
- •Contents
- •1. Cell Biology and Epithelia
- •2. Connective Tissue
- •3. Cartilage and bone
- •5. Nervous Tissue
- •6. Immune Tissues
- •7. Respiratory System
- •8. Gastrointestinal System
- •12. Integument
- •1. Gonad Development
- •4. Embryonic Period (Weeks 3-8)
- •1. Back and Autonomic Nervous System
- •2. Thorax
- •5. Lower Limb
- •4. The Spinal Cord
- •5. The Brain Stem
- •7. Basal Ganglia
- •11. Limbic System
- •Index

Connective Tissue |
2 |
Connective tissue (CT) provides supportforparenchymalcells (epithelial andother functional cell types) that carry out the specific tissue and organ functions. Paren chymal cells are not only attached to and supported by connective tissue, they also have active mechanical, chemical, and other interactions between parenchymal cells and components of the connective tissue. CT is comprised of support cells, guest cells, and their associated extracellularmatrix (ECM) or ground substance.
CopyrightMcGraw-Hi// Companies. Usedwithpermission.
Figure 1-2-1. Loose connective tissue (LCT)
LCT contains collagen fibers and elastic fibers (arrows); mast cells are one type of CT permanent guest cell (arrowheads)
SUPPORT CELLS
Support cells include fibroblasts, myofibroblasts, chondroblasts, and osteoblasts and their derivatives, adipocytes.
Fibroblasts are the principle cells that produce collagen, and are also thought to have a role in the ordering of collagen fibrils and fibers in the ECM through attachment ofthe extracellular collagen to fibroblast membranes. Fibroblasts are more resistant to injury than most other cell types and are crucial in the response to injury.
Myofibroblasts share many of the features of fibroblasts (and may be derived from them), but additionally contain actin microfilaments and myosin thick fila ments, adding an intrinsic ability ofcell contraction. This is critical in reshaping tissue as it repairs after injury.
Note
There are 2 types of CT proper: loose and dense. Dense CT may be regular or irregular.
There are 4 types of special CT: adipose, cartilage, bone, and bone marrow.
MEDICAL 27

Section I • Histology and Cell Biology
Note
Tissue-specific macrophages:
Kupffer cells-liver
Osteoclasts-bone
Microglia-CNS
Chondroblasts and chondrocytes produce the type II collagen in cartilage. Car tilage covers the articular surfaces ofbones, and is found in the ears, nose, larynx, and tracheobronchial tree.
Osteoblasts andosteocytes produce the type I collagen in bone, along with other components of bone ECM (osteoid).
Adipocytes are the principal support cell in fat (adipose tissue) and may be found in other organs as well. There are 2 basic types of fat cells. In the adult, all or most fat is white fat or unilocular fat. A single adipocyte contains a single huge vacuole of fat (not membrane-bound), which pushes and flattens the cell nucleus to one side. Adipose cells have a surrounding external lamina and type III reticulin collagen fibers are found between the adipocytes. Brown fat or mul tilocular fat is a second type of fat found in fetuses and neonates (occasionally in small amounts in adults) that is composed of adipocytes with multiple small vacuoles offat and with a round central nucleus. This type of fat is thought to be important in generating heat in the newborn.
PERMANENT GUEST CELLS
The permanentguestcells are macrophages and mast cells.
Macrophages (histiocytes) are phagocytic cells derived from bone marrow monocytes, which can leave the bloodstream, enter tissues, and remain there for long periods. Macrophages are motile, (they can move within the tissue), are phagocytic, and are a source of metalloproteinases, which can break down ECM components They can process and present antigens to cells of the immune sys tem, either locally or by travelling to distant sites of immune cell accumulation. Tissue macrophages can resemble fibroblasts.
Copyright McGraw-Hill Companies. Used with permission.
