
- •Foreword
- •Preface
- •Contents
- •1.1 Introduction
- •1.2 Prologue
- •1.9 Expansion of the Greater Omentum
- •3: Distal Gastrectomy
- •4: Total Gastrectomy
- •5.2 Part II: Thoracic Manipulation
- •6: Right Hemicolectomy
- •7: Appendectomy
- •8.6 Internal Pudendal Artery and Its Branches
- •8.13 Lateral Ligament
- •8.16 Fascia Propria of the Rectum: Part II
- •9: Sigmoidectomy
- •13: Hemorrhoidectomy
- •14: Right Hemihepatectomy
- •15: Left Lateral Sectionectomy
- •16: Laparoscopic Cholecystectomy
- •17: Open Cholecystectomy
- •Bibliography
Right Hemicolectomy |
6 |
|
Abstract
Right hemicolectomy is a typical procedure that reverses the embryonic process by which organs are placed in their final positions. It also provides a valuable opportunity for us to view the top and undersides of the fused mesentery. This chapter describes a procedure of ascending colon cancer resection based on the concept of complete mesocolic excision with central vascular ligation proposed by Professor W. Hohenberger [12]. Standard operation time is 2 h.
Keywords
Right hemicolectomy · Lymphadenectomy
Fusion fascia of Toldt
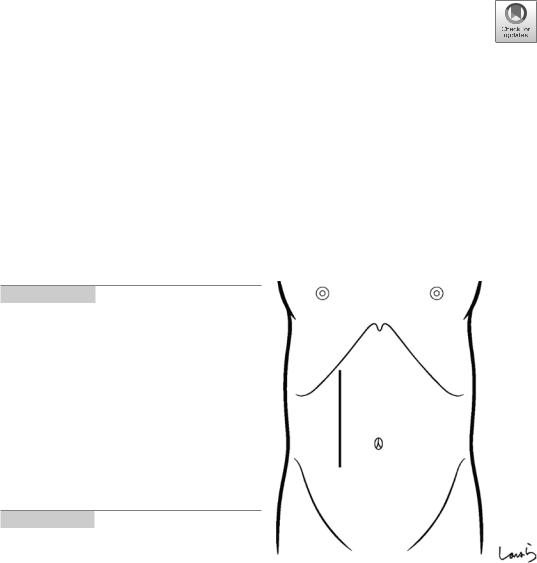
Fig. 6.1 The surgeon stands on the right side of the patient and makes a pararectal incision starting below the costal arch. It would be actually more accurate to say that right hemicolectomy is an upper abdominal surgery
© Springer Nature Singapore Pte Ltd. 2020 |
187 |
