
- •Contents
- •1. Cell Biology and Epithelia
- •2. Connective Tissue
- •3. Cartilage and bone
- •5. Nervous Tissue
- •6. Immune Tissues
- •7. Respiratory System
- •8. Gastrointestinal System
- •12. Integument
- •1. Gonad Development
- •4. Embryonic Period (Weeks 3-8)
- •1. Back and Autonomic Nervous System
- •2. Thorax
- •5. Lower Limb
- •4. The Spinal Cord
- •5. The Brain Stem
- •7. Basal Ganglia
- •11. Limbic System
- •Index

Gonad Development |
1 |
INDIFFERENT GONAD
Although sex is determined at fertilization, the gonads initially go through an indifferent stage between weeks 4 and 7 when there are no specific ovarian or testicular characteristics.
The indifferent gonads develop in a longitudinal elevation or ridge ofintermedi ate mesoderm called the urogenital ridge.
Primordial Germ Cells
Primordial germ cells arise from the lining cells in the wall ofthe yolk sac.
At week 4, primordial germ cells migrate into the indifferent gonad.
Components ofthe Indifferent Gonad
•Primordial germ cells migrate into the gonad from the yolk sac and provide a critical inductive influence on gonad development.
•Primary sex cords are fingerlike extensions of the surface epithelium that grow into the gonad that are populated by the migrating primordial germ cells.
•Mesonephric (Wolffian) and the paramesonephric (Mullerian) ducts of the indifferent gonad contribute to the male and female genital tracts, respectively.
|
|
MEDICAL |
155 |


Chapter 1 • Gonad Development
MEIOSIS
Meiosis occurs within the testes and ovary. This is a specialized process of cell division that produces the male gamete (spennatogenesis) and female gamete (oogenesis). There are notable differences between spermatogenesis and oogen esis, discussed below.
Meiosis consists of 2 cell divisions, meiosis I and meiosis II (Figure II- 1 -2).
Meiosis I
In meiosis I, the following events occur:
•Synapsis-the pairing of 46 homologous chromosomes
•Crossingover-the exchange of segments of DNA
•Disjunction-the separation of 46 homologous chromosomes without centromere-splitting
Meiosis II
In meiosis II:
•Synapsis does not occur.
•Crossing over does not occur.
•Disjunction occurs with centromere-splitting.
MEDICAL 157


Chapter 1 • Gonad Development
SPERMATOGENESIS
•Primordial germ cells arrive in the indifferent gonad at week 4 and remain dormant until puberty.
•When a boy reaches puberty, primordial germ cells differentiate into type A spermatogonia, which serve as stem cells throughout adult life.
•Some type A spermatogonia differentiate into type B spermatogonia.
•Type B spermatogonia enter meiosis I to form primary spermatocytes.
•Primary spermatocytes form 2 secondary spermatocytes.
•Secondary spermatocytes enter meiosis II to form 2 spermatids.
•Spermatids undergo spermiogenesis, which is a series of morphological changes resulting in the mature spermatozoa.
OOGENESIS
•Primordial germ cells arrive in the indifferent gonad at week 4 and dif ferentiate into oogonia.
•Oogonia enter meiosis I to form primary oocytes. Allprimary oocytes are formed by month 5 offetallife and are arrested the first time in prophase (diplotene) ofmeiosis I and remain arrested until puberty.
•Primary oocyte arrested in meiosis I are present at birth.
•When a girl reaches puberty, during each monthly cycle a primary oocyte becomes unarrested and completes meiosis I to form a secondary oocyte and polar body.
•The secondary oocyte becomes arrested the second time in metaphase of meiosis II and is ovulated.
•At fertilization within the uterine tube, the secondary oocyte completes meiosis II to form a mature oocyte and polar body.
MEDICAL 1 59

