
- •Copyright
- •Contents
- •Dedication
- •Preface
- •Acknowledgments
- •Contributors
- •Contributors to the Previous Edition
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •IV. Hypertension
- •VI. Nephrotic Syndrome (NS)
- •VII. Hemolytic Uremic Syndrome (HUS)
- •VIII. Hereditary Renal Diseases
- •IX. Renal Tubular Acidosis (RTA)
- •XI. Chronic Kidney Disease (CKD) and End-Stage Renal Disease (ESRD)
- •XII. Structural and Urologic Abnormalities
- •XIII. Urolithiasis
- •XIV. Urinary Tract Infection (UTI)
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •IV. Food Allergy
- •VI. Urticaria (Hives)
- •VII. Drug Allergy
- •VIII. Asthma
- •IX. Immunology Overview
- •X. Disorders of Lymphocytes (Figure 15-2)
- •XI. Disorders of Granulocytes (Figure 15-3)
- •XII. Disorders of the Complement System
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Comprehensive Examination
- •Index
Review Test
1.You are called to the newborn nursery to evaluate a 2-hour-old newborn who has suddenly become cyanotic. The oxygen saturation on room air is 69%, and the patient is tachycardic and tachypneic. Oxygen is administered without improvement in the patient’s oxygen saturation. On examination, you hear a loud S2 and no murmur. A chest radiograph shows increased pulmonary vascular markings, a narrow mediastinum, and a small heart. Which of the following would be the next step in management?
A.Start digoxin.
B.Refer the patient to surgery for placement of a Blalock–Taussig shunt.
C.Refer the patient to surgery for repair of a ventricular septal defect.
D.Proceed with pulmonary balloon valvuloplasty.
E.Begin infusion of prostaglandin E (PGE).
2.A 20-month-old boy with tetralogy of Fallot is admitted for evaluation of cyanosis that is increasing in frequency. As you conclude your history and physical examination, you witness an episode of cyanosis when the patient’s brother makes him cry. As the crying increases, the patient becomes more and more cyanotic. On examination, his cardiac murmur is now much softer than before he began crying. What is the next most appropriate step in management?
A.Intubate and begin mechanical ventilation.
B.Administer intravenous dopamine.
C.Place the patient in a knee-chest position.
D.Administer subcutaneous epinephrine.
E.Call for a cardiology consult.
3.A 10-year-old girl is seen for a routine health maintenance evaluation. Five years ago, she underwent surgical repair of coarctation of the aorta. On examination, the blood pressure in her right arm is 173/81 mm Hg, and her oxygen saturation is 97% in room air. Auscultation reveals a systolic ejection murmur audible throughout the precordium. The patient is otherwise asymptomatic. Which of the following would be the most appropriate next step in management?
A.Check the blood pressure in all extremities.
B.Refer the patient to a cardiac surgeon promptly.
C.Obtain an echocardiogram to rule out a bicuspid aortic valve.
D.Recheck the oxygen saturation in 100% oxygen.
E.Have the patient return in 6 months for reevaluation.
4.A 7-year-old boy presents with a 3-day history of fever (temperature to 39.7°C [103.5°F]), shortness of breath, and weakness. He also complains of chest pain, which is most intense when he lies down and improves when he sits upright. His past medical history is significant for closure of a ventricular septal defect 2 weeks ago. Which of the following findings is consistent with the most likely diagnosis?
A.Splinter hemorrhages
B.Pulsus paradoxus
C.Heart rate of 260 beats/minute with absent P waves
D.Prolongation of his QT interval
E.Tenderness at two of his costochondral joints
5.A 1-month-old female infant is seen in your office for a routine health maintenance evaluation. On examination, you hear a grade 4 holosystolic murmur at the left sternal border. Femoral pulses and oxygen saturation in room air are normal. The infant is otherwise well and growing normally. Which of the following statements regarding this patient’s condition is correct?
328
A.Without intervention, congestive heart failure will develop.
B.Eisenmenger syndrome will eventually occur.
C.Surgical closure of the patent ductus arteriosus is indicated.
D.The murmur may disappear without intervention.
E.Balloon valvuloplasty is indicated.
6.You are called to the nursery to evaluate a male newborn with cyanosis. On auscultation, you hear a single S2 but no murmur. Pulse oximetry shows an oxygen saturation of 72% in room air. An electrocardiogram reveals left axis deviation and left ventricular hypertrophy. What is his likely diagnosis?
A.Tetralogy of Fallot
B.Transposition of the great arteries
C.Truncus arteriosus
D.Total anomalous pulmonary venous return
E.Tricuspid atresia with intact ventricular septum
7.A 4-year-old boy is in the office for a routine health maintenance evaluation. His examination is normal except for multiple deep dental cavities. You plan on referring him for dental evaluation and possible dental extraction. His mother reminds you that he has a “heart condition.” Which of the following cardiac conditions requires antibiotic prophylaxis against endocarditis?
A.Patch repair of ventricular septal defect repaired 4 months ago
B.History of uncomplicated Kawasaki disease
C.Wolff–Parkinson–White syndrome
D.Patent ductus arteriosus
E.Ostium secundum atrial septal defect
8.You see a 7-week-old male infant with cough and poor feeding. Examination reveals a respiratory rate of 72 breaths/minute and a heart rate of 170 beats/minute. His weight is
7 pounds 6 oz, just 2 oz more than his birth weight. You hear diffuse rales throughout the lung fields and a systolic murmur on auscultation. The liver is 4 cm below the right costal margin. Which of the following conditions is the most likely cause of his signs and symptoms?
A.Large ventricular septal defect
B.Ostium secundum atrial septal defect
C.Small patent ductus arteriosus
D.Critical or severe aortic stenosis
E.Mild to moderate pulmonary stenosis
9.A thin 5-year-old boy presents for a routine health maintenance evaluation. He feels well and is growing normally. On examination, you hear a continuous murmur below the right midclavicle. The murmur is loudest while the patient is sitting and disappears while he is supine. The femoral pulses are normal. Which of the following conditions is the most likely diagnosis?
A.Aortic stenosis with regurgitation
B.Venous hum
C.Patent ductus arteriosus
D.Still’s murmur
E.Pulmonic systolic murmur
10.A 15-year-old boy complaints of chest pain that occurs during basketball practice. He is otherwise healthy and has no history of cardiac problems. Examination is normal except for a harsh systolic ejection murmur at the apex that worsens with standing and the Valsalva maneuver. An electrocardiogram demonstrates left ventricular hypertrophy and left axis deviation. Which of the following is the most appropriate initial management at this time regarding the likely diagnosis?
329
A.Start propranolol to reduce left ventricular outflow tract obstruction.
B.Admit for urgent aortic balloon valvuloplasty.
C.Reassure the patient that the murmur is innocent and allow complete athletic participation.
D.Admit for surgical myomectomy for septal hypertrophy.
E.Begin albuterol, as the patient’s chest pain is likely caused by asthma.
The response options for statements 11–13 are the same. You will be required to select one answer for each statement in the set.
A.Sinus tachycardia
B.Supraventricular tachycardia
C.Third-degree atrioventricular (AV) heart block
D.Wolff–Parkinson–White syndrome
E.Second-degree AV heart block, Wenckebach type
F.Prolonged QT syndrome
G.First-degree AV heart block
For each patient, select the most likely associated heart rhythm abnormality.
1.A female newborn is born to a mother with systemic lupus erythematosus.
2.A 10-year-old girl has congenital deafness.
3.A 5-year-old boy has an electrocardiogram that demonstrates a slurred upslope of the QRS complex.
The response options for statements 14–17 are the same. You will be required to select one answer for each statement in the set.
A.Tetralogy of Fallot
B.Truncus arteriosus
C.Transposition of the great arteries
D.Total anomalous pulmonary venous return with supracardiac drainage
E.Tricuspid atresia with ventricular septal defect
For each clinical description, select the cyanotic congenital heart disease lesion.
