
- •Copyright
- •Contents
- •Dedication
- •Preface
- •Acknowledgments
- •Contributors
- •Contributors to the Previous Edition
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •IV. Hypertension
- •VI. Nephrotic Syndrome (NS)
- •VII. Hemolytic Uremic Syndrome (HUS)
- •VIII. Hereditary Renal Diseases
- •IX. Renal Tubular Acidosis (RTA)
- •XI. Chronic Kidney Disease (CKD) and End-Stage Renal Disease (ESRD)
- •XII. Structural and Urologic Abnormalities
- •XIII. Urolithiasis
- •XIV. Urinary Tract Infection (UTI)
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •IV. Food Allergy
- •VI. Urticaria (Hives)
- •VII. Drug Allergy
- •VIII. Asthma
- •IX. Immunology Overview
- •X. Disorders of Lymphocytes (Figure 15-2)
- •XI. Disorders of Granulocytes (Figure 15-3)
- •XII. Disorders of the Complement System
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Review Test
- •Answers and Explanations
- •Comprehensive Examination
- •Index
Answers and Explanations
1.The answer is E [IV.B.2]. Malrotation is the result of abnormal rotation and fixation of the intestines in utero. In heterotaxy, the intestines begin their rotation from an already abnormal position, and this results in final fixation in a variable position. This variable rotation and final position can lead to twisting of the intestines and volvulus. Pyloric stenosis is a thickening of the pylorus muscle that results in projectile vomiting. Intestinal malrotation is not present in this disorder. Ulcerative colitis is a type of inflammatory bowel disease in which many intestinal manifestations may be present, including rectal bleeding, diarrhea, abdominal pain, and toxic megacolon, but not intestinal malrotation. Patients with Down syndrome may have duodenal atresia but are at no increased risk for malrotation. Renal anomalies are not associated with malrotation.
2.The answer is C [IV.A.4 and IV.A.5]. The infant’s symptoms are the classic presentation of hypertrophic pyloric stenosis. Forceful vomiting of stomach contents develops, and the vomiting persists unless it is corrected surgically. This persistent vomiting causes a progressive loss of hydrogen ions and chloride, resulting in hypochloremia and a metabolic alkalosis. If hydrogen ion loss is severe, hypokalemia often develops as well.
3.The answer is D [IV.C.1]. Duodenal atresia is a congenital anomaly that develops because of failure of the intestinal lumen to recanalize early in gestation. As a result, the fetus is unable to swallow significant amounts of amniotic fluid, and this may lead to polyhydramnios. Postnatally, duodenal atresia leads to vomiting, epigastric distension (proximal to the obstruction), and absence of intestinal bowel gas that causes a scaphoid appearance to the abdomen. Although the abdomen may be scaphoid in appearance with congenital diaphragmatic hernia, polyhydramnios is not associated with this condition, and these infants present with severe respiratory distress at birth. Pyloric stenosis, malrotation, and Hirschsprung disease are not associated with a scaphoid abdomen or polyhydramnios.
4.The answer is A [V.B.2.d]. The clinical presentation is most consistent with pancreatitis. In children, approximately 25% of cases of pancreatitis are idiopathic (without identifiable cause). Idiopathic pancreatitis is second only to blunt abdominal trauma, which is the leading cause of acute pancreatitis during childhood. Sepsis, viral infections, and drug or toxin exposure are other important causes of pancreatitis in children but are less common than trauma or the idiopathic category. Congenital anomalies of the pancreas and biliary tree are also less common causes.
5.The answer is E [IV.D.5]. This infant’s history is consistent with intussusception, in which the intestine telescopes into itself, causing bowel wall edema, mucosal injury, and eventually necrosis. The child typically presents with colicky abdominal pain, often accompanied by vomiting, lethargy, and bloody stools. The most appropriate initial test to diagnose intussusception is an abdominal ultrasound. Experienced radiologists may also then perform the potentially therapeutic contrast enema under ultrasound guidance. Surgical exploration is indicated for intussusception that fails to reduce with contrast enema or if peritonitis is suspected. Plain radiography is not generally sensitive for this diagnosis. Upper gastrointestinal imaging with small bowel follow-through will not show most cases of intussusception, which most commonly occurs in the ileocolic location.