H. Shinohara, Illustrated Abdominal Surgery, https://doi.org/10.1007/978-981-15-1796-9_6 |
|

188 |
6 Right Hemicolectomy |
|
|
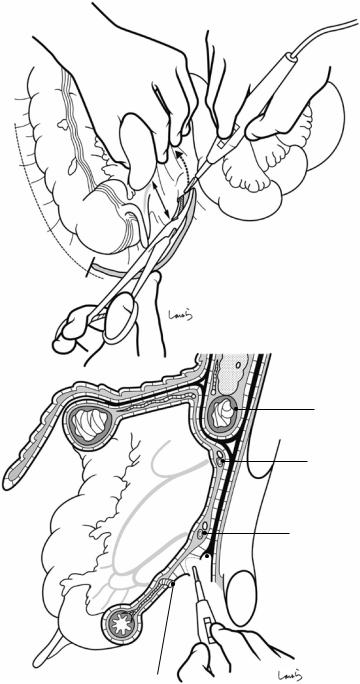
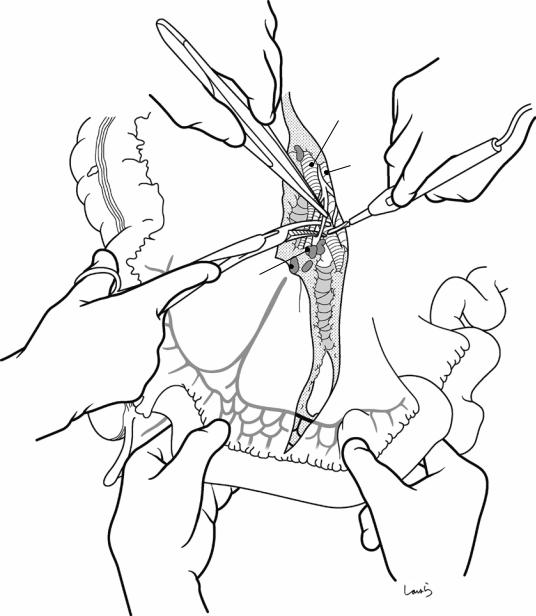
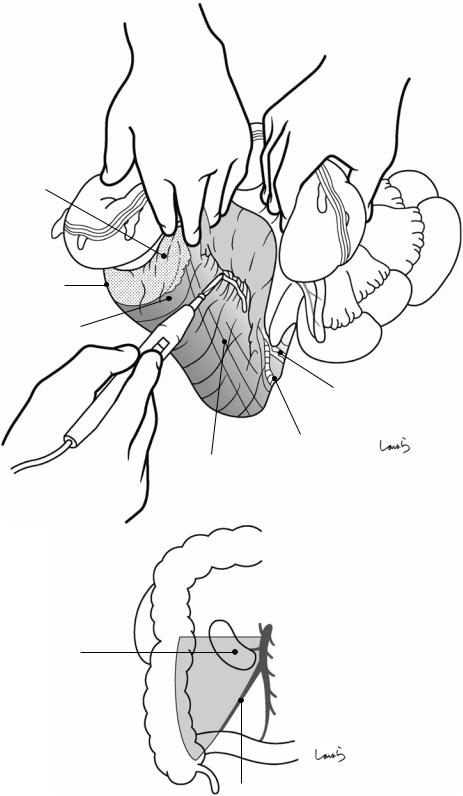
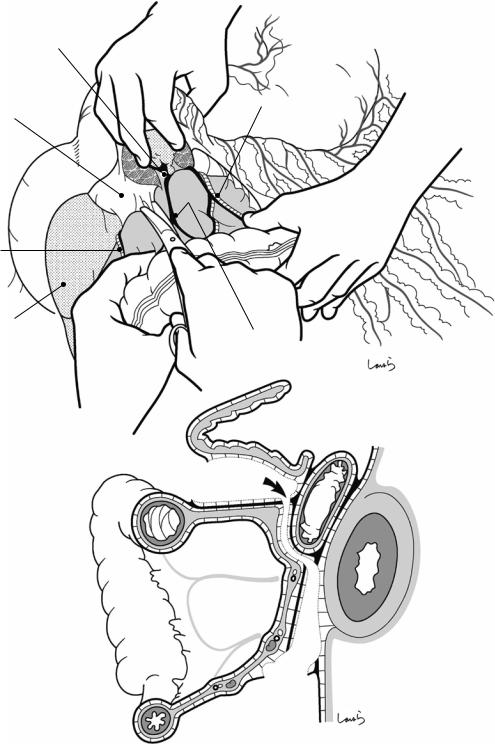
Fig. 6.2 After careful examination of the abdominal cavity, a wound retractor is placed. With the medial
approach, blood vessels are ligated 3 and divided at their root ( 1 ) , and
then the mesentery is detached from the retroperitoneal space as much as possible. This is followed by detachment from the lateral side of the ascending colon ( 2 ) and the transverse colon ( 3 )
2
1
6 Right Hemicolectomy |
189 |
|
|
Fig. 6.3 The boundary between the retroperitoneum and the visceral peritoneum (Monk’s white line) is identified lateral to the cecum and an incision is made using electrocautery along the line but slightly toward the cecum. The incision is extended along the lower margin of the cecum while keeping about 3 cm away from the ileum until the root of mesostenium is incised. The incision is further advanced toward the imaginary dissection line 10–15 cm proximal from the terminal ileum (a). The ileocecal region may be liberated from the retroperitoneum in some patients. Sagittal cross section shows the positional relationship of the incised peritonea (b)
a
Monk's white line
b
Horizontal part of duodenum
R colic a. & v.