Section II • Early Embryology
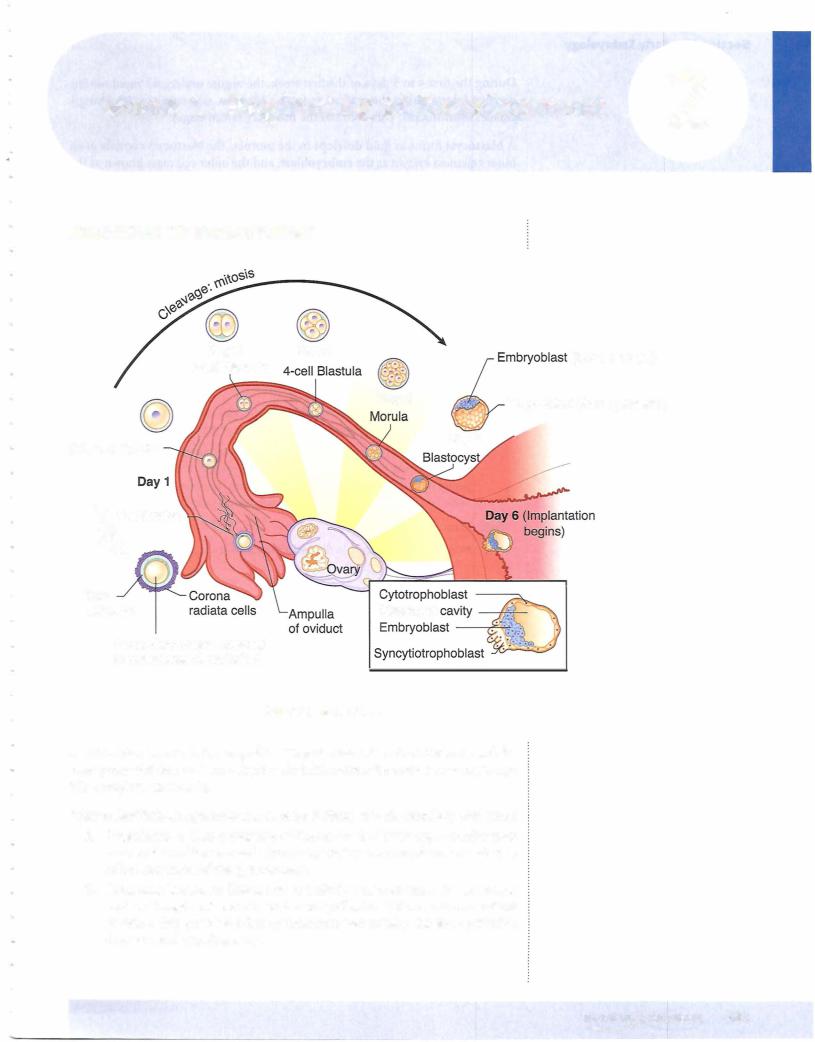
During the first 4 to 5 days ofthe first week, the zygote undergoes rapid mitotic division (cleavage) in the oviduct to form a blastula, consisting of increasingly smaller blastomeres. This becomes the morula (32-cell stage).
A blastocyst forms as fluid develops in the morula. The blastocyst consists ofan inner cell mass known as the embryoblast, and the outer cell mass known as the trophoblast, which becomes the placenta.
At the end of the first week, the trophoblast differentiates into the cytotropho blast and syncytiotrophoblast and then implantation begins (see below).
Clinical Correlate
Ectopic Pregnancy
Tubal
•The most common form of ectopic pregnancy; usually occurs when the blastocyst implants within the ampulla ofthe uterine tube because of delayed transport
•Risk factors: endometriosis, pelvic inflammatory disease (PID), tubular pelvic surgery, or exposure to diethylstilbestrol (DES)
•Clinical signs: abnormal or brisk uterine bleeding, sudden onset of abdominal pain that may be confused with appendicitis, missed menstrual period (e.g., LMP 60 days ago), positive human chorionic gonadotropin (hCG) test, culdocentesis showing intraperitoneal blood, positive sonogram
Abdominal
•Most commonly occurs in the rectouterine pouch (pouch of Douglas)
Implantation
The zona pellucida must degenerate for implantation to occur.
The blastocyst usually implants within the posterior wall ofthe uterus.
The embryonic pole ofblastocyst implants first.
The blastocyst implants within the functional layer of the endometrium during the progestational phase ofthe menstrual cycle.
Chapter Summary
•Fertilization occurs in the ampulla ofthe uterine tube with the fusion of the male and female pronuclei to form a zygote. During the first 4-5 days of
the first week, the zygote undergoes rapid mitotic division (cleavage) in the oviduct to form a morula before entering the cavity ofthe uterus.
•A blastocyst forms as fluid develops in the morula, resulting in a blastocyst that consists of an inner cell mass known as the embryoblast (becomes the embryo) and the outer cell mass known as the trophoblast (becomes the placenta). At the end ofthe first week, the trophoblast differentiates into the cytotrophoblast and syncytiotrophoblast and then implantation begins.
162 MEDICAL


Section II • Early Embryology
Extraembryonic mesoderm is derived from the epiblast. Extraembryonic somatic mesoderm lines the cytotrophoblast, forms the connecting stalk, and covers the am nion. Extraembryonic visceral mesoderm covers the yolk sac.
The connecting stalk suspends the conceptus within the chorionic cavity. The wall ofthe chorionic cavityis called the chorion, consisting ofextraembryonic somatic mesoderm, the cytotrophoblast, and the syncytiotrophoblast.
The syncytiotrophoblast continues its growth into the endometriurn to make con tact with endometrial blood vessels and glands. No mitosis occurs in the syncytio trophoblast. The cytotrophoblast is mitotically active.
Hematopoiesis occurs initially in the mesoderm surrounding the yolk sac (up to 6 weeks) and later in the fetal liver, spleen, thymus (6 weeks to third semester), and bone marrow.
Clinical Correlate
Human chorionic gonadotropin (hCG) is a glycoprotein produced by the syncytiotrophoblast. It stimulates progesterone production by the corpus luteum. hCG can be assayed in maternal blood or urine and is the basis for early pregnancy testing. hCG is detectable throughout pregnancy.
•Low hCG levels may predict a spontaneous abortion or ectopic pregnancy.
•High hCG levels may predict a multiple pregnancy, hydatidiform mole, or gestational trophoblastic disease.
ChapterSummary
•In the second week, implantation is completed with the rapid growth and erosion ofthe syncytiotrophoblast into the endometrium of the uterus where early utero-placental circulation is established. The inner cell mass of the first week differentiates into the epiblast and hypoblast cells and forms a bilaminar embryonic disk. An amniotic cavity develops from the epiblast and the primary yolk sac replaces the blastocyst cavity.
•The extraembryonic mesoderm and chorion are formed in the second week.
164 MEDICAL