Figure 1-2-2. Alveolar macrophage (arrow) is a second type of permanent guest cell in connective tissue
28 MEDICAL

Chapter 2 • Connective Tissue
Mast cells are closely related but not derived from blood basophils, and store inflammatorymediators such as histamine that have an early role in response to tissue injury, particularly immune mediated injury associated with immediate hypersensitivity reactions. IgE bound to the surface membrane ofthe mast cells mediates these reactions. Morphologically, mast cells contain large, membrane bound granules of their inflammatory mediators, which can best be visualized with special stains in the light microscope.
TRANSIENT CELLS
Transient cells migrate into connective tissue from the blood and include lym phocytes, plasma cells, neutrophils, eosinophils, basophils, and monocytes.
EXTRACELLULAR MATRIX
The extracellular matrix consists offibrillar proteins (collagen, elastin, fibrillin, fibronectin), proteoglycans that are associated with water and form a gel matrix, and glycoproteins that form structural proteins and include laminin, entactin, and tenascin.
Fibrillar proteins are derived from soluble precursors synthesized and secreted by support cells ofthe CT. The most abundantis collagen, butvarious connective tissues may also have a variable content of elastin and fibrillin, and fibronectin, which help to anchor cells to basal lamina.
Collagen is produced by fibroblasts and myofibroblasts. The initial collagen mol ecule is a triple helix ofchains, which are tightly bound and which exclude water from the helix (hydrophobic), thereby allowing very tight packing of the mol ecules. The molecule undergoes glycosylation and hydroxylation ofvarious ami no acids, resulting in procollagen. Procollagen is secreted into the extracellular space, where extracellular peptidases (also offibroblast origin) cleave off a por tion ofthe molecule toproducetropocollagen. Tropocollagen then selfassembles into larger fibrils, which are visible with the electron microscope. Depending on the type ofcollagen and the tissue, fibrils may assemble into even larger collagen fibers, which can be visible with the light microscope. Collagen provides tensile strength to tissue.
Clinical Correlate
lgE-sensitized mast cells degranulate during hypersensitivity reactions (asthma, hay fever, eczema). The release of histamine during asthma causes difficulty breathing.
MEDICAL 29


There are at least 25 different collagen chain types, and they can combine to pro duce at least 19 different collagens. Some form fibrils, others are associated with but are not the backbone of the fibrils, and yet others form a felt-like mesh rather than fibrils. An abbreviated list of the most important ones includes:
•Type I collagen is found in skin, tendon, ligaments, bone, and cornea. Most of the body's collagen is Type I.
Copyright McGraw-Hill Companies. Used with permission.
Figure 1-2-3. Collagen fibers with a banding pattern with repeating units of 64 nm in length.
•Type II collagen is found in cartilage, intervertebral discs, and vitreous body of the eye.
•Type III collagen is found in blood vessels, and forms reticular fibers in various organs and tissues.
-Links the basal lamina of cells to the underlyingECM in many tissues.
-Comprises the main supporting fibers in the ECM surrounding the
parenchymal cells of lymphoid (lymph node and spleen) organs, bone marrow, and liver
• Type IV collagen is found in the basal lamina.
Chapter 2 • Connective Tissue
Clinical Correlate
Type Ill is the first collagen type synthesized in wound healing, and is then replaced by type I.
MEDICAL 31
Section I • Histology and Cell Biology
Clinical Correlate
In Marfan syndrome, elastic tissue is weakened.
•Ocular defects include myopia and detached lens.
•Skeletal defects are long arms, legs, fingers, and scoliosis.
•Cardiovascular defects are mitral valve prolapse and dilated aorta.