Ileocolic a. & v.
 Root of mesentery of small intestine
Root of mesentery of small intestine
Marginal a.
190 |
6 Right Hemicolectomy |
|
|
Mid. colic a. & v.
Horizontal part of duodenum
*
Fig. 6.4 After the small intestine is repositioned to the left lower abdominal cavity, the transverse colon is inverted cranially to spread the mesocolon. The anterior aspect of the horizontal part of the duodenum is seen through the mesocolon. The dotted line between the terminal ileum and the ligament of Treitz represents the root of the mesostenium. A peritoneal incision is made starting from the planned dissection line on the ileum, as mentioned in Fig. 6.3, and ascends to the left of the ileocolic
artery up to the front of the superior mesenteric artery (SMA). The incision is advanced along the left margin of the duodenum and then along the middle colic artery and vein on their right side until the transverse colon is reached. This, combined with the procedure described in Fig. 6.3, results in dissection of the top and undersides of the peritoneum between the ileum and the root of the mesostenium (asterisk) and exposure of the intermediate layer (fat plus two layers of the subperitoneal fascia)
6 Right Hemicolectomy |
191 |
|
|
MCA  (R br.)
(R br.)
Acc. rt. colic v.
SMV
RCA
ICA
Root of mesentery (cut)
Crescent-shaped defect of peritoneum
MCA (L br.)
MCA (root)
SMA |
J1 |
|
J2
J3
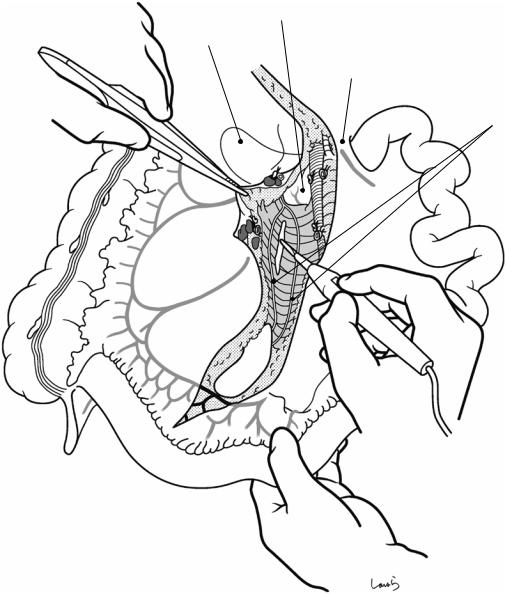
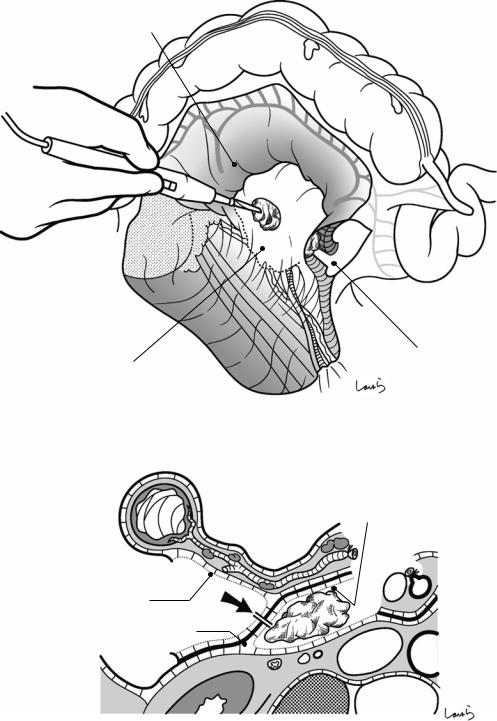
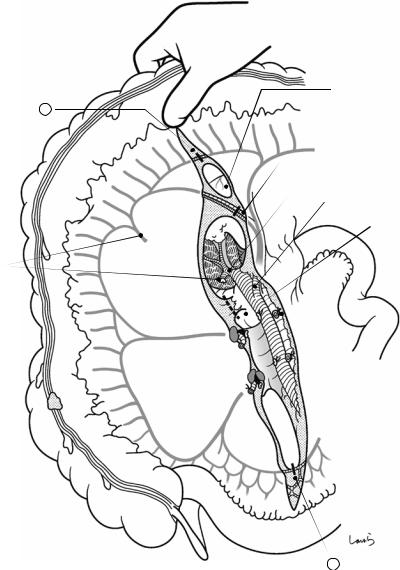
Fig. 6.5 After completing the peritoneal incision, an incision is made in the avascular part of the intermediate layer of the mesoileum at a certain distance from the intestinal wall. Through the crescent-shaped defect of the peritoneum created by the peritoneal incision, we can identify the middle colic artery (MCA), right colic artery