1.A male newborn has cyanosis and no heart murmur on auscultation.
2.When a 4-year-old boy with cyanosis squats, his cyanosis improves.
3.A male newborn with cyanosis has an electrocardiogram that demonstrates left ventricular hypertrophy.
4.An 8-year-old boy has a chest radiograph that shows cardiomegaly with a “snowman” appearance.
330
Answers and Explanations
1.The answer is E [IV.C.4]. This patient’s clinical presentation and physical examination are most consistent with transposition of the great arteries (TGA). Because the pulmonary and systemic circulations are in parallel, rather than in series, blood must be shunted from one circulation to the other for survival, either by a patent ductus arteriosus or by a patent foramen ovale. Intravenous prostaglandin E (PGE) helps keep the ductus patent, which improves oxygen saturation. In some cases, a balloon atrial septostomy will be indicated. This patient’s presentation is not consistent with a ventricular septal defect. Neither digoxin, pulmonary balloon valvuloplasty, nor a Blalock–Taussig shunt is indicated in the management of a patient with TGA.
2.The answer is C [IV.B.3.c and Table 8-5]. Tetralogy of Fallot (hypercyanotic or “tet”) spells are defined as paroxysmal episodes of hyperpnea, irritability, and prolonged crying that result in increasing cyanosis and decreasing intensity of the heart murmur. This condition is often triggered by crying. Initial management is to increase systemic vascular resistance by placing the patient in a knee-chest position. Other therapeutic modalities include the administration of morphine sulfate, sodium bicarbonate, and intravenous fluids and the use of oxygen. Mechanical ventilation in combination with general anesthesia may be effective but would only be used when other management options fail to reverse the cyanosis. Dopamine and epinephrine are contraindicated because they may worsen the spell. A cardiology consultation may be useful, but the acuity of the patient’s clinical presentation requires immediate intervention.
3.The answer is A [III.F.3.b]. Restenosis is a known complication from repair of coarctation of the aorta, and these clinical features are consistent with restenosis. Patients with coarctation of the aorta classically present with hypertension in the right arm, and commonly in the left arm, and reduced blood pressures in the lower extremities. Therefore, the most appropriate initial step in this patient would be to obtain blood pressures in all four extremities. Balloon angioplasty with or without endovascular stenting is the treatment of choice for restenosis, rather than surgical repair, after the patient undergoes a complete evaluation. Confirmation of a bicuspid aortic valve is important because it may accompany coarctation in up to half of patients; however, it is not the most appropriate initial step in this patient’s management. The oxygen saturation is normal in room air and therefore does not require reassessment in 100% oxygen. Given the significantly elevated blood pressure, it is not appropriate to wait 6 months for reevaluation.
4.The answer is B [V.D.2.c, V.D.4]. This patient’s clinical presentation is most consistent with pericarditis. The likely cause of his pericarditis is postpericardiotomy syndrome, given the recent closure of his ventricular septal defect before the onset of his symptoms.
Postpericardiotomy syndrome is believed to be an autoimmune response to a concomitant viral infection and is associated with opening of the pericardium during cardiac surgery. Pulsus paradoxus, or a greater-than-10 mm Hg drop in systolic blood pressure on deep inspiration, is found in patients with pericarditis. Splinter hemorrhages are noted in patients with endocarditis, which is also associated with fever. Supraventricular tachycardia, which would present as a rapid heart rate with absent P waves on electrocardiogram, may cause chest pain, but the pain would not change with position and fever would be absent. Prolonged QT syndrome is most often associated with syncope and sudden cardiac arrest. Costochondritis is a common cause of chest pain, but fever is not associated with this diagnosis.
5.The answer is D [III.D.3]. This patient’s murmur is consistent with a small ventricular septal defect (VSD). With a small VSD, a patient is likely to remain asymptomatic with normal
331
growth and development. Typically, the smaller the VSD, the louder the murmur. Small muscular or membranous VSDs may close on their own without intervention. Small VSDs do not generally result in congestive heart failure or in Eisenmenger syndrome. A patent ductus arteriosus would more commonly present with a machinery-like continuous murmur at the upper left sternal border. Balloon valvuloplasty is not indicated for a VSD.
6.The answer is E [IV.D.3 and Table 8-4]. Tricuspid atresia is the only cause of cyanosis in the newborn period that manifests with left axis deviation and left ventricular hypertrophy on electrocardiogram (ECG). Patients with tricuspid atresia without a ventricular septal defect have a single S2 as a result of the usual coexistence of pulmonary atresia and do not have a murmur. Patients with tetralogy of Fallot present with a systolic murmur of pulmonary stenosis and right ventricular hypertrophy (RVH) on ECG. Patients with transposition of the great arteries also have no murmur and a single S2 but will have RVH on ECG. Similarly, RVH is present in total anomalous pulmonary venous return, along with a systolic murmur. Truncus arteriosus manifests as combined ventricular hypertrophy with both a systolic and diastolic murmur.
7.The answer is A [V.C.8]. Before any invasive procedures that may result in bacteremia, prophylaxis against bacterial endocarditis is required for any patient who had structural heart disease repaired within the past 6 months. Patients with uncomplicated Kawasaki disease and cardiac dysrhythmias, including Wolff–Parkinson–White syndrome, or with acyanotic structural heart defects, such as patent ductus arteriosus, do not require antibiotic prophylaxis.
8.The answer is A [I.C.1.a]. This patient’s signs and symptoms are consistent with congestive heart failure (CHF). Forms of congenital heart disease that increase pulmonary blood flow, obstruct outflow, or overload portions of the heart through valvular regurgitation are among the many causes of CHF. Of the choices listed, only a large ventricular septal defect, which has a large left-to-right shunt with increased pulmonary blood blow, would cause CHF in a child of this age. Atrial septal defects, small patent ductus arteriosus defects, and mild to moderate pulmonary stenosis do not typically cause CHF. Critical or severe aortic stenosis may cause CHF, but this usually occurs within 24 hours of birth.
9.The answer is B [Table 8-1]. This murmur is most consistent with a venous hum, an innocent heart murmur. Aortic stenosis with regurgitation presents with systolic ejection and decrescendo diastolic murmurs. The murmur of a patent ductus arteriosus (PDA) is generally continuous and machinery-like and does not vary with position. Patients with PDAs generally also have brisk pulses. Both a Still’s murmur and a pulmonic systolic murmur are innocent systolic murmurs. A Still’s murmur is usually a grade 1–3 systolic murmur best heard at the mid-left sternal border. A pulmonic systolic murmur is a grade 1–2 high-pitched systolic
murmur best heard at the upper left sternal border. Both the Still’s murmur and the pulmonic systolic murmur are loudest supine.
10.The answer is A [V.F.3]. This patient’s presentation, including the heart murmur and electrocardiogram findings, is consistent with hypertrophic cardiomyopathy. Initial management typically includes medications, such as β-adrenergic blockers or calcium-channel blockers, to reduce the left ventricular outflow tract obstruction and improve ventricular compliance. Aortic balloon valvuloplasty is a treatment for aortic stenosis. In aortic stenosis, the murmur would not be expected to increase with the Valsalva maneuver or with standing. Patients with hypertrophic cardiomyopathy are at risk for sudden death and should be restricted from athletic participation. Myomectomy is recommended for severe obstruction refractory to medical management. Albuterol is a β2-agonist and is contraindicated in hypertrophic cardiomyopathy.
11.The answers are C, F, and D, respectively [VI.A–VI.C]. Congenital third-degree atrioventricular block is a complete heart block, with no conduction of atrial impulses to the ventricles. It is associated with infants born to mothers with systemic lupus erythematosus.