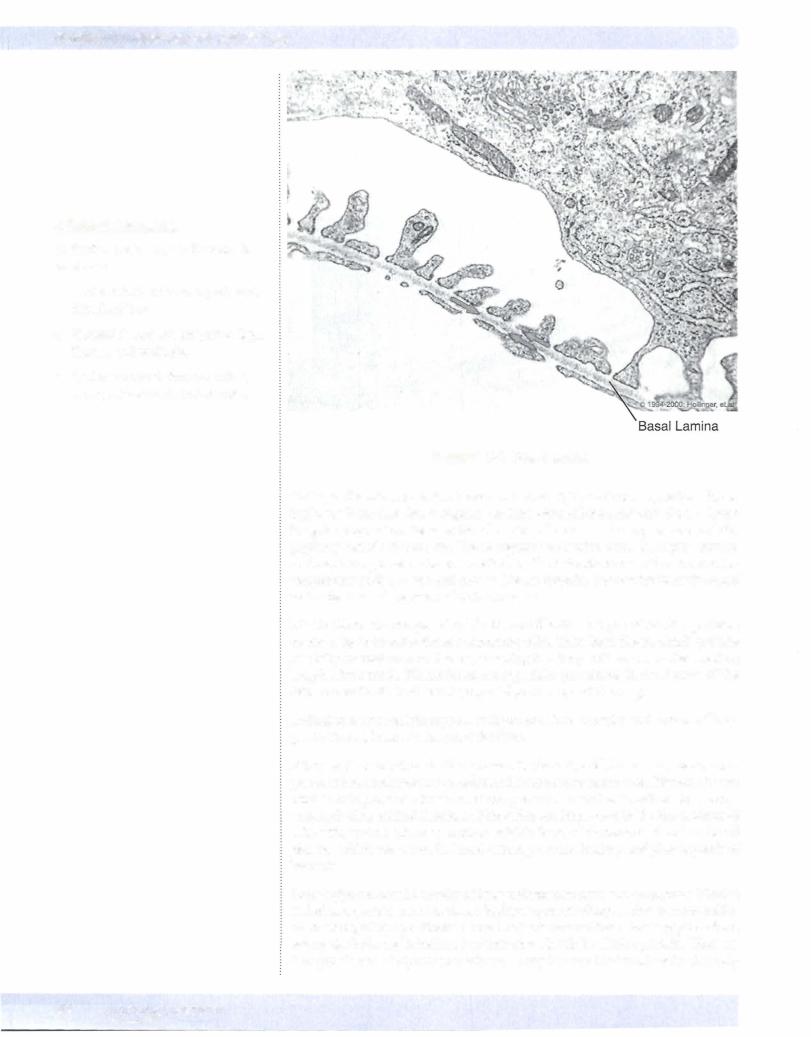
Figure 1-2-4. Basal lamina
Collagen fibers in connective tissue can have a highly variable disposition, form ing loose irregular, dense regular, or dense irregular connective tissue. Loose irregular connective tissue is found in the submucosa of many organs and the papillary dermis of the skin. Dense regular connective tissue is highly ordered and may be organized in larger parallel bundles in tendons or in other ordered ar rangements such as bone and cornea. Dense irregular connective tissue is found in the dermis and capsules of various organs.
Elastic fibers are composed of elastin and fibrillin, 2 types of fibrillar proteins secreted by connective tissue supporting cells,. They form fibers, which provide elasticity or resilience to tissues, meaning that they will return to their resting length after stretch. Elastic fibers are especially prominent in the dermis of the skin, the walls of blood vessels, especially arteries, and the lung.
Reticular fibers contain type III collagen and form capsules and stroma oflym phatic tissues, bone marrow, and the liver.
Fibronectin is another fibrillar protein in the extracellular matrix, again com prised ofinsoluble monomers secreted by connective tissue cells. Fibronectin can bind to collagen and other matrix components, as well as to cell-surface recep tors, including epithelial cells, and therefore are important in the interactions of cells with matrix. There is another soluble form of fibronectin found in blood plasma, which has a role in blood clotting, wound healing and phagocytosis of bacteria.