6.The answer is C [VII.D.1]. This patient’s constipation is most likely functional or nonorganic (functional fecal retention). Functional constipation results from an inappropriate constriction of the external anal sphincter. Most commonly, toddlers retain stool purposely because of a traumatic event, such as a painful diaper rash, painful diarrhea, or even physical or sexual abuse. Encopresis may be associated with severe constipation and could eventually result in this patient. Organic causes of constipation (e.g., Hirschsprung disease, hypothyroidism,
404
infant botulism) account for less than 5% of constipation seen during childhood. Therefore, radiographic studies are not indicated unless suggested on the basis of history or physical examination. Because this patient’s constipation is associated with pain, management should include stool evacuation using osmotic laxatives, enemas, or other modalities. Recommendations for increased dietary fiber, water, and juice are important adjuncts to treatment but alone are insufficient for this patient whose constipation is significant and resulting in very hard stools and crying during defecation.
7.The answer is E [II.B.3]. Protein intolerance occurs in up to 8% of all infants and is usually caused by cow’s milk protein or soy protein allergy. Protein intolerance may present with vomiting, diarrhea, irritability, rectal bleeding, and weight loss. Diagnosis of protein intolerance is made up on resolution of symptoms after a complete withdrawal of the suspected antigen. Symptoms usually resolve within 1–2 weeks of stopping the offending protein. Because this approach to treatment and diagnosis is noninvasive and effective, abdominal radiographs, small bowel biopsy, and allergy testing are not necessary and are overly invasive for this 4-week-old. In addition, radiographs are not diagnostic, and this infant is too young for a response to allergy skin testing. Stool-reducing substances and an abnormal acidic pH are found in carbohydrate malabsorption, not protein malabsorption.
8.The answers are B and C, respectively [IX.C and Table 10-4]. Patients with Crohn disease, like the girl in question 8, may present with diarrhea, abdominal cramping, and loss of appetite. Perianal skin disease, such as skin tags, fissures, and fistulas, may precede intestinal symptoms. Patients with Crohn disease may also have poor growth and delayed puberty. Patients with ulcerative colitis, like the boy in question 9, often present with rectal bleeding, diarrhea, and abdominal pain. In addition, his presentation with fever, abdominal distension and low blood pressure may be consistent with toxic megacolon, a severe complication of ulcerative colitis. In contrast, celiac disease presents with bloating, foul-smelling stools, diarrhea, and vomiting. Delayed sexual maturity is unusual, stools are nonbloody, and perianal disease is not usually present. Irritable bowel syndrome is associated with bloating, cramping, and alterations in stool patterns. Lactase deficiency is a disorder of carbohydrate absorption and presents with bloating and diarrhea.
9.The answer is D [X.C.3.a]. Before further investigation or definitive therapy, the most important step in any patient who may have hypovolemia or significant or worsening anemia is initial stabilization, including the ABCs (airway, breathing, and circulation). This includes placement of two large-bore intravenous lines for fluid resuscitation. Because the heart rate is elevated, suggesting hypovolemia, a normal saline solution bolus would also be an appropriate initial step in management. After stabilization, placement of a nasogastric tube to confirm upper gastrointestinal bleeding and ordering a complete blood count to assess the patient’s hemoglobin are appropriate. Intravenous H2-blockers are used if gastritis, esophagitis, or ulcer disease is suspected. Upper endoscopy would also likely be needed to
diagnose the cause of the bleeding, but after the patient has been initially stabilized.
10.The answer is A [II.C.2.b and II.C.5]. This patient presents with the classic features of celiac disease (gluten-sensitive enteropathy). Signs and symptoms usually develop between
6 months and 2 years of age when gluten is introduced into the diet. The treatment of celiac disease is restriction of gluten from the diet. Wheat, barley, and rye all contain gluten. Oats also usually contain gluten because most oats are harvested in fields that also contain wheat. Rice is the only food listed that does not contain gluten and can be eaten safely by patients with celiac disease.
11.The answer is A [III.G.2]. Gastroesophageal reflux disease results from inappropriate transient lower esophageal sphincter relaxation that allows gastric contents to reflux into the esophagus, and manifests as vomiting, irritability, arching of the back, poor weight gain, and pulmonary symptoms (e.g., wheezing). After a trial of conservative management that includes positioning
405
and thickened feeds, medical management with antacids, H2-blockers, or proton-pump inhibitors is indicated. Dietary changes would be ineffective at this time. Nissen fundoplication with gastric antroplasty and gastrostomy tube feedings may be required should medical management fail.
