
- •Preface
- •Acknowledgments
- •Basic Physics
- •Transducers and Resolution
- •Doppler Physics
- •Artifacts
- •Summary
- •Introduction
- •Patient Preparation
- •Patient Positioning
- •Transducer Selection
- •Two-Dimensional Images
- •Two-Dimensional Imaging Controls
- •Introduction
- •M-Mode Echocardiography
- •Color-Flow Doppler
- •Spectral Doppler
- •Tissue Doppler Imaging
- •Measurement and Assessment of Two-Dimensional Images
- •Measurement and Assessment of M-Mode Images
- •Measurement and Assessment of Spectral Doppler Flow
- •Measurement and Assessment of Tissue Doppler Imaging
- •Evaluation of Color-Flow Doppler
- •Evaluation of Ventricular Function
- •Mitral Regurgitation
- •Aortic Regurgitation
- •Tricuspid Regurgitation
- •Pulmonary Regurgitation
- •Endocarditis
- •Pulmonary Hypertension
- •Systemic Hypertension
- •Hypertrophic Cardiomyopathy
- •Dynamic Right Ventricular Outflow Obstruction
- •Moderator Bands
- •Dilated Cardiomyopathy
- •Right Ventricular Cardiomyopathy
- •Restrictive Cardiomyopathy
- •Endocardial Fibroelastosis
- •Arrhythmogenic Right Ventricular Cardiomyopathy
- •Myocardial Infarction
- •Myocardial Contusions
- •Pericardial Effusion
- •Neoplasia as a Cause of Pericardial Effusion
- •Pericardial Disease
- •Abscesses
- •Pericardial Cysts
- •Thrombus
- •Ventricular Septal Defect
- •Patent Ductus Arteriosus
- •Aorticopulmonary Window
- •Right to Left Shunting PDA
- •Atrial Septal Defects
- •Endocardial Cushion Defects
- •Bubble Studies
- •Atrioventricular Valve Dysplasia
- •Outflow Obstructions
- •Inflow Obstructions
- •Tetralogy of Fallot
- •APPENDIX ONE Bovine
- •APPENDIX TWO Canine
- •APPENDIX THREE Equine
- •APPENDIX FOUR Feline
- •APPENDIX FIVE Miscellaneous Species
- •Index
CHAPTER EIGHT
Pericardial Disease, Effusions, and Masses
The reported causes of pericardial effusion (PE) in animals include pericardioperitoneal hernias, congestive heart failure, left atrial rupture, infection, neoplasia, trauma, and benign idiopathic causes (1–5). The pericardial effusion may lead to tamponade (6).
Feline infectious peritonitis (FIP) is the most common cause of pericardial effusion in the cat and is often accompanied by pleural effusion and ascites. Hypertrophic cardiomyopathy is the most frequent form of heart disease leading to pericardial effusion in cats (5). Other less-encountered forms of heart disease resulting in PE in the cat include dilated and restrictive cardiomyopathies, and mitral valve abnormalities (7,8).
Intrapericardial neoplasia, idiopathic hemorrhagic pericarditis, and left atrial rupture secondary to chronic mitral regurgitation are the most common causes of pericardial effusion in the dog, with intracardiac and pericardial tumors heading the list (9). Of these tumors, hemangiosarcoma, chemodectoma, and mesothelioma lead the list for highest incidence (10).
Pericardial Effusion
There is a high incidence of pericardial effusion in large breed dogs with the highest incidence seen in golden retrievers, German shepherd dogs, Saint Bernards, Labrador retrievers, and Newfoundlands (11–14). Most dogs that present with pericardial effusion with echocardiographic evidence of a mass are older (median age 9–11 years) than dogs that present without echocardiographic evidence of a mass (median age 7–9 years). The exception is the Saint Bernard, which presented at a much younger median age of 2.3 years (11). Congestive heart failure may also cause pericardial effusion in both dogs and cats, although the incidence is less common and the amount of effusion is typically small (1,5,11,15–19). Occasionally atrial rupture causes pericardial effusion in dogs (15).