Proteoglycans consist mostly of long unbranched glycosaminoglycans (GAGs) linked to a protein core. GAGs are highly negatively charged, due to many sulfat ed residues, attract positively charged cations around them. Proteoglycans form aggregates by being linked to a hyaluronan molecule by a linker protein. There are 5 major classes of glycosaminoglycans. They include hyaluronic acid (the only
32 M EDICAL

one that does not form proteoglycans), chondroitin sulfate, dermatan sulfate, keratan sulfate and heparan sulfate. The major components ofECM include a gel formed by the interaction ofwater with proteoglycan aggregates. This gel resists compressive forces and provides a medium through which water soluble com pounds can diffuse such as between blood vessels and parenchymal cells, includ ing ions, nutrients, metabolites, growth factors, hormones, etc.
Glycoproteins have a relatively greater content of protein compared to proteo glycans. Laminin, entactin, and tenascin are non-filamentous structural glyco proteins in the ECM.
•Laminin is a component ofthe basement membrane of most epithelial and endothelial cells.
•Laminin binds integrins of the cell membrane and link the cell mem brane to the basal lamina via entactin, which links laminin to the type IV collagen of the basal lamina.
•Tenascin is another important adhesion molecule in the cell.
Ifthese 2 conditionsare notpresent,fibroblasts replacethe damaged parenchyma with scar tissue. Fibroblasts can be stimulated to proliferate and produce large amounts of extracellular collagen to fillin the defect. In either case, in regen eration or scar formation, macrophages clear away any debris of damaged cells and ECM components. Macrophages may already reside in the tissue or can be recruited from the blood stream. The recruitment, proliferation, and function of cells involved in wound healing is directed by the sequential expression and sup pression ofvarious growth factors and inflammatory mediators.
Chapter 2 • Connective Tissue
CUnical Correlate
If an organ is damaged, it may be able to restore itselfthrough regeneration totally or nearly to the state it was in prior to injury. Regeneration requires a resident population of parenchymal cells ableto replace lost ones, either stem cells or differentiated cells that still have the ability to proliferate.
Regeneration requires an intact underlying connective tissue support network, including an intact basal lamina, to guide the organization of newly formed parenchymal cells.
MEDICAL 33

Section I • Histology and Cell Biology
ChapterSummary
•Connective tissue (Cl) provides support for parenchymal cells (epithelial and other functional cell types) that carry out the specific tissue and organ functions.
•Connective tissue is comprised of support cells, guest cells, and their associated extracellular matrix (ECM) or ground substance. Support cells include fibroblasts, myofibroblasts, chondroblasts, osteoblasts and their derivatives, adipocytes. The permanent guest cells are macrophages and mast cells.
•The extracellular matrix consists offibrillar proteins (collagen, elastin, fibrillin, fibronectin), proteoglycans that are associated with water and form a gel matrix, and glycoproteins that form structural proteins and include laminin, entactin, and tenascin.
•Fibrillar proteins are mainly collagen, but various connective tissues may also have a variable content of elastin and fibrillin, and fibronectin, which help to anchor cells to basal lamina. Collagen is produced by fibroblasts and myofibroblasts.
•Type I collagen is found in skin, tendon, ligaments, bone, and cornea.
•Most of the body's collagen is type I. Type II collagen is found in cartilage,
intervertebral discs, and in vitreous body of the eye.
•Type Ill collagen is found in blood vessels, and it forms reticular fibers in various organs and tissues. It links the basal lamina ofcells to the underlying extracellular matrix in many tissues. Type Ill collagen comprises the main supporting fibers in the extracellular matrix surrounding the parenchymal cells of lymphoid (lymph node and spleen) organs, bone marrow, and liver.
•Type IV collagen is found in the basal lamina.
•Elastic fibers are composed of elastin and fibrillin and are especially prominent in the dermis ofthe skin, the walls of blood vessels, especially arteries, and the lun
•Fibronectin can bind to collagen and other matrix components, as well as to cell surface receptors, including epithelial cells, and therefore are important in the interactions of cells with matrix.
•Proteoglycans consist mostly of long unbranched glycosaminoglycans
(GAGs) linked to a protein core.
•Glycoproteins have a relatively greater content of protein compared to proteoglyc.ans. Laminin, entactin, and tenascin are non-filamentous structural glycoproteins in the ECM.
34 MEDICAL