12.The answer is D [XI.C.1, XI.C.4.e, and XI.C.4.f]. This patient has cholestasis, or retention of bile within the liver, manifested by the elevated conjugated (direct) bilirubin. In addition, the findings of hepatomegaly and poor growth (he has only gained 8 oz since birth) are consistent with the diagnosis of cholestasis. The causes of cholestasis are many, and biliary atresia and choledochal cyst must always be considered and ruled out rapidly in any infant who presents with conjugated hyperbilirubinemia. This evaluation includes an abdominal ultrasound and liver biopsy in rapid sequence. Should biliary atresia not be identified promptly (by 50–
70 days of age), liver transplantation may be the only treatment option. Phototherapy is not indicated for direct hyperbilirubinemia. Neonatal hepatitis is a possible cause of this patient’s symptoms, but biliary atresia must first be ruled out. Ursodeoxycholic acid enhances bile flow, but it is recommended only once biliary obstruction has been excluded.
13.The answer is A [XI.F.2 and Figure 10-2]. Hepatitis A infection is the most common hepatitis virus infection and usually occurs through fecal–oral contamination. Only 30% of children infected with the hepatitis A virus have symptoms of hepatitis (the majority of hepatitis A infections are asymptomatic during childhood), but even those with hepatitis symptoms very rarely have jaundice. Hepatitis D infection requires the presence of hepatitis B surface antigen (HBsAg) for replication, not hepatitis A virus. Chronic hepatitis A infection does not occur, but up to 25% can have a relapse of symptoms at some point after recovery from the initial infection. Patients shed virus in the stool for 2–3 weeks before the onset of any symptoms and for 1 week after the onset of symptoms. Serologic testing confirms the diagnosis. Both IgM and IgG antibodies to hepatitis A virus rise early in infection.
14.The answer is D [VI.C and Table 10-2]. Nonorganic or functional abdominal pain is much more common than organic abdominal pain in children. However, although the pain is nonorganic, some children do have minor disturbances in gastrointestinal motility or in their parasympathetic or sympathetic nervous systems that make them susceptible to the pain. It is important to understand that the pain is real to the patient, and therefore, management should focus on empowering the child and family to overcome the discomfort. In addition, the child must resume and normalize all activities, including attending school even when pain is present. Although 50% of patients have resolution of symptoms during childhood, at least 25% still have pain as adults.
406

C H A P T E R 1 1
407

Nephrology and Urology
Elaine S., Kamil, Lee Todd, Miller
408
I.Fluids, Electrolytes, and Dehydration
A.General principles
1.The most common cause of acute fluid and electrolyte imbalance is acute diarrhea with dehydration.
2.Worldwide, acute diarrheal diseases are among the leading causes of childhood morbidity and mortality.
B.Total body fluid requirement is the sum of a patient’s maintenance fluid needs, replacement of prior fluid losses (i.e., deficits), and replacement of ongoing losses, if any.
1.Maintenance water and electrolyte calculations are designed to balance the usual daily losses of water and salts that occur as a result of normal daily metabolic activities. These losses take both measurable forms (sensible losses), such as urinary losses, and less readily measurable but still clinically significant forms (insensible losses), such as losses from the skin, lungs, and gastrointestinal (GI) tract.
a.Maintenance water requirement is approximately 1500 mL/m2/day for children. Water requirements for infants and premature infants vary with the birth weight and postnatal age.
b.Maintenance water requirement may alternatively be calculated from the patient’s weight.
1.100 mL/kg/day for the first 10 kg of body weight
2.50 mL/kg/day for the second 10 kg of body weight
3.20 mL/kg/day for each kg above the first 20 kg of body weight
c.Maintenance fluids should be increased if the patient has increased insensible losses, such as respiratory distress and fever (i.e., about a 10% increase for every degree of temperature).
d.Maintenance sodium (Na+) requirement is approximately 2–3 mEq/kg/day.
e.Maintenance potassium (K+) requirement is approximately 2 mEq/kg/day.