Pericardial effusion in the cat is relatively rare. When present however, several studies have shown that congestive heart failure secondary to hypertrophic, restrictive, and unclassified cardiomyopathy are the most common underlying causes of pericardial effusion in cats (5,15,17,20,21). Feline infectious peritonitis, neoplasia, pericardial peritoneal diaphragmatic hernia, systemic infections, and uremia, are other reported causes of pericardial effusion in cats. Of these, neoplasia, primarily lymphoma, and adenocarcinoma and FIP are reported as the next most common causes of effusion in the cat (5,7,8,15–19,22–24).
Fibrinous pericarditis is the most common underlying etiology of pericardial effusion in the cow. Other causes of bovine pericardial effusion include cardiac lymphoma and effusion secondary to spread from systemic, pleural, and respiratory infection (25–27).
Echocardiographic Features of Pericardial Effusion
Echocardiography is the procedure of choice when trying to diagnose the presence or absence of
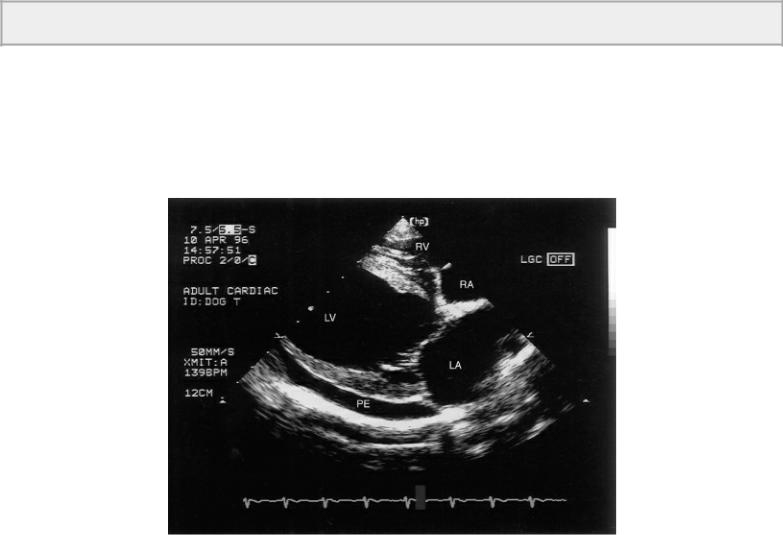
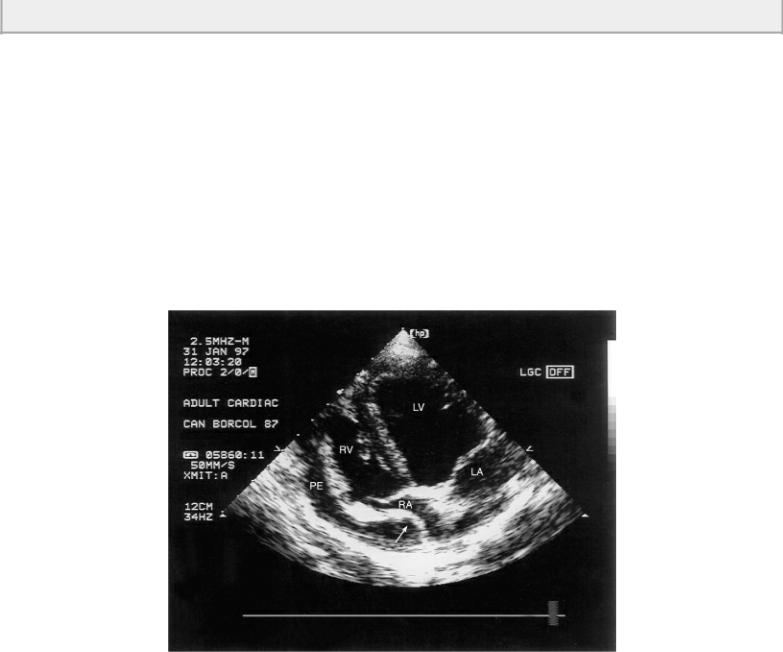
pericardial effusion (28). The echocardiographic features of pericardial effusion in all animals include the presence of an echo free or hypoechoic space between the epicardium and the pericardial sac, swinging motion of the heart when the amount of effusion is significant, and if tamponade is present, diastolic collapse of the right atrium or ventricle (3,5,28–30). Pericardial effusion is typically not seen behind the left and right atrium on echocardiographic images since the parietal and visceral pericardiums are more adherent to each other at the base of the heart (Figures 8.1, 8.2, 8.3, 8.4, 8.5). This helps differentiate pleural from pericardial effusions (31). The boundaries of pericardial effusion are typically smooth and conform to the shape of the heart while pleural effusion is seen as more irregular with ill-defined boundaries. In man, an echo-free space of less than 5 mm is considered to be a mild effusion, a space between 5 and 10 mm is moderate in amount, and an anechoic space of greater than 10 mm is classified as a severe amount of fluid accumulation (28).