332
Long QT interval is a lengthening of the QT interval, which increases the risk of lethal ventricular arrhythmias. There are two inherited forms of the disorder, one associated with congenital deafness (autosomal recessive Jervell–Lange-Nielsen syndrome) and one not associated with congenital deafness (autosomal dominant Romano–Ward syndrome). Wolff– Parkinson–White syndrome is a form of supraventricular tachycardia that is identified by the presence of a delta wave (slurred upslope of the QRS complex) on electrocardiogram.
12.The answers are C, A, E, and D, respectively [IV.B–IV.D, IV.F, and Table 8-4]. Transposition of the great arteries presents with no murmur and a single S2 on auscultation. Squatting, or knee-chest positioning, increases systemic vascular resistance, which decreases the right-to-left shunt through a ventricular septal defect in tetralogy of Fallot. It is usually the first maneuver attempted to resolve a “tet” or hypercyanotic spell. Tricuspid atresia is the only cyanotic congenital heart disease lesion that manifests left ventricular hypertrophy on electrocardiogram in the newborn period. The classic chest radiograph in older children with unrepaired total anomalous pulmonary venous return and with supracardiac drainage is cardiomegaly with a “snowman” appearance.
333

C H A P T E R 9
334

Pulmonology
Lauren J. Witcoff
335
I.Anatomy and Physiology of the Respiratory System
A.Development
1.By 16 weeks’ gestation, the bronchial tree has developed. By 26–28 weeks’ gestation, sufficient air sacs and pulmonary vasculature have developed so that the fetus is able to survive.
2.Alveolarization begins around 36 weeks’ gestational age with most alveoli forming during the first few years of life, followed by a slower rate later in childhood and continuing through adolescence.
B.Anatomy
1.The right lung contains three lobes, and the left lung contains two lobes, plus the lingula.
2.Infants are at higher risk for respiratory insufficiency than older children and adults because infants have anatomically smaller air passages, less compliant (stiffer) lungs with a more compliant chest wall, and less efficient pulmonary mechanics.
3.The cricoid cartilage ring is the narrowest part of pediatric airway, predisposing to upper airway obstruction with any inflammation or narrowing. A small incremental decrease in lumen diameter in infants and small children can be critical, resulting in a large increase in airway resistance and increased work of breathing.
4.Congenital malformations of the respiratory tract may be associated with other congenital anomalies, especially of the cardiovascular system.
C.Physiology
1.Pulmonary vascular resistance decreases after birth when the fetal pulmonary and systemic circulations separate and the lungs ventilate for the first time.
2.The primary function of the lungs is gas exchange.
3.Lung disorders may be classified as obstructive or restrictive.
a.Obstructive defects are secondary to decreased airflow through narrowed airways. Examples include asthma, bronchiolitis, and foreign body aspiration.
b.Restrictive defects are secondary to processes that decrease lung volume (the amount of air filling the alveoli). Examples include pulmonary edema, scoliosis, pulmonary fibrosis, and respiratory muscle weakness.
4.During normal respiration, the extrathoracic upper airway narrows during inspiration and the intrathoracic lower airways narrow during expiration.
336
II.Clinical Assessment of Pulmonary Disease
A.History is most important in determining the diagnosis of pulmonary disorders.
1.The antenatal, prenatal, and neonatal histories are very important because complications of pregnancy, fetal or postnatal tobacco exposure, prematurity, and airway instrumentation can predispose to pulmonary problems.
2.Past medical history should include previous respiratory problems, including frequent respiratory tract infections, cough, wheeze, stridor, snoring, and exercise intolerance.
3.Review of systems should include documentation of atopy (asthma), failure to thrive or steatorrhea (cystic fibrosis), choking (aspiration), and recurrent infections (immunodeficiencies).
4.Family history should include assessment for genetic diseases (e.g., cystic fibrosis, asthma).
5.Environmental history is extremely important because fumes, strong odors, tobacco smoke, allergens, animals, and day care attendance may cause or exacerbate pulmonary disease.
B.Physical examination should emphasize the chest and respiratory system.
1.In the general assessment, assess for evidence of increased work of breathing, such as tachypnea, nasal flaring, expiratory grunting, and chest wall retractions.
2.Evaluate the ears, nose, and throat for signs of obstruction, atopy, or infection.
3.Perform a chest examination.
a.Inspiratory stridor suggests extrathoracic obstruction, such as in croup and laryngomalacia (softening and weakness of laryngeal cartilage during the first year of life, in which the cartilage collapses into the airway, especially when in the supine position).
b.Expiratory wheezing suggests intrathoracic obstruction, such as in asthma and bronchiolitis.
c.Crackles or rales suggest parenchymal disease, such as in pneumonia and pulmonary edema.
d.Prolonged expiratory phase and/or a hyperinflated thorax suggest obstructive disease.
e.Rapid, shallow breathing and/or a small thorax suggest restrictive disease.
4.Assess for related findings in other organs, such as heart murmurs, a prominent second heart sound (suggests elevated pulmonary artery pressure), eczema, and digital clubbing.
C.Accessory tests help to evaluate pulmonary function.
1.Imaging studies may include chest radiograph (CXR), computed tomography (CT) scan, magnetic resonance imaging (MRI), and nuclear studies (e.g., ventilation–perfusion scans). Ultrasound is helpful to localize pleural effusions.
2.Arterial blood gas (ABG) is the gold standard to measure oxygenation (PO2) and ventilation (PCO2).
3.Pulse oximetry noninvasively measures oxygen saturation (SpO2).
4.Pulmonary function testing (PFT) helps determine the type and severity of pulmonary dysfunction. The most common PFTs measure airflow as a function of time (spirometry) and lung volumes (plethysmography).
D.Laryngoscopy and bronchoscopy are performed in some conditions to visualize the upper and lower airways and/or to obtain bronchoalveolar lavage specimens for laboratory analysis. Common indications include persistent or recurrent cough, stridor, wheezing, and pulmonary infiltrates.
337
338
III.Infectious Disorders of the Respiratory Tract
A.Epiglottitis (supraglottitis)
1.Definition. Epiglottitis is bacterial cellulitis of the supraglottic structures: epiglottis, arytenoids, and aryepiglottic folds.
2.Epidemiology. The disorder is most common in children 2–7 years of age, with equal incidence in males and females.
3.Etiology
a.Infection with Haemophilus influenzae type b (HIB) was the most common cause before HIB immunization. Epiglottitis is now rare because of the success of the HIB immunization program.
b.Group A β-hemolytic streptococcus, Streptococcus pneumoniae, and Staphylococcus species may also cause epiglottitis.
4.Clinical features
a.Abrupt onset of rapidly progressive upper airway obstruction without a prodrome. The following signs and symptoms may occur:
1.High fever and toxic appearance
2.Muffled speech and quiet stridor
3.Dysphagia with drooling
4.Sitting forward in tripod position with neck hyperextension
b.Complete airway obstruction with respiratory arrest may occur suddenly.
c.Laboratory studies demonstrate leukocytosis with left shift. Ninety percent of patients have a positive blood culture, if the epiglottitis is secondary to HIB.
d.Epiglottis appears like a “thumbprint” on a lateral radiograph of the neck.
5.Differential diagnosis. Croup, bacterial tracheitis, and retropharyngeal abscess are diagnoses to also consider. Table 9-1 compares the clinical features that differentiate supraglottic disorders (e.g., epiglottitis) from subglottic disorders (e.g., viral croup).
6.Diagnosis. Epiglottitis should be suspected on the basis of clinical features. Visualization of a cherry red swollen epiglottis is made when the airway is established.