2.Deficit fluid calculations are designed to replace abnormal losses of water and salts caused by pathologic states, such as diarrhea and vomiting. Deficit fluids are calculated as follows: Fluid deficit (L) = pre-illness weight (kg) − current weight (kg).
3.Ongoing loss calculations are designed to replace additional losses of water and salts after the patient’s initial evaluation (e.g., ongoing vomiting or diarrhea, nasogastric tube aspirate). These ongoing losses are replaced milliliter for milliliter.
C.Dehydration may be classified by both the initial serum Na+ level and by the degree of dehydration.
1.Classification by serum sodium concentration
a.Hyponatremic dehydration (Na+ < 130 mmol/L)
b.Isonatremic dehydration (Na+ = 130–150 mmol/L)
c.Hypernatremic dehydration (Na+ > 150 mmol/L)
2.Classification by degree of dehydration
a.Mild dehydration (3–5%) is associated with normal pulse rate and quality, flat fontanelle, dry mucous membranes, normal skin turgor, normal capillary refill, and normal to decreased urine output.
b.Moderate dehydration (7–10%) is associated with mild tachycardia with a weak pulse, flat fontanelle, deep set eyes, reduced tears, dry mucous membranes, skin tenting, and capillary refill of about of 2 seconds, in a patient with decreased urine output.
c.Severe dehydration (≥10%) is associated with tachycardia and feeble pulse, sunken fontanelle, sunken eyes, no tears, parched and cracked lips and buccal mucosa,
409
clammy skin, and capillary refill >3 seconds, in a patient with lethargy and anuria.
D.Parenteral rehydration should occur in two phases:
1.Emergency phase
a.The goal of the emergency phase is to restore or maintain the intravascular volume to ensure perfusion of vital organs.
b.The emergency phase is the same for all patients, regardless of the patient’s initial serum sodium level.
c.20 mL/kg boluses of intravenous (IV) solutions with a high enough oncotic load (e.g., normal saline or lactated Ringer solution) are commonly used.
2.Repletion phase
a.The goal of the repletion phase is a more gradual correction of the patient’s water and electrolyte deficits.
b.Patients with the acute onset of hyponatremic or isonatremic dehydration generally have their fluid and electrolyte deficits replaced over 24 hours. Chronic hyponatremia should be corrected much more slowly.
c.Patients with hypernatremic dehydration generally have their fluid and electrolyte deficits replaced more slowly, usually over 48 hours, to minimize the risk of cerebral edema that may accompany rapid fluid correction.
E.Oral rehydration therapy (ORT)
1.ORT may be an effective, safe, and inexpensive alternative to IV rehydration therapy.
2.Oral rehydration salt (ORS) solutions are balanced mixtures of glucose and electrolytes for use in treating and preventing dehydration, potassium depletion, and base deficits caused by diarrhea.
3.ORT is based on the principle that the intestinal absorption of sodium and other electrolytes is enhanced by the active absorption of glucose (coupled cotransport mechanism). This coupled cotransport process of intestinal absorption continues to function normally during secretory diarrhea, whereas other pathways of intestinal absorption of sodium are impaired.
4.ORT is inappropriate for patients with severe life-threatening dehydration, for patients with paralytic ileus or GI obstruction, and for patients with extremely rapid stool losses or repeated severe emesis losses.
410
II.Hematuria
A.Definition. Hematuria is defined as the presence of red blood cells (RBCs) in the urine. Hematuria may be seen on voiding (gross hematuria) or only on urinalysis (microscopic hematuria). Microscopic hematuria is defined as ≥5–6 RBCs per high-power field (HPF) detected on two or more consecutive samples.
B.Epidemiology. Approximately 5% of school children have microscopic hematuria detected on a single voided urine sample, but only 0.5–2% have persistent microscopic hematuria.