(RCA), and ileocolic artery (ICA) in that order from the top. We can also see the superior mesenteric vein (SMV) in a slightly deeper layer. Note that the right colic artery and vein are located cranial to the horizontal part of the duodenum, as shown, although these vessels are absent in most cases, as described in Fig. 6.7
192 |
6 Right Hemicolectomy |
|
|
SMV
SMA
No.203 
Fig. 6.6 The ileocolic artery and vein are dissected at their root. As shown, after the nerve bundle clinging to the artery is dissected with electrocautery and the lymph nodes around the root of the ileocolic artery and vein (No. 203) are dissected as they remain in the resection side, the exposed artery is ligated and divided and then the vein is ligated and divided. Attention must be paid to the course of the ileocolic artery because although it usually crosses the SMV ventrally as shown, it may dive into the dorsal side of the SMV in some cases, with the true root of the ileocolic artery located
behind the SMV, and this requires more careful manipulation
The SMV connecting between the ileocolic vein and the gastrocolic trunk of Henle is the most important vessel responsible for venous return in the area extending from the small intestine to the right colon. Damaging this vein, which is also referred to as “surgical trunk,” necessitates complicated repair techniques and can even be life- threatening. Although right hemicolectomy itself is not such a complicated procedure, the utmost care should be taken when ligating the surgical trunk

6 Right Hemicolectomy |
193 |
|
|
a
Ileocolic v. (root)
Ilecolic a. (root)
No.213
No.203
b |
c |
¼ of cases |
¾ of cases |
Fig. 6.7 Dissection of the right colic artery and vein at their root and the No. 213 lymph nodes are performed in the same way (a). Again, usually, the right colic artery
runs on the ventral side and the vein on the dorsal side. However, the artery is present in only about 1 out of 4 patients (b) and so is absent in most cases (c)
194 |