7.Management
a.Epiglottitis is a medical emergency.
b.Controlled nasotracheal intubation should be performed by experienced personnel in a controlled environment (e.g., operating room).
c.Before intubation, minimize stimulation while offering humidified oxygen. Avoid causing distress or examining the throat with a tongue depressor, as this may cause sudden respiratory arrest.
d.Intravenous antibiotic therapy typically includes a secondor third-generation intravenous cephalosporin to cover HIB and Streptococcus. If epiglottitis is secondary to HIB, rifampin prophylaxis is indicated for unimmunized household contacts younger than 4 years of age.
B.Laryngotracheobronchitis (croup)
1.Definition. Croup syndromes include viral croup and spasmodic croup and are secondary to mucosal inflammation and edema of the subglottic larynx, trachea, and bronchi.
2.Epidemiology
a.Viral croup is the most common cause of stridor. It typically occurs in children
6 months of age to 4 years of age in the late fall and winter. The male to female ratio is 2:1.
b.Spasmodic croup occurs year round in preschool age children.
339
3.Etiology
a.Viral croup is most commonly secondary to parainfluenza viruses. It may be recurrent owing to lack of complete immunity after initial infection, and because it can be caused by a variety of viruses in addition to parainfluenza.
b.The cause of spasmodic croup is unknown but possibly secondary to a hypersensitivity reaction.
4.Clinical features
a.Viral croup
1.Begins with an upper respiratory infection prodrome for 2–3 days, followed by stridor and cough.
2.Symptoms include inspiratory stridor, fever, barky cough, and hoarse voice, which typically last 3–7 days. Respiratory distress may occur.
3.Stridor and cough worsen at night and with agitation.
4.Wheezing may occur if the lower respiratory tract is involved.
5.Anterior–posterior radiograph of the neck demonstrates the “steeple sign” of subglottic narrowing.
b.Spasmodic croup
1.Characteristic acute onset of stridor without fever or other symptoms usually occurs at night.
2.Spasmodic croup typically recurs and resolves without treatment.
5.Diagnosis. Croup should be suspected on the basis of clinical features.
6.Management
a.Supportive care may involve hydration, antipyretics, and possibly oxygen, in addition to avoiding agitation. Improvement has been anecdotally noted when patients are exposed to humidified air, although use of cool mist or steam has not been proven efficacious.
b.A single dose of systemic corticosteroids, such as oral or intramuscular dexamethasone, has been shown to reduce croup severity and duration.
c.Children with respiratory distress get transient improvement from racemic epinephrine aerosols, which vasoconstrict subglottic tissues.
d.Hospitalization is indicated for children in respiratory distress.
C.Bacterial tracheitis is an uncommon, but re-emerging, cause of stridor.
1.Definition. Bacterial tracheitis is acute infectious inflammation of the trachea.
2.Etiology. Causes include Staphylococcus aureus (60%), Streptococcus, Haemophilus influenzae, and Moraxella catarrhalis.
3.Clinical features
a.Abrupt deterioration
b.Toxicity, high fever, stridor, brassy cough, choking, and acute respiratory distress secondary to mucus and pus in the trachea
4.Management. Bronchoscopy can be both diagnostic and therapeutic to remove secretions and sloughed tissue from the trachea. Appropriate antistaphylococcal antibiotics and airway support are indicated.
D.Pertussis. This highly contagious respiratory infection is also known as “whooping cough.”
1.Etiology. Bordetella pertussis is the major pathogen responsible for infection. Bordetella parapertussis causes illness that appears clinically very similar to pertussis.
2.Epidemiology and pathophysiology
a.Adolescents and adults whose immunity has waned are the major source for pertussis infection of unimmunized or underimmunized children.
b.Sneezed or coughed droplets are inhaled into airways of close contacts. A toxin is subsequently produced, which damages respiratory cells and enters the
340
bloodstream.
c.Infants younger than 6 months of age are most at risk for severe disease.
d.Routine immunization beginning at 2 months of age has been effective in reducing the overall incidence of pertussis infection (see Chapter 1, section III.C.2).
3.Clinical features
a.The incubation period is typically 7–10 days.
b.Pertussis is characterized by three stages.
1.Catarrhal stage (1–2 weeks) is characterized by upper respiratory symptoms such as rhinorrhea, nasal congestion, conjunctival redness, and low-grade fever.
2.Paroxysmal stage (1–6 weeks) is characterized by paroxysms of coughing that are the hallmark of pertussis. A whoop is an inspiratory gasp that may be heard at the very end of a coughing fit (although rarely observed in young infants). The coughing fits are exhausting, and posttussive vomiting is common. Young infants may have cyanosis, apnea, and choking during the paroxysms of cough. Between the coughing fits, children appear well and are afebrile.
3.Convalescent phase (weeks to months) is a recovery stage in which paroxysmal cough continues but becomes less frequent and severe over time.
4.Diagnosis
a.Diagnosis is suspected based on clinical features.
b.White blood cell (WBC) count is elevated with a significant lymphocytosis.
c.Diagnosis is confirmed by identification of B. pertussis by nasopharyngeal culture or polymerase chain reaction (PCR).
5.Management
a.Hospitalization of young infants often occurs during the paroxysmal phase because of choking, apnea, or cyanosis. Supportive care and oxygen (if needed) are important therapies.
b.Macrolide antibiotics are given to all patients and close contacts to prevent the spread of infection. Antibiotics do not alter the patient’s clinical course, unless they are administered during the catarrhal phase or very early in the paroxysmal phase.
c.Respiratory isolation is needed until antibiotics have been given for at least 5 days.
E.Bronchiolitis
1.Definition. Bronchiolitis is inflammatory bronchiolar obstruction with cellular debris and mucus plugging, most commonly secondary to a viral lower respiratory tract infection.
2.Epidemiology
a.Bronchiolitis is the most common lower respiratory tract infection in the first
2 years of life and the most common cause of hospitalization during the first year.
b.This disorder predominantly affects children younger than 2 years of age.
c.The male to female ratio is 2:1.
d.Epidemics occur from November to April.
e.Risk of infection is increased with day care attendance, multiple siblings, exposure to tobacco smoke, and lack of breastfeeding.
f.More significant disease occurs in patients with chronic lung disease, congenital heart disease, history of prematurity, immunodeficiency diseases, and genetic abnormalities, as well as in infants younger than 3 months of age.
3.Etiology
a.Respiratory syncytial virus (RSV) is the most common cause.
b.Less common causes include human metapneumovirus, parainfluenza, adenovirus,
341
rhinovirus, influenza, and coronavirus.
4.Clinical features
a.Onset is gradual, with upper respiratory symptoms, such as rhinorrhea, nasal congestion, fever, and cough.
b.Progression of respiratory symptoms includes tachypnea, fine rales, wheezing, and increased work of breathing.
c.Hypoxemia may occur.
d.Apnea may occur, especially in young infants and in children with a history of apnea of prematurity.
e.CXR may reveal hyperinflation with air trapping, patchy infiltrates, and atelectasis.
f.Improvement is usually noted within 2 weeks. More than 50% develop recurrent wheezing.
g.Complications may include apnea, respiratory insufficiency, respiratory failure, and death. Bacterial superinfection occurs rarely.
h.Immunity is incomplete, although repeat infections tend to be less severe.
5.Diagnosis is made on the basis of clinical features. Virologic testing is available if needed.
6.Management
a.Treatment is primarily supportive with nasal bulb suctioning (infants are obligatory nose breathers), hydration, and oxygen as needed for SpO2 < 90%.
b.Hand decontamination (preferably with alcohol-based rubs) is an essential part of contact isolation to prevent spread of infection.
c.Exposure to environmental tobacco smoke should be avoided.
d.Nebulized hypertonic saline may help hospitalized infants, but albuterol, epinephrine, and corticosteroids are no longer recommended.
e.Hospitalization is indicated for respiratory distress, hypoxemia, apnea, dehydration, or underlying cardiopulmonary disease.
f.RSV monoclonal antibody (palivizumab) may be given prophylactically as five monthly intramuscular injections during RSV season to prevent severe disease in infants with a history of prematurity, chronic lung disease, or hemodynamically significant congenital heart disease.
