphatic tissue within the posterior wall ofthe nasopharynx.
•Histologic features of the trachea, bronchi, and bronchioles are described in Table 1-7- 1 . Respiratory bronchioles contain alveoli and branch to form alveolar ducts, which terminate in alveolar sacs and are lined by squamous alveolar epithelium. Alveoli are terminal, thin-walled sacs of the respiratory tree responsible for gaseous exchange. They contain 2 kinds of cells.
-Type I cells provide a thin surface forgaseous exchange
-Type II cells produce surfactant.
Alveolar macrophages (dust cells) are located on the surface of alveoli and within the interalveolar connective tissue. They are derived from monocytes.
Chapter 7 • Respiratory System
Clinical Correlate
Alveolar macrophages have several other names: dust cells because they have phagocytosed dust or cigarette particles, and heart failure cells because they have phagocytosed blood cells that have escaped into the alveolar space during congestive heart failure.
MEDICAL 85