6 Right Hemicolectomy |
|
|
Ascending part of duodenum
Horizontal part of duodenum
Lig. of Treitz
Fusion fascia of
Toldt (divided)
No.213
No.203
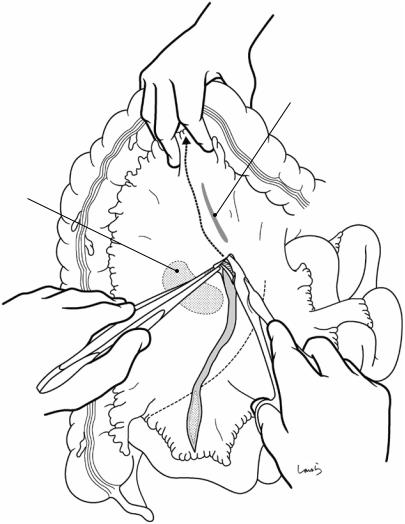
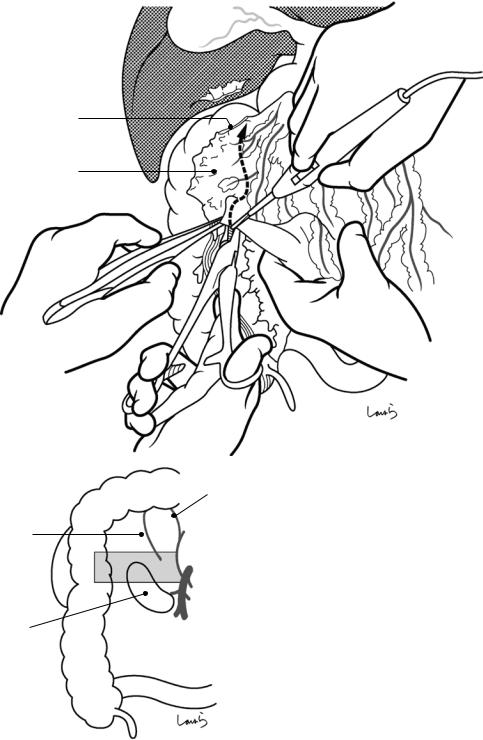
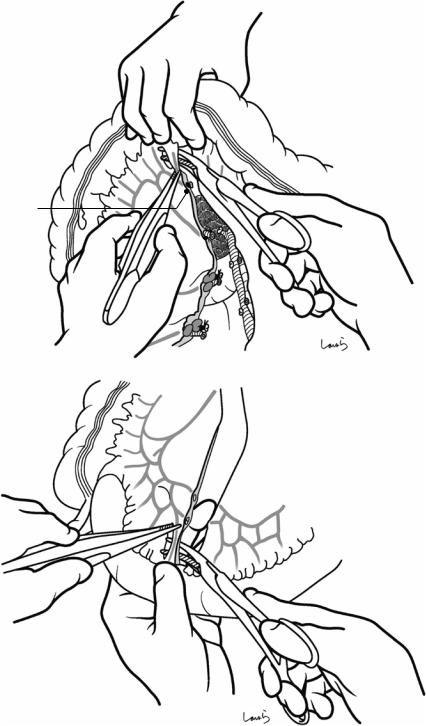
Fig. 6.8 When the vascular dissection is completed, the mesentery is dissected. Once the cut edge of the peritoneum is everted with forceps, as shown, the loose connective tissue is stretched and the cotton-like mesenteric base
is exposed. Because the fusion fascia of Toldt is inadvertently incised during lymph node dissection around vascular roots, the first layer accessed with electrocautery is usually the layer below the fascia
6 Right Hemicolectomy |
195 |
|
|
|
Lieocolic a. |
|
Fascia of |
Fusion fascia |
No.203 |
Gerota |
of Toldt |
|
a |
b |
Ascending |
|
colon |
|
Monk’s white line
|
|
vertebrae |
|
Psoas m. |
Fascia transversalis |
|
|
|
Route a |
RCA |
Route b |
|
|
|
|
No.203 |
|
ICA |
|
SMV |
Mesostenium
SMA
Root of mesentery of small intestine
IMA
L colic a.
Fusion fascia  of Toldt
of Toldt
Subperitoneal fascia
L ureter
L gonadal a. & v.
Fusion fascia of Toldt (divided)
When entering into the layer above the fusion fascia of Toldt with no rupture of the fascia
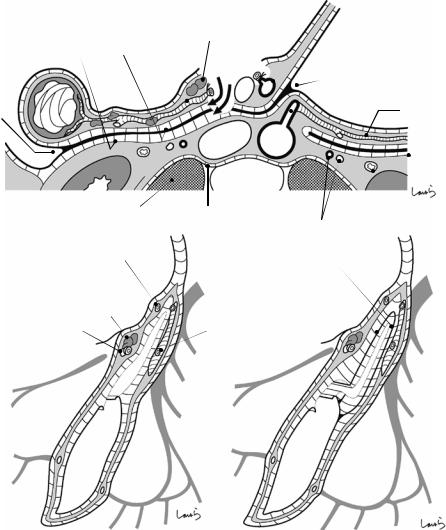
Fig. 6.9 This computed tomography (CT) cross section allows for a detailed explanation of the procedure. Arrow (a) indicates the route of entry into the layer above the fusion fascia of Toldt without rupturing the fascia. Although this route is precise enough for lymph node
When entering into the layer above the fusion fascia of Toldt with rupture of the fascia
dissection, the fusion fascia of Toldt will most likely be ruptured during the dissection process. So, it is easier to enter the layer below the fascia, making Route (b) the first choice

196 |
6 Right Hemicolectomy |
|
|
a
Fusion fascia of Toldt
Gonadal a. & v.