Pericardial effusion is typically not seen at the heart base below the atria while pleural fluid is present.
Figure 8.1 An echo-free space below the left ventricular wall in this parasternal four-chamber view representative of pericardial effusion is seen in this dog with congestive heart failure. Notice that the pericardial fluid is not seen at the heart base and stops just beyond the atrial and ventricular junction. RV = right ventricle, RA = right atrium, LV = left ventricle, LA = left atrium, PE = pericardial effusion.
Figure 8.2 The large echo-free space of pericardial effusion surrounds the heart of this dog with idiopathic pericardial effusion. Notice that the fluid does not extend around the base of the heart and its boundaries are relatively smooth and circular. PE = pericardial effusion, RV = right ventricle, LV = left ventricle, LA = left atrium, RA = right atrium, plane = right parasternal four chamber.
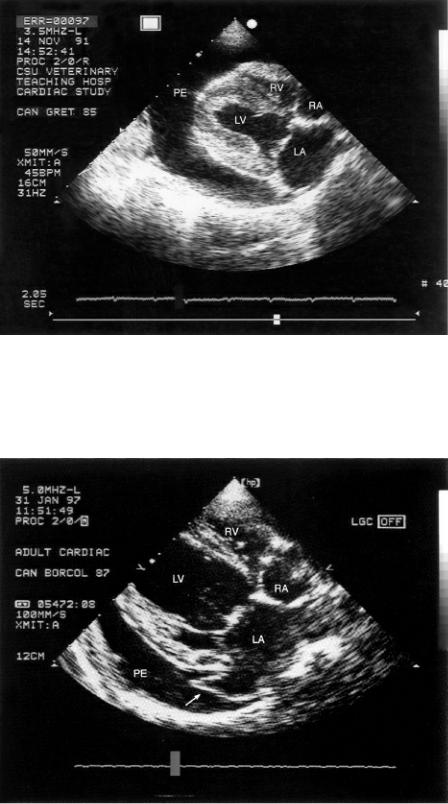
Figure 8.3 The left auricle is seen within the pericardial space in this dog with effusion (arrow). RV = right ventricle, LV = left ventricle, RA = right atrium, LA = left atrium, plane = right parasternal four chamber.
Figure 8.4 The left auricle may be seen within the pericardial fluid next to the left ventricle on transverse images. LAU = left auricle, PE = pericardial effusion, RV = right ventricle, LV = left ventricle, plane = right parasternal transverse view at the level of the chordae.
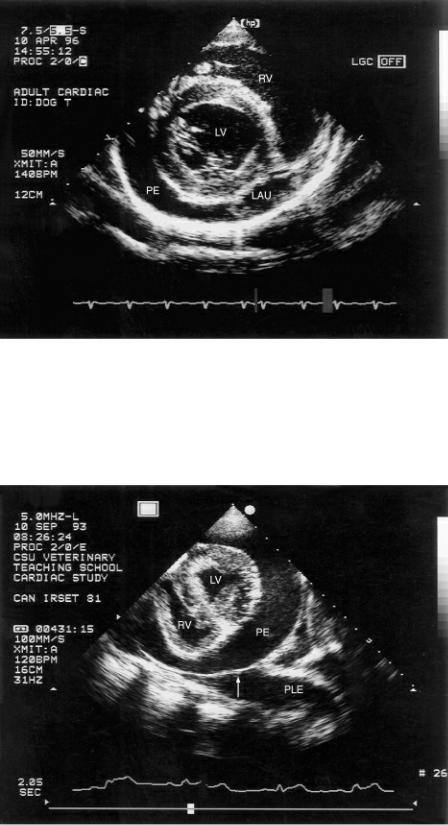
Figure 8.5 Pericardial and pleural effusion are seen surrounding this dog’s heart. The sac (arrow) is smooth and round while the pleural fluid space contains irregularities. PE = pericardial effusion, PLE pleural effusion, RV = right ventricle, LV = left ventricle, plane = left parasternal transverse left ventricle.