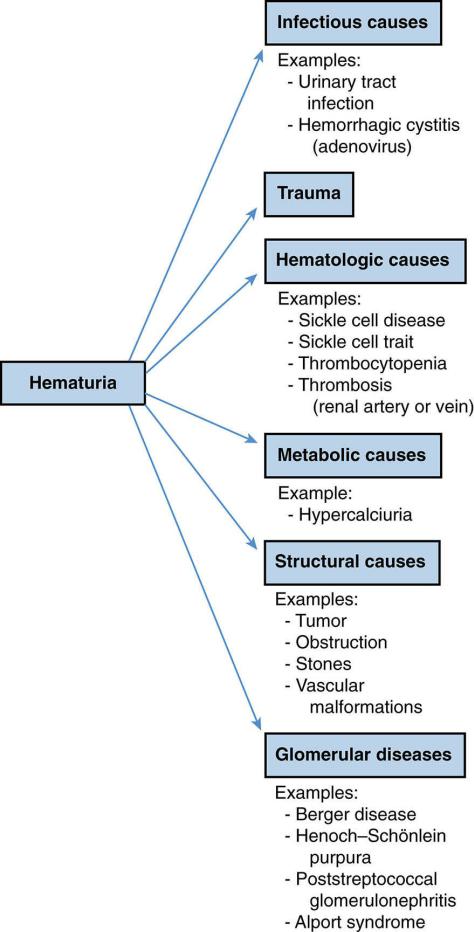
C.Clinical significance. Microscopic hematuria may be an indicator of a serious medical condition such as a tumor or chronic glomerulonephritis or may be of no serious medical consequence. Discolored urine may not be from blood in the urine. See Figure 11-1 for clues regarding the causes of discolored urine. The differential diagnosis of hematuria is outlined in Figure 11-2.
D.Evaluation (Figure 11-1). Detection of hematuria may be by urinary dipstick or by microscopy. Urinary dipstick detects the presence of hemoglobin or myoglobin in the urine.
False-negative results may occur with ascorbic acid (vitamin C) ingestion. Microscopic urinalysis may also provide helpful clues. When RBCs are present on microscopic examination, careful examination of RBC morphology and identification of other urine elements, such as casts or bacteria, may be extremely helpful in determining the cause of the hematuria.
1.RBC morphology
a.RBCs originating in the glomerulus are dysmorphic in character, often with blebs in the RBC membrane.
b.RBCs that appear to be normal biconcave disks usually originate in the lower urinary tract.
2.RBC casts are diagnostic of glomerular bleeding, which usually occurs in acute or chronic glomerulonephritis.
a.Crystals may be indicative of renal stone disease.
b.Large numbers of RBCs (especially in the presence of dysuria) may indicate acute hemorrhagic cystitis, which may result from bacterial infections, viral infections (e.g., adenovirus), or chemotherapeutic agents (e.g., cyclophosphamide).
411
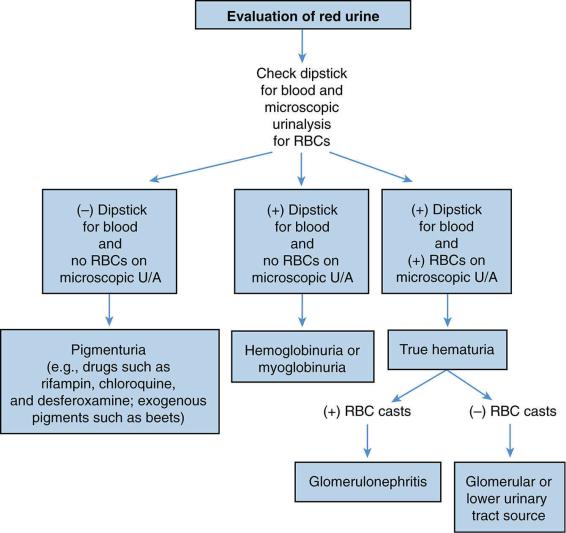
FIGURE 11-1 An approach to red urine. RBC = red blood cell; U/A = urinalysis.
412
413
FIGURE 11-2 Differential diagnosis of hematuria.
414
III.Proteinuria
A.While a small amount of protein is normally present in the urine, proteinuria greater than 100 mg/m2/day or an elevated urine total protein/creatinine ratio are considered pathologic.
B.Detection
1.Urinary dipstick is the most frequently used method of screening for proteinuria and detects variable levels of albuminuria.
a.False positives may result if the urine is very concentrated (specific gravity > 1.025) or alkaline (pH ≥ 7.0), or if the patient has received certain medications (e.g., penicillin, aspirin, IV contrast imaging agents, oral hypoglycemic agents).
b.False negatives may result if the urine is very dilute.