F.Pneumonia
1.Definition. Pneumonia involves infection and inflammation of the lung parenchyma associated with infiltrates on CXR.
2.Epidemiology. Pneumonia is associated with poverty, multiple siblings, exposure to tobacco smoke, and prematurity, as well as urban residence.
3.Etiology. Causes may be classified based on the child’s age (Table 9-2).
a.Viruses are the most common cause of pneumonia in all age groups.
b.S. pneumoniae is the single most common bacterial pathogen after first few weeks of life.
c.Staphylococcal pneumonias are often complicated by empyema.
d.Recurrent or persistent pulmonary infiltrates may have many causes and are further differentiated if occurring in a single lobe versus multiple lobes (Table 9-3).
4.Clinical features, diagnosis, and management vary depending on the etiologic agent.
a.Viral pneumonia
1.Symptoms often begin with upper respiratory complaints, such as nasal congestion and rhinorrhea. Fever, cough, and dyspnea typically follow.
2.Physical examination may demonstrate tachypnea, wheezing, rales, or respiratory distress.
342
3.Diagnosis is suggested by interstitial infiltrates on CXR and a WBC count
<20,000 cells/mm3 with a lymphocyte predominance.
4.Management is supportive.
b.Bacterial pneumonia
1.Symptoms have more rapid onset and greater severity. Fever, cough, and dyspnea typically occur without preceding upper respiratory symptoms.
2.Physical examination may demonstrate rales, tachypnea, decreased breath sounds, egophony (changes in voice transmission through consolidated lung), and evidence of respiratory distress.
3.Diagnosis is suggested by a WBC count >20,000 cells/mm3 with a neutrophil predominance, elevated C-reactive protein (CRP), and lobar consolidation on CXR.
4.Management includes appropriate antibiotics and supportive care.
c.Chlamydia trachomatis is a cause of afebrile pneumonia at 1–3 months of age, secondary to a perinatal-acquired infection from the maternal genital tract.
1.Symptoms include a staccato-type cough, dyspnea, and absence of fever. A history of conjunctivitis after birth may be identified in 50% of patients.
2.Physical examination may demonstrate tachypnea and wheezing.
3.Diagnosis is suggested by eosinophilia and a CXR with interstitial infiltrates. Definitive diagnosis is by positive culture, antigen detection, or nucleic acid amplification test from conjunctiva or nasopharynx.
4.Management includes an oral macrolide.
d.Mycoplasma pneumoniae is one of the most common causes of pneumonia in older children and adolescents.
1.Symptoms include low-grade fever, chills, nonproductive cough, headache, pharyngitis, and malaise. The cough may last 3–4 weeks.
2.Lung examination may demonstrate widespread rales. Examination findings are often worse than expected by history.
3.Diagnosis
a.Positive cold agglutinins are suggestive but are not specific.
b.Elevated EIA-IgM (enzyme-linked immunoassay for the detection of
IgM) is useful; PCR obtained by a nasopharyngeal swab is more sensitive.
c.CXR findings are variable and may show unilateral or bilateral infiltrates.
4.Management includes an oral macrolide, tetracycline, or quinolone.
e.Mycobacterium tuberculosis should be considered in all patients with risk factors for tuberculosis (see Chapter 7, section XVII.C).
Table 9-1
Differentiating Features of Supraglottic and Subglottic Disorders*
Feature |
Supraglottic Disorders |
Subglottic Disorders |
Stridor |
Quiet |
Loud |
Cough |
None |
Barky |
Voice |
Muffled |
Hoarse |
Dysphagia/drooling |
Present |
Absent |
Fever |
High |
Low to moderate (croup) |
|
|
High (tracheitis) |
Toxicity |
Present |
Absent, unless tracheitis is present |
Posture |
Neck extended, tripod position |
Normal |
*Supraglottic disorders include epiglottitis and retropharyngeal abscess. Subglottic disorders include bacterial tracheitis and viral croup.
343
Table 9-2
Age and Its Relationship to Pneumonia Etiology
Age |
Typical Causes |
0–3 months |
Congenital infections, such as syphilis, toxoplasmosis, CMV, rubella, herpes simplex virus, and tuberculosis |
|
Intrapartum-acquired infections, such as group B streptococcus (most common infection), Gram negative rods, |
|
and Listeria monocytogenes |
|
Postpartum infections, such as RSV and other respiratory viruses |
|
Afebrile pneumonitis caused by Chlamydia trachomatis, Ureaplasma urealyticum, Mycoplasma hominis, CMV, and |
|
PCP |
3 months– |
Viruses, such as adenovirus, influenza A and B, parainfluenza, HMPV, and RSV (note that RSV pneumonia is |
5 years |
generally uncommon beyond 2–3 years of age) |
|
Bacteria, most commonly Streptococcus pneumoniae, but may also include Staphylococcus aureus and HIB |
Age 6 and |
Mycoplasma pneumoniae and Chlamydia pneumoniae increasingly common |
older |
Viruses, such as adenovirus, influenza A and B, HMPV, and parainfluenza |
|
Bacteria, most commonly S. pneumoniae |
CMV = cytomegalovirus; RSV = respiratory syncytial virus; HMPV = human metapneumovirus; HIB = Haemophilus influenzae type b; PCP = Pneumocystis jiroveci pneumonia.
Table 9-3
Causes of Recurrent or Persistent Pulmonary Infiltrates
Single Lobe |
Multiple Lobes |
Intraluminal obstruction |
Aspiration |
Foreign body |
Impaired gag or swallow |
Tumor |
Esophageal obstruction or dysmotility, GERD |
Mucus plug |
Mucociliary clearance dysfunction |
Extraluminal obstruction |
Cystic fibrosis |
Enlarged lymph node from infection or malignancy |
Ciliary dyskinesia (e.g., immotile cilia syndrome) |
|
Bronchopulmonary dysplasia (chronic lung disease) |
Structural abnormalities |
Congenital heart disease |
Bronchial stenosis |
α1-antitrypsin deficiency |
Bronchiectasis |
Sickle cell disease |
Right middle lobe syndrome |
Hypersensitivity pneumonitis |
Congenital lung abnormalities, such as cysts or sequestration |
Pulmonary hemosiderosis |
|
Asthma |
|
Immunodeficiency diseases |
GERD = gastroesophageal reflux disease.
344
IV. Noninfectious Disorders of the Respiratory Tract
A.Asthma (reactive airway disease)
1.Definition
a.Asthma is a chronic inflammatory disorder of the airways that causes recurrent episodes of wheezing, cough, dyspnea, and chest tightness.
b.Symptoms are typically associated with widespread, variable airflow obstruction that is at least partially reversible, either spontaneously or with therapy.
c.Inflammation causes airway hyperresponsiveness to many stimuli.
2.Epidemiology. Asthma is the most common chronic pediatric disease.
a.Between 50 and 80% of children who have asthma develop symptoms before their fifth birthday.
b.Most patients with recurrent episodes of viral-triggered wheezing during their first year of life do not become asthmatics. This risk is increased if the child has a positive asthma predictive index. A positive asthma predictive index is either
1.One of the following: physician diagnosis of atopic dermatitis, parental history of asthma, or evidence of sensitization to aeroallergens OR
2.Two of the following: wheezing apart from colds, sensitization to foods, ≥4% eosinophils on CBC differential
c.Higher prevalence and severity in African American, Puerto Rican, and low socioeconomic populations.
3.Etiology
a.Predisposing factors involve interplay between host and environment, including multiple interacting genes, atopy, family history of asthma, and exposure to tobacco smoke. Viral respiratory infections, diet, and pollution can increase susceptibility in predisposed patients.
b.Triggers of exacerbations include respiratory infections, exercise, cold air, emotions, allergens, gastroesophageal reflux, and exposure to pollutants.
c.Asthma may accompany other acute or chronic lung diseases, such as cystic fibrosis.