M-mode images show an echo-free space between the left ventricular wall and the pericardial sac (Figure 8.6). The epicardium on these images will be very bright simply because of the difference in acoustical impedance between the epicardium and fluid. When the fluid space is not seen during systolic contraction of the left ventricular chamber, the fluid accumulation is not clinically significant (28).
Figure 8.6 M-mode images show an echofree space between the left ventricular wall and the pericardial sac when pericardial effusion is present. RVW = right ventricular wall, PE = pericardial
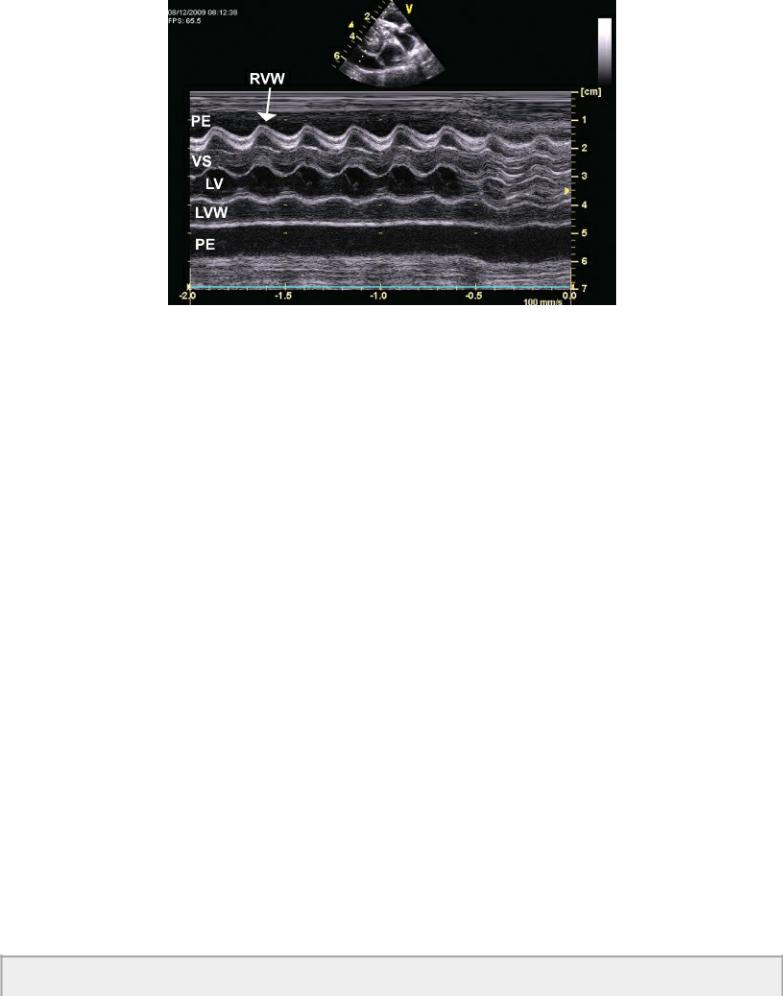
effusion, VS = ventricular septum, LV = left ventricle, LVW = left ventricular wall.
Large amounts of thoracic or mediastinal fat have sometimes been misdiagnosed as pericardial effusion, and care should be taken to set the gain correctly and to image multiple cardiac planes (31). The diagnosis of pericardial fat is typically made when an anechoic space is seen in the near field of the sector image, and although it may be present in the far field, it usually is not. Therefore, an echofree space in both the near field and far field usually supports the diagnosis of true pericardial effusion, but this is not foolproof as pericardial fat can occasionally be seen in both areas (28,32,33). Fat when present typically moves with the heart during contraction, and is somewhat echogenic, features that can help differentiate fat from pericardial effusion (28).
