
- •Copyright
- •Contents
- •Dedication
- •Preface
- •Acknowledgments
- •Contributors
- •Contributors to the Previous Edition
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •IV. Hypertension
- •VI. Nephrotic Syndrome (NS)
- •VII. Hemolytic Uremic Syndrome (HUS)
- •VIII. Hereditary Renal Diseases
- •IX. Renal Tubular Acidosis (RTA)
- •XI. Chronic Kidney Disease (CKD) and End-Stage Renal Disease (ESRD)
- •XII. Structural and Urologic Abnormalities
- •XIII. Urolithiasis
- •XIV. Urinary Tract Infection (UTI)
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •IV. Food Allergy
- •VI. Urticaria (Hives)
- •VII. Drug Allergy
- •VIII. Asthma
- •IX. Immunology Overview
- •X. Disorders of Lymphocytes (Figure 15-2)
- •XI. Disorders of Granulocytes (Figure 15-3)
- •XII. Disorders of the Complement System
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Comprehensive Examination
- •Index
XI. Chronic Kidney Disease (CKD) and End-Stage Renal Disease (ESRD)
A.Etiology
1.The most common causes include glomerular diseases (e.g., FSGS), congenital or inherited kidney diseases (e.g., renal dysplasias or obstructive uropathies), reflux nephropathy, collagen vascular diseases, cystic kidney diseases, interstitial nephritis, and HUS.
2.The cause is unknown in up to 10% of cases.
3.Determining the cause of the child’s chronic kidney disease may have implications for the child and his or her family, especially important in cases of inherited disorders. Specific therapies may modify disease progression, some genetic diseases may occur in siblings or offspring, and some diseases may recur in transplanted kidneys.
B.Clinical features. Clinical findings may include short stature, anemia, failure to thrive, polyuria and polydipsia, lethargy, and rickets.
C.Evaluation
1.Investigation for the causes of CKD
2.Careful family history
3.Assessment of growth and nutrition
4.Evaluation for renal osteodystrophy (i.e., bone disease secondary to renal failure)
5.Serologic testing for collagen vascular diseases
6.Renal imaging to look for structural kidney abnormalities
7.Renal biopsy (in some cases)
D.Management
1.Medical
a.Nutritional management includes assurance of adequate caloric intake and avoidance of high phosphorus, high sodium, and high potassium foods. Patients are also given oral phosphate binders and vitamin D analogues to prevent renal osteodystrophy. Protein intake should be at the RDA for age.
b.Biochemical management includes monitoring and management of serum electrolytes, BUN, creatinine, calcium, and alkaline phosphatase.
c.Blood pressure monitoring and management are critical.
d.Anemia is treated with iron and recombinant erythropoietin therapy.
e.Growth is closely monitored, and patients may require recombinant human growth hormone if their growth fails to normalize with other medical interventions.
2.Dialysis is initiated or transplantation is considered when the glomerular filtration rate is <10% of normal, or earlier if the child is symptomatic.
a.Peritoneal dialysis is generally the preferred dialysis modality in infants and children.
b.Chronic hemodialysis may also be performed in children and requires vascular access via an indwelling catheter or an arteriovenous fistula. This is technically very difficult in an infant.
c.Kidney transplantation is the preferred treatment for children with ESRD.
1.Living related donors and living unrelated donors are preferred over deceased donors because of better kidney transplant outcomes. Graft outcome varies with donor source. Approximately 80% of living donor kidneys and 65% of deceased donor kidneys remain functioning 5 years after transplant.
2.Kidney transplantation requires lifelong immunosuppression with increased risks of infection and subsequent malignancies.
435
3.The most common causes of transplant loss include acute and chronic rejection, noncompliance with medications, technical problems during surgery, and recurrent disease.
436
XII. Structural and Urologic Abnormalities
A.Structural and urologic abnormalities are common, occurring in 6–10% of children.
B.Congenital obstructive abnormalities may occur at any level in the urinary tract. Bilateral lesions threaten renal function.
1.Ureteropelvic junction obstruction may occur as a result of kinks, fibrous bands, or overlying aberrant blood vessels.
2.Ureterovesical junction obstruction may occur as a result of ureterocele, primary megaureter, or abnormal insertion of the ureter into the bladder.
3.Bladder outlet obstruction may occur as a result of posterior urethral valves in males, may be secondary to polyps or tumors, and may be associated with prune belly syndrome (i.e., absence of rectus muscles, bladder outlet obstruction, and, in males, cryptorchidism). Bladder outlet obstruction is typically associated with impairment in renal function.
4.Any form of congenital obstruction, if severe in utero, may lead to abnormal renal development (renal dysplasia). Severe impairment of renal function from any in utero cause may lead to oligohydramnios, which results in pulmonary hypoplasia that may be incompatible with life.
C.Acquired obstruction may occur as the result of renal calculi [see section XIII], tumors, or strictures.