4.Pathophysiology. Increased production and infiltration of inflammatory cells and mediators result in smooth muscle bronchoconstriction, airway mucosal edema, increased secretions with airway plugging, and possible airway wall remodeling.
5.Clinical features
a.Typical features during an exacerbation include tachypnea, dyspnea, nasal flaring, retractions, and multiphonic wheezing with a prolonged expiratory phase.
b.Some patients have only chronic or recurrent cough (especially at night).
c.CXR often reveals hyperinflation, peribronchial thickening, and patchy atelectasis.
d.PFTs reveal increased lung volumes and decreased expiratory flow rates.
6.Diagnosis
a.The basis of diagnosis is clinical features and usually a therapeutic response to a bronchodilator trial.
b.Spirometry (possibly with bronchoprovocation) can support diagnosis and should be attempted in a child 5 years of age or older. It can show airflow obstruction, which reverses following administration of bronchodilators.
c.“All that wheezes is not asthma.”
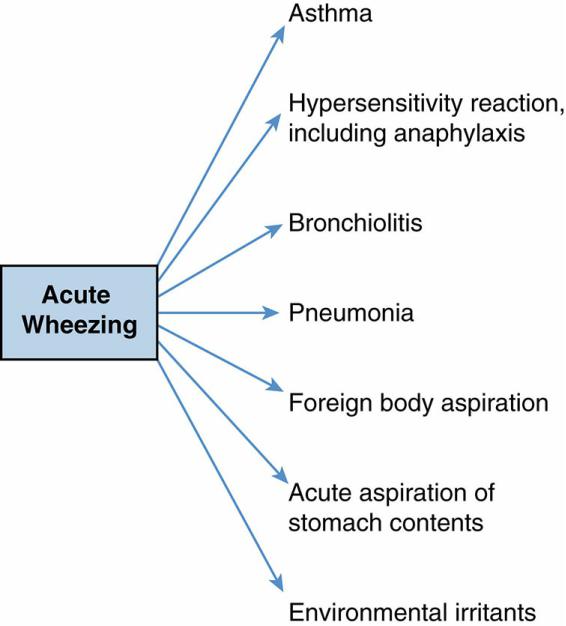
1.Differential diagnosis of acute wheezing (Figure 9-1)
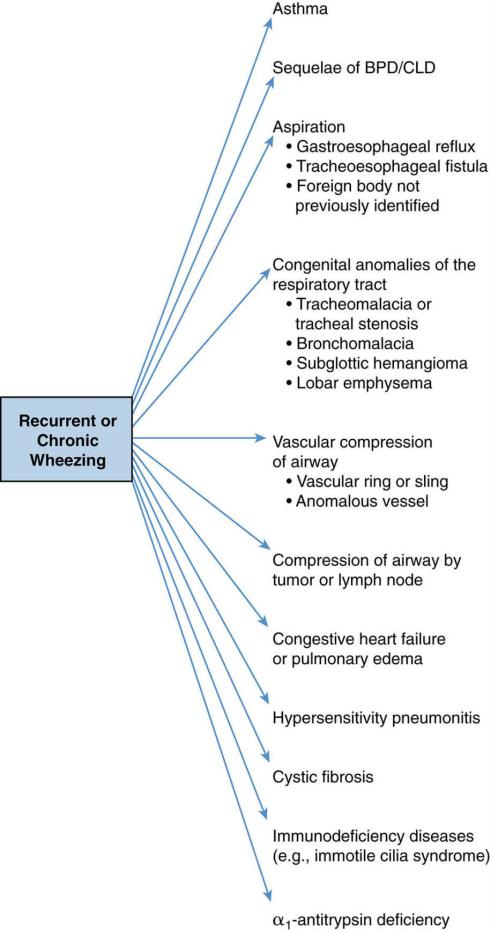
2.Differential diagnosis of recurrent or chronic wheezing (Figure 9-2)
345
7.Management. Therapy is initiated based on asthma severity, and is subsequently adjusted to obtain the goal of asthma control, with reduction of ongoing impairment as well as prevention of future risk.
a.Assessment and monitoring are performed at each visit to assess asthma control, medication administration technique, and patient adherence, as well as to address concerns.
b.Education is provided for self-monitoring and to reinforce self-management with oral demonstrations and written instructions. A spacer device (valved holding chamber) is recommended for administration of metered-dose inhalers.
c.Measures are recommended to control environmental factors (e.g., avoidance of allergens, pollutants, irritants) and treat comorbid conditions (e.g., allergic rhinitis, gastroesophageal reflux, obesity, stress).
d.Medications are prescribed and titrated using a stepwise approach. National guidelines classify asthma treatment by severity for three different age groups: 0– 4 years, 5–11 years, and 12 years and older. Table 9-4 reviews the classification of
asthma and initiating therapy. Table 9-5 reviews the stepwise approach to managing asthma long term.
1.Asthma is usually classified as “intermittent” if symptoms and/or short-acting betaagonist (SABA) use are ≤2 days/week, nighttime awakenings are
≤2×/month, and corticosteroid-requiring exacerbations are 0–1×/year. Treatment is with an short-acting beta-2 agonist (SABA), usually albuterol, as needed for quick relief of symptoms.
2.Patients with more frequent symptoms are classified as mild, moderate, or severe “persistent” asthma and require long-term controller medications, in addition to SABA for quick relief of symptoms.
a.Inhaled corticosteroids (ICS) are the most effective long-term control therapy for all ages. Start with low dose for mild persistent asthma.
b.Leukotriene modifiers (leukotriene receptor antagonist [LTRA]), such as montelukast, are alternative although less effective controllers.
c.With increased symptoms/severity (moderate–severe persistent asthma), consider increasing the ICS dose and/or adding an inhaled long-acting beta-agonist (LABA), theophylline, or LTRA.
3.Long-term control therapy with low-dose ICS or montelukast should also be considered for children who are 0–4 years of age and who have had ≥4 episodes of wheezing in the past year that lasted >1 day and affected sleep AND who have a positive Asthma Predictive Index.
4.To prevent exercise-induced bronchospasm, pretreatment with SABA or LTRA is recommended, in addition to a warm-up period.
5.Acute exacerbations are treated with repetitive or continuous inhaled SABA, a short course of systemic corticosteroids, and supplemental oxygen as needed.
B.Cystic fibrosis (CF)
1.Definition. CF is a chronic progressive multisystem genetic disorder with major manifestations in the respiratory, gastrointestinal (GI), and reproductive systems.
2.Epidemiology
a.CF affects 1 in 3000 Caucasians and is less common in Hispanics, African Americans, and Asians.
b.Five percent of Caucasians are carriers.
c.Median age of survival has increased to 41 years with CF center–based care.
3.Etiology. CF is an autosomal recessive disease resulting from genetic mutations on chromosome 7. 2000 known mutations cause a wide spectrum of phenotypes ranging
346
from mild and atypical to severe and classic.
4.Pathophysiology
a.The genetic defect produces an abnormal cystic fibrosis transmembrane conductance regulator (CFTR) protein that causes sodium and chloride transport dysfunction in exocrine epithelial cells and submucosal glands.
b.In the lungs, abnormal thick, viscous mucus results in airway obstruction, inflammation, and infection causing bronchiectasis.
5.Clinical features
a.Recurrent or chronic respiratory symptoms, steatorrhea, and failure to thrive
(FTT) are typical presenting features. Clinical expression is variable. See Figure 9-3 for the multisystem signs and symptoms of CF.
b.Chronic, recurrent sinopulmonary disease includes chronic productive cough, dyspnea, lung hyperinflation, lung crackles, wheezing, pansinusitis, nasal polyps, digital clubbing, and progressive hypoxemia.