Cardiac Tamponade
Pericardial fluid accumulation that causes intrapericardial pressure to be higher than or equal to right ventricular pressure results in diastolic collapse of the right ventricle and atrium, decreased cardiac output, and signs of forward failure (21,34–36). The amount of pericardial fluid does not determine whether tamponade is present or not. Intrapericardial pressure is determined by pericardial compliance, the rate of fluid accumulation, and the amount of fluid accumulation (30). The compliance of the pericardial sac decreases with age, with chronic pericardial inflammation, and with pericardial neoplasia, so smaller amounts of fluid are needed to generate large amount of pressure on the cardiac chambers (30). Additionally a chronic slow-developing effusion is less likely to develop tamponade (3,21,37,38). Dogs that present with the clinical sign of collapse typically have tamponade and have a high incidence of being positive for the presence of cardiac neoplasia. The collapse is thought to occur because of a rapid accumulation of fluid secondary to the neoplastic lesion (14). Dogs that are diagnosed with idiopathic effusions tend to accumulate larger volumes of effusion before tamponade develops presumably because of the slow and chronic nature of fluid accumulation, which allows the pericardial sac to expand slowly, delaying the development of high pressure within the pericardial space (13). Signs of right heart failure including jugular distension and ascites instead of collapse typically suggest slow fluid accumulation (21,39).
The size of the effusion does not determine whether tamponade is present. Diastolic collapse of the right atrium and/or
ventricle confirms the presence of tamponade.
The diastolic collapse of the right ventricle secondary to tamponade is displayed on M-mode images as downward motion of the right ventricular wall during diastole. This is a sensitive and specific finding (28). When right ventricular hypertrophy is present, increased loading conditions prevent collapse of the right ventricular chamber even in the presence of high intrapericardial pressure (28,40). Abnormal diastolic downward motion of the right atrial wall is 100% sensitive for the presence of tamponade but is less specific (28). Left atrial collapse though not common is a very specific finding for tamponade in man after cardiac surgery (28).
Figure 8.7 Cardiac tamponade exists when there is diastolic collapse of the right ventricle and or atrium (arrow). RV = right ventricle, LV = left ventricle, PE = pericardial effusion, LA = left atrium, RA = right atrium, plane = left parasternal apical four chamber, species = canine.
Figure 8.8 The right atrial wall is collapsed into the chamber secondary to tamponade (small arrows). A mass is seen in the right atrial wall near the tricuspid annulus. PE = pericardial effusion, RV = right ventricle, TV = tricuspid valve, RA = right atrium, AO = aorta, LA = left atrium, plane = left cranial transverse view.

Two-dimensional imaging is superior to M-mode in identifying both pericardial effusion and the presence of tamponade. Real-time images will show the collapse of the right side of the heart. Right parasternal long-axis images may be used to view the collapse since the heart is displaced from the thoracic wall and right-sided structures are easier to visualize, but multiple planes should be interrogated for diagnostic accuracy and for identification of an underlying cause (Figures 8.7, 8.8) (21,28,39,41).
Tapping the pericardial fluid results in visibly increased chamber sizes (42). Rarely a sudden increase in venous return and volume overload of the heart resulting in acute pulmonary edema has been associated with pericardiocentesis in several animals and man (43,44).
There are reports of clinical signs related to cardiac tamponade without echocardiographic evidence of diastolic collapse of the right-sided chambers. This is seen when there is increased right-sided pressure secondary to other cardiac disease such as pulmonary hypertension, Tetralogy of Fallot, intracardiac tumors, and pulmonic stenosis (41,45). Cardiac tamponade has been reported in man secondary to large pleural effusion without the presence of pericardial effusion. Evidence of diastolic collapse on the right side of the heart is visible in these patients (46). Experimental models in man of pleural effusion with minimal pericardial effusion have shown that pleural effusion can cause echocardiographic signs of cardiac tamponade, with both right atrial and right ventricle diastolic collapse (47,48). Signs of tamponade have been reported in a dog with pleural effusion and no echocardiographic evidence of pericardial effusion or cardiac pathology (49).
Flow alterations with tamponade can be documented with spectral Doppler. Pulmonary artery and right ventricular inflow velocities increase with inspiration in the presence of tamponade. Flow velocities in the left side of the heart at the aorta and mitral valve decrease accordingly with inspiration (28). Vena caval flow into the right atrial chamber will show increases systolic velocities with inspiration and increased diastolic reversal of flow with expiration (28,50).
Cardiac Function with Pericardial Effusion
Pericardial fluid with or without tamponade reduces the amount of filling and output from the right side of the heart. This will reduce left-sided volume and output. Function is reduced when a significant volume of pericardial fluid is present, and the diagnosis of myocardial failure should wait until after resolution of the effusion. Often adequate assessment of function is not possible simply