D.Renal abnormalities
1.Renal agenesis occurs as a result of the failure of development of the mesonephric duct or the metanephric blastema, and may be associated with severe congenital anomalies in other organ systems (e.g., heart and hearing).
a.Unilateral renal agenesis occurs in 0.1–0.2% of children.
b.Bilateral renal agenesis is very rare. Infants die in the perinatal period secondary to associated pulmonary hypoplasia.
2.Renal dysplasia is much more common than renal agenesis.
a.Pathologically, renal dysplasia is associated with altered structural organization of the kidney, ranging in severity from mild to severe.
b.Functionally, renal dysplasia is associated with concentrating defects, RTA, and varying degrees of decreased kidney function.
c.Patients with relatively mild renal dysplasia and its associated renal functional abnormalities at birth may experience improved kidney function in later infancy and childhood, only to deteriorate in late childhood or adolescence.
d.Severe renal dysplasia results in a nonfunctional kidney.
1.The most common abdominal mass discovered in newborns is the multicystic dysplastic kidney, which is usually associated with an atretic ureter.
2.If bilateral and severe, multicystic dysplastic kidneys are incompatible with life. These infants are usually born with the stigmata of Potter syndrome (see Chapter 5, section IV.I.6).
3.Other structural abnormalities include horseshoe kidney (fusion of the lower poles of the kidneys), renal ectopia (kidney located outside of the renal fossa, such as in the pelvis), and duplication anomalies.
E.Vesicoureteral reflux (VUR)
1.Definition. VUR is defined as urine refluxing from the urinary bladder into the ureters and the renal collecting system.
2.Epidemiology. It is estimated that at least 0.5% of healthy infants have some degree of
437
VUR.
3.Etiology
a.VUR is caused by abnormalities of the ureterovesical junction, most commonly a short submucosal tunnel in which the ureter inserts through the bladder wall. It also is associated with dysfunctional voiding patterns in infants and children.
b.VUR has been described to have multiple inheritance patterns, including autosomal dominant inheritance with variable expression, autosomal recessive, or X-linked inheritance.
4.Classification. VUR is graded from grade 1 to grade 5 (Figure 11-4).
5.Clinical features
a.Most children with lower grades of VUR eventually have spontaneous resolution of the reflux.
b.VUR may predispose to episodes of pyelonephritis, and severe pyelonephritis in turn may lead to renal scarring, especially in infants and young children.
c.Severe in utero VUR may lead to renal hypoplasia/dysplasia and compromised kidney function.
d.Reflux nephropathy is the pathologic entity resulting from severe VUR. Kidneys show segmental scars, contraction, and interstitial nephritis, and this may lead to ESRD and hypertension.
6.Diagnosis. VUR is diagnosed by voiding cystourethrogram (VCUG) in which contrast is introduced into the urinary bladder via a urinary catheter. The bladder and kidneys are imaged under fluoroscopy during filling of the bladder and during voiding.
7.Management
a.Low-dose prophylactic antibiotics were previously routinely prescribed to reduce the incidence of UTI until the child outgrew the VUR. However, more recent studies have suggested that the benefits of prophylactic antibiotics may not outweigh the risks, especially in older children with low-grade VUR. The infant with high-grade VUR (e.g., grades 4 or 5) and a history of febrile UTI is still a candidate for prophylactic antibiotic therapy and close follow-up.
b.Children with grade 4 or 5 reflux should be referred to a pediatric urologist for consideration of surgical reimplantation of the ureters.
438
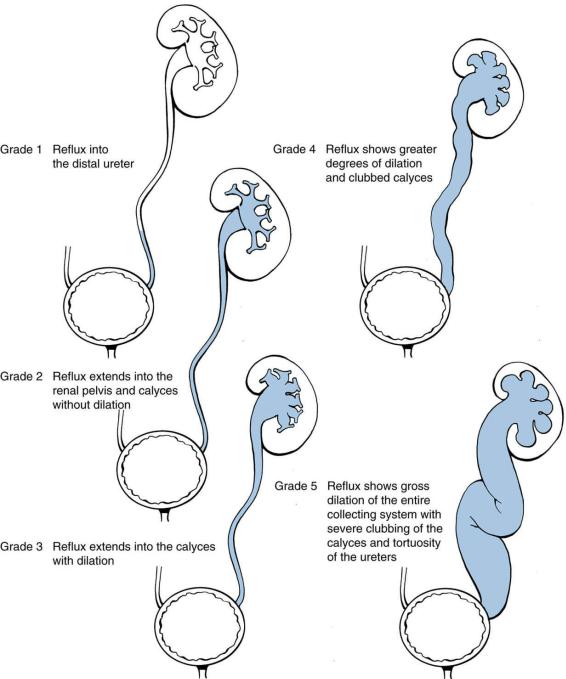
FIGURE 11-4 Classification of vesicoureteral reflux.
439