1.PFTs show decreased respiratory flow rates (consistent with obstruction) and eventually decreased lung volumes (consistent with restriction).
2.Pneumonia develops as the lungs become colonized, first with Staphylococcus aureus and later with mucoid Pseudomonas aeruginosa.
3.Common pulmonary complications include hemoptysis, pneumothorax, recurrent pneumonia exacerbations, severe bronchiectasis, allergic bronchopulmonary aspergillosis, pulmonary fibrosis, cor pulmonale, and eventually respiratory failure.
c.GI and nutritional abnormalities, include pancreatic insufficiency in 90% of patients, with malabsorption predisposing to malnutrition, deficiencies of vitamins A, D, E, and K, and FTT, with possible later complication of CF-related diabetes mellitus.
d.Salt depletion syndromes secondary to sweat electrolyte losses
e.Male urogenital abnormalities, including congenital absence of the vas deferens
6.Diagnosis requires the following:
a.One or more characteristic phenotypic features or positive family history or increased immunoreactive trypsinogen (IRT) on newborn screen AND
b.Laboratory evidence of abnormal CFTR function, including sweat chloride
>60 mmol/L or two CFTR mutations or a characteristic ion transport abnormality across the nasal epithelium
7.Management. Goals are to preserve the lung function, optimize nutrition, and both prevent and treat complications, while maintaining quality of life.
a.Airway clearance therapies (e.g., postural drainage and percussion, chest wall oscillating vest) combined with mucus-altering therapies (e.g., DNase, hypertonic saline) to remove abnormal secretions
b.Antibiotics (inhaled, oral, IV) to control chronic airway infection and treat acute pulmonary exacerbations
c.High-calorie diet, pancreatic enzyme replacement, fat-soluble vitamins (A, D, E, and K), and insulin, if needed, to optimize nutritional status
d.Anti-inflammatory therapy (e.g., high-dose ibuprofen, but not corticosteroids) to treat chronic airway inflammation
e.Mutation-specific disease-modifying therapies (e.g., ivacaftor) to correct gene defects
f.Oxygen as needed for hypoxemia
g.Lung transplantation
h.Psychosocial support for patients and families
347
C.Bronchopulmonary dysplasia (BPD; also termed chronic lung disease of infancy [CLDI]; see also Chapter 4, section VI.G.2.a)
1.Definition. Infants with lung disease of prematurity who require supplemental oxygen ≥28 postnatal days are classified as having mild, moderate, or severe BPD, depending on the level of respiratory support needed.
2.Epidemiology. BPD follows exposure of premature lungs to various antenatal and postnatal insults. Risk increases with increased prematurity and decreased birth weight.
3.Etiology and pathophysiology
a.Previously, the development of BPD followed treatment with high FiO2 (fraction of inspired oxygen) and aggressive mechanical ventilation, which resulted in diffuse airway damage, smooth muscle hypertrophy, polymorphonuclear cell (PMN) inflammation, and parenchymal fibrosis.
b.The current BPD phenotype is manifest primarily by impaired alveolar and vascular development secondary to extreme prematurity. “New” BPD has milder airway injury, inflammation, and fibrosis than “old” BPD because of improved neonatology practices.
c.Decreased and simplified alveoli result in less surface area for gas exchange.
4.Clinical features vary and range from transient oxygen dependency to a prolonged need for ventilatory support.
a.Diminished oxygenation (decreased PaO2) and hypercarbia (increased PaCO2) are often found on ABG testing.
b.Chronic increased work of breathing with intermittent episodes of tachypnea, wheezing, sputum production, and respiratory distress.
c.Frequent respiratory tract infections, airway hyperreactivity, and pulmonary hypertension may result.
d.CXR is diffusely hazy to coarsely irregular and may remain abnormal for several years.
e.Nonpulmonary manifestations include increased caloric needs, feeding intolerance, delayed growth, and neurodevelopmental sequelae.
5.Management
a.Goals of treatment are to minimize the lung damage, promote growth of new lung tissue, maintain optimal oxygenation, and prevent complications.
b.Most important therapy is supplemental oxygen, which may be needed after discharge to home.
c.Optimize high caloric intake for growth.
d.Consider bronchodilators, diuretics, and/or fluid restriction to transiently improve pulmonary function.
e.Prevent complicating infections through avoidance of ill contacts, appropriate immunization practices, and RSV prophylaxis.
f.Avoid passive smoke exposure.
g.Focus on early identification and treatment of complications, such as subglottic stenosis, gastroesophageal reflux disease, and tracheobronchomalacia.
6.Prognosis. Pulmonary symptoms and disease usually improve with time and lung growth. Some patients have increased risk of rehospitalization, continued airway hyperreactivity, exercise limitation, delays in development, and poor tolerance of respiratory infections. There is a possibility of risk of developing chronic obstructive pulmonary disease (COPD) during adulthood.
D.Foreign body aspiration
1.Epidemiology. Children 3 months–5 years of age are at greatest risk for small object aspiration.
348
2.Etiology. Typical aspirated objects include seeds, popcorn, hot dogs, candy, grapes, and small toy parts.
3.Clinical features depend on location and biologic reactivity of the material aspirated.
a.History may elicit choking episode in 50–80% of cases.
b.Laryngotracheal foreign bodies (extrathoracic) result in cough, hoarseness, and inspiratory stridor.
c.Bronchial foreign bodies (intrathoracic; right bronchus slightly more common thanleft)
1.Asymmetric findings on auscultation
2.Complete obstruction with atelectasis, partial ball-valve obstruction with unilateral emphysema, or no obstruction that initially can be asymptomatic.
3.Localized wheezing, persistent pneumonia, chronic cough, or hemoptysis
d.Esophageal foreign bodies may compress the trachea, producing respiratory symptoms.
4.Diagnosis is challenging. Have a high index of suspicion!
a.A radiopaque object is evident on CXR in only 15% of cases.
b.Consider inspiratory and expiratory films, or bilateral decubitus films in young children who cannot inspire and expire on command, or fluoroscopy to identify air trapping distal to a foreign body.
5.Management
a.Basic life support is the initial management for a severe choking episode.
b.Natural cough, if present, is the most effective expulsive mechanism.
c.Foreign bodies that remain in the airway must be removed by bronchoscopy.
E.Apnea, apparent life-threatening event (ALTE), Brief resolved unexplained event (BRUE), sudden infant death syndrome (SIDS), and obstructive sleep apnea syndrome (OSAS)
1.Definitions
a.Apnea of infancy is the unexplained cessation of breathing for ≥ 20 seconds, or a shorter respiratory pause associated with bradycardia, cyanosis, pallor, or hypotonia in a full-term infant.
1.Respiratory pause may be central (no respiratory effort), obstructive (efforts at respiration are made but are unsuccessful, usually because of upper airway obstruction), or both.
2.Short central apnea for ≤15 seconds is normal at all ages.
b.Apnea of prematurity is the unexplained cessation of breathing for ≥ 20 seconds in a premature infant (see also Chapter 4, section IX). This usually resolves by 37–
40 weeks postconceptual age.
c.Periodic breathing is a normal breathing pattern in young infants with three or more respiratory pauses lasting at least 3 seconds each, with less than 20 seconds of normal respiration in between.
d.ALTE/BRUE is a frightening event characterized by some combination of apnea, color change, change in muscle tone, choking, or gagging, in which recovery occurs only after stimulation or resuscitation.
e.SIDS is the sudden death of a child younger than 1 year of age that is unexplained after a thorough investigation, including a complete autopsy, an examination of the death scene, and a review of the clinical history.
f.OSAS is a disorder of breathing during sleep that is characterized by prolonged partial upper airway obstruction and/or intermittent complete obstruction (obstructive apnea) that disrupts normal ventilation during sleep and normal sleep patterns. Obstructive sleep apnea (OSA) is typically worse during rapid eye movement (REM) sleep. Ongoing OSA is associated with risk for neurocognitive
349
and cardiovascular morbidity.