Ureter
b
Ascending colon
Subperitoneal fascia
Horizontal part of duodenum
SMV
Fusion fascia of Toldt
 SMA
SMA
Ureter Gonadal a. & v. Subperitoneal fascia
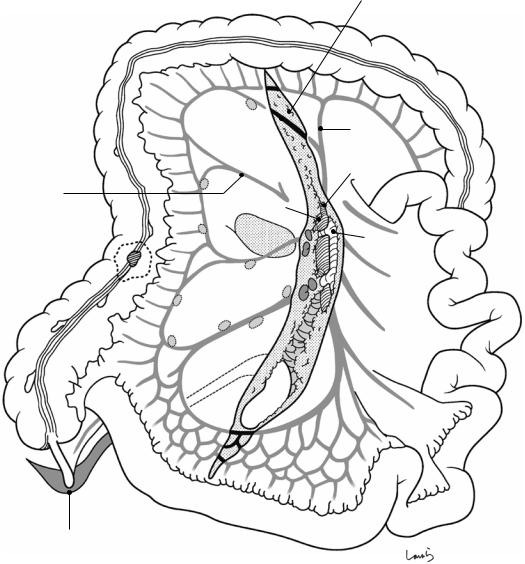
Fig. 6.10 The mesentery is dissected toward the lateral side while keeping to Route (b) seen in Fig. 6.9. The presence of the fusion fascia of Toldt over the dissection surface provides reassurance that a cancerous lesion can be completely removed, wrapped in the fascia. Note that the subretroperitoneal fascia is under the dissection surface
(a). This thin membrane continues from the fascia of Gerota and suspends the ureter and gonadal artery and vein. These structures need to be detached from the membrane with care. The dissection is advanced up to the vicinity of the ureter, at which point a sheet of stretched gauze is placed. CT cross section shows the dissection route (b)
6 Right Hemicolectomy |
197 |
|
|
a |
Hepatocolic lig. |
Monk’s white fine
b
Gauze
Monk’s white line
Fig. 6.11 At this point, the mesenteric dissection is stopped halfway and started over from the lateral side (a). The boundary between the retroperitoneum and the visceral peritoneum (Monk’s white line) is identified lateral to the ascending colon, and an incision is made along the line but slightly toward the colon (b). Layer separation proceeds smoothly when starting the procedure around the right colic flexure. The incision is advanced until it reaches the peritoneal incision made earlier
in the surgery (see Fig. 6.3); it is only a moment before the two incisions are connected because the ascending colon is often shorter than expected (about 15 cm long)
Around the right colic flexure, the right extension of the greater omentum may be adherent to the diaphragm (as the left phrenicocolic ligament) or the underside of the liver (as the hepatocolic ligament). If present, these structures should be dissected early with electrocautery
198 |
6 Right Hemicolectomy |
|
|
a
Fascia of Gerota seen through fusion fascia of Toldt
Monk’s white line
Fusion fascia of Toldt
R ureter
R gonadal a. & v.
Psoas m.
b
Horizontal part of duodenum
Ileocoilc a. & v.