2.Twenty-four–hour urinary protein collection (normal is <100 mg/m2/day) is the most accurate method of detecting proteinuria but is very difficult to obtain in children. Instead, a random spot urine total protein-to-creatinine ratio (TP/CR) is usually performed. An early morning sample correlates well with 24-hour urinary protein excretion.
a.Normal urine TP/CR for infants of age 6–24 months is <0.5.
b.Normal urine TP/CR for children of age >2 years is <0.2.
C.Epidemiology. Up to 10% of children have a single positive dipstick test for proteinuria at some point; however, <1% have persistent proteinuria on repeated dipstick evaluations.
D.Classification
1.Benign transient proteinuria. Increased urinary protein excretion may sometimes be associated with vigorous exercise, fever, dehydration, and congestive heart failure (CHF).
2.Orthostatic proteinuria
a.Certain children and adults (especially athletic individuals) have increased urinary protein excretion while upright but not while supine.
b.Orthostatic proteinuria is usually a benign condition, and its confirmation eliminates the need for further workup.
c.The presence of orthostatic proteinuria is diagnosed with an elevated afternoon urine TP/CR and a normal first morning urine TP/CR.
3.Persistent pathologic proteinuria
a.Persistent pathologic proteinuria may be associated with significant renal disease and is considered a marker for progression of renal disease.
b.Generally, the greater the magnitude of the proteinuria, the more serious the renal disease. The greatest amounts of proteinuria are seen in patients with nephrotic syndrome [see section VI].
c.Persistent pathologic proteinuria may have a glomerular origin or a tubular origin. Glomerular proteinuria is more common.
1.Glomerular proteinuria is caused by increased permeability of the glomerular capillaries to large molecular weight proteins, as seen in glomerulonephritis [see section V] and in minimal change nephrotic syndrome.
2.Tubular proteinuria results from decreased reabsorption of low molecular weight proteins by the tubular epithelial cells, or by the addition of inflammatory proteins to the tubular urine.
a.Examples of tubular proteinuria include interstitial nephritis, ischemic renal injury (acute tubular necrosis, acute kidney injury [AKI]), and tubular damage resulting from nephrotoxic drugs.
b.Laboratory findings include elevated levels of urinary β2-microglobulin,
415
a good marker for tubular proteinuria among others. This small molecule, which is freely filtered at the glomerulus, is normally almost completely reabsorbed by the tubular epithelial cells. Its presence therefore signifies tubular injury. Glucosuria and aminoaciduria may also accompany diffuse injury to the tubular epithelial cells.
E. Evaluation of proteinuria (Figure 11-3)
416
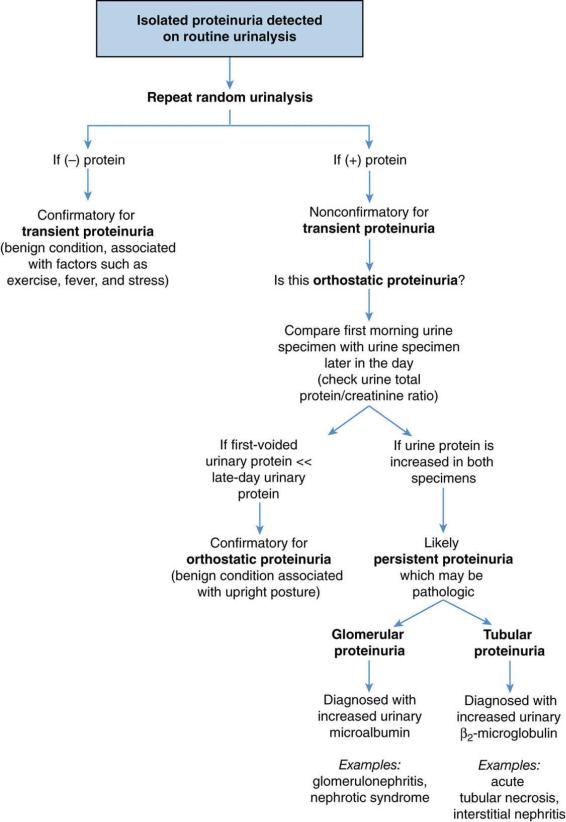
FIGURE 11-3 Evaluation of proteinuria.
417
418