2.Epidemiology
a.SIDS reaches its peak incidence at 2–4 months of age, and 95% of cases occur before 6 months of age.
b.Risk factors for SIDS
1.Prone sleeping position
2.Soft bedding, overbundling, and overheating
3.Prematurity
4.Being the twin of a sibling who died of SIDS
5.Low birth weight or growth retardation
6.Recent illness
7.Lack of breastfeeding
8.Maternal smoking, drug abuse, or infection
3.Etiology
a.Apnea of prematurity is usually caused by immature central respiratory center control.
b.Obstructive apnea may be secondary to craniofacial anomalies, adenotonsillar hypertrophy, obesity, or hypotonia.
c.The cause of SIDS is unknown.
d.No definite cause and effect relationship has been proven among apnea, ALTE/BRUE, and SIDS.
4.Differential diagnosis of ALTE/BRUE
a.Seizure disorder
b.Gastroesophageal reflux disease (GERD)
c.Upper airway obstruction
d.Intracranial mass lesion
e.Sepsis or other infections, including RSV, pertussis, and meningitis
f.Metabolic abnormalities, including electrolyte imbalance and hypoglycemia
g.Inborn errors of metabolism
h.Arrhythmia, including long QT syndrome
i.Abnormal central control of breathing
j.Munchausen by proxy
k.Nonaccidental trauma (shaken baby syndrome)
5.Evaluation
a.Detailed history and physical examination, especially HEENT (head, eyes, ears, nose, and throat), is essential.
b.Further testing is based on clinical impression from the history and physical examination and may include the following:
1.Hospital observation and monitoring
2.Blood work, including complete blood count, ABG, electrolytes, and evaluation for infection
3.CXR, electrocardiogram, and electroencephalogram
4.Multichannel recording (sleep study), which simultaneously evaluates oxygen saturation, airflow, chest wall movement, and cardiac rhythm
5.Barium esophagram or pH probe study to evaluate for GERD
6.Imaging studies of the head and neck
7.Workup for metabolic disease
6.Management
a.For infant apnea and ALTE, teach caregivers cardiopulmonary resuscitation techniques.
350
b.For moderate–severe OSAS, consider adenotonsillectomy and/or continuous positive airway pressure (CPAP) therapy.
c.Home cardiorespiratory monitors should not be prescribed to prevent SIDS, and the following prevention strategies should be followed:
1.Sleep on the back
2.Firm bedding without pillows or blankets
3.Avoid overheating
4.Smoke-free environment
5.Early prenatal care and regular well-child care
6.Breastfeed
FIGURE 9.1 Differential diagnosis of acute wheezing.
351
352

FIGURE 9.2 Differential diagnosis of recurrent or chronic wheezing. BPD/CLD = bronchopulmonary
dysplasia/chronic lung disease.
Table 9-4
Classifying Asthma Severity and Initiating Therapy in Patients Not Taking Long-Term Controller Medications
Components of Severity |
Classifying |
|
|
|
|
|
|
|
|
|
|
Asthma |
|
|
|
|
|
|
|
|
|
|
Severity |
|
|
|
|
|
|
|
|
|
|
Intermittent |
|
Persistent |
|
|
|
|
|
|
|
|
|
|
Mild |
|
Moderate |
Severe |
|
|||
|
Ages 0–4 |
Ages 5–11 |
Ages |
Ages |
Ages |
|
Ages 5–11 |
Ages |
|
Ages 5– |
|
0–4 |
5–11 |
0–4 |
|
0–4 |
|
11 |
|||
|
|
|
|
|
|
|||||
Symptoms |
≤2 days per week |
>2 days per |
Daily |
|
Throughout the |
|||||
|
|
|
week but not |
|
|
|
day |
|
||
|
|
|
daily |
|
|
|
|
|
|
|
Night awakenings |
0 |
<2× per month |
1–2× |
3–4× |
3–4× |
|
>1× per week |
>1× |
|
Often 7× |
|
|
|
per |
per |
per |
|
but not |
per |
|
per |
|
|
|
month |
month |
month |
|
nightly |
week |
|
week |
Short-acting beta-agonist: |
≤2 days per week |
>2 days per |
Daily |
|
Several times |
|||||
use for symptom control |
|
|
week but not |
|
|
|
per day |
|
||
|
|
|
daily |
|
|
|
|
|
|
|
Interference with activity |
None |
|
Minor |
|
Some limitation |
Extremely |
||||
|
|
|
limitation |
|
|
|
limited |
|
||
Lung function: FEV1 or |
N/A |
Normal between |
N/A |
>80% |
N/A |
|
60–80% |
N/A |
|
<60% |
peak flow |
|
exacerbations |
|
|
|
|
|
|
|
|
|
|
(>80%) |
|
|
|
|
|
|
|
|
Exacerbations |
In general, more frequent and severe exacerbations (e.g., hospitalizations, urgent care, intensive |
|||||||||
|
care unit admission) indicate greater underlying disease severity |
|
|
|
|
|||||
Recommended step for |
Step 1 |
|
Step 2 |
|
Step 3 |
|
Step 3 or 4 |
|||
initiating therapy (see |
|
|
|
|
|
|
|
|
|
|
Table 9-5) |
|
|
|
|
|
|
|
|
|
|
National Asthma Education and Prevention Program, Third Expert Panel on the Diagnosis and Management of Asthma. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Bethesda (MD): National Heart, Lung, and Blood Institute (US), August 2007:40 and 42.
FEV1 = forced expiratory volume during the first second of forced breath.
Table 9-5
Stepwise Approach to Managing Asthma Long Term
STEP-UP MEDICATION IF NEEDED (Check Medication Adherence, Inhaler Technique, Other Contributing Factors)
STEP-DOWN MEDICATION (If Asthma Is Well Controlled for at Least 3 Months)
|
Step 1 |
Step |
Step 3 |
Step 4 |
Step 5 |
Step 6 |
|
|
2 |
|
|
|
|
|
Intermittent Asthma |
Persistent Asthma (daily medication) |
|
|||
0–4 years |
SABA |
Low- |
Medium-dose ICS |
Medium-dose |
High-dose |
High-dose ICS + either |
|
as |
dose |
|
ICS + either LABA |
ICS + either |
LABA or |
|
needed |
ICS |
|
or montelukast |
LABA or |
montelukast + oral |
|
|
|
|
|
montelukast |
corticosteroids |
5– |
SABA |
Low- |
Low-dose ICS + either LABA, |
Medium-dose |
High-dose |
High-dose |
11 years |
as |
dose |
LTRA or theophylline OR |
ICS + LABA |
ICS + LABA |
ICS + LABA + oral |
|
needed |
ICS |
Medium-dose ICS |
|
|
corticosteroids |
>12 years |
SABA |
Low- |
Low-dose ICS + LABA OR |
Medium-dose |
High-dose |
High-dose |
|
as |
dose |
Medium-dose ICS |
ICS + LABA |
ICS + LABA |
ICS + LABA + oral |
|
needed |
ICS |
|
|
|
corticosteroids |
Adapted from National Asthma Education and Prevention Program, Third Expert Panel on the Diagnosis and Management of Asthma. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Bethesda (MD): National Heart, Lung, and Blood Institute (US), August 2007:42.
Quick Relief Medication: SABA as needed for relief of symptoms. Short course of oral steroids may be needed for exacerbations.
SABA = short-acting beta-2 agonist; ICS = inhaled corticosteroid; LABA = long-acting inhaled beta-2 agonist; LTRA = leukotriene receptor antagonist.
353

FIGURE 9.3 Features of cystic fibrosis.
354