Fig. 6.12 The mesentery is dissected while displacing the colon (a). Entering from the intestinal side of the Monk’s white line ensures that the dissection is advanced in the layer above the fusion fascia of Toldt. Area of the dissection (b)
6 Right Hemicolectomy |
199 |
|
|
a
Fascia on back side of mesocolon
|
Mesocolon dissected |
Fusion fascia of Toldt |
via medial approach |
b
Fusion fascia of Toldt
Fascia on back side of mesocolon
Incision
Fusion fascia of Toldt
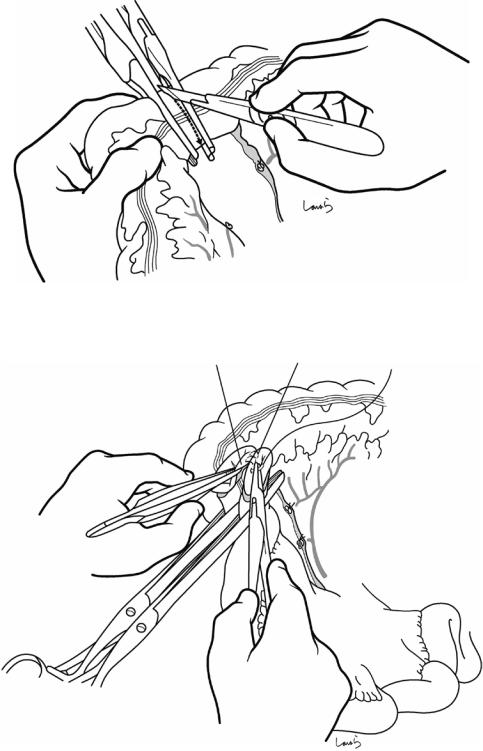
Fig. 6.13 When the dissection advances past the major psoas muscle, the gauze placed earlier (see Fig. 6.10) is seen through the fascia (a). By incising this with electro-
cautery, the mesenteric dissections from both directions are connected and the penetration of the tunnel is achieved (b)
200 |
6 Right Hemicolectomy |
|
|
a
Cut end of hepatocolic lig.
Omentocolic lig.
b
R branch of mid. colic a. & v.
Acc. rt. colic v.
Horizontal part of duodenum
Fig. 6.14 Next, the part of the right transverse mesocolon colliding with the anteroinferior part of the pancreas and duodenum is released (a). Area of the dissection (b). The right edge of the greater omentum is, in most cases, adherent to the upper portion of the ascending colon (as
the omentocolic ligament). In cases where the cancerous lesion is localized to the lower half of the ascending colon or has not invaded the serosa, allowing preservation of the greater omentum, this adhesion should be dissected with electrocautery before proceeding with the operation
6 Right Hemicolectomy |
201 |
|
|
a |
Descending part of duodenum |
Transverse
mesocolon
Acc. R colic v.
Descending part
of duodenum
b
Fusion fascia
Fusion fascial of Treitz
RCA |
|
|
ICA |
|
Subperitoneal |
|
* |
fascia |
|
(Fascia of |
|
|
|
|
|
|
Gerota) |
Fusion fascia of Toldt
Marginal a.
Fig. 6.15 The greater omentum is detached from the right transverse mesocolon (a). This procedure is the reverse of the gastrectomy procedure shown in Fig. 3.12, but it is performed in the same dissection layer. When the middle colic artery is to be preserved, there is no need to advance the dissection across the right border of the
omental bursa. The route for omental dissection (b). Compared with the schematic diagram of Fig. 6.3, the ascending mesocolon is already separated from the abdominal wall (asterisk) and the only remaining procedure is to release the connection with the horizontal part of the duodenum
202 |
6 Right Hemicolectomy |
|
|
a
Gastrocolic trunk of Henle
Horizontal part of duodenum
R colic
a.& v.
Facia of Gerota
b
Mid. colic a. & v.
Acc. R colic v.
Fig. 6.16 The transverse mesocolon is detached from the horizontal part of the duodenum using Cooper scissors (a). Dissection route on a sagittal cross section (b)

6 Right Hemicolectomy |
203 |
|
|
a
R br. of
mid. colic a. & v.
Acc. R colic v.
 Ileocolic a. & v.
Ileocolic a. & v.
b |
R gastropiploic v. |
PV |
Acc.R colic v.
Transverse colon
R br. of mid. colic a. & v.
SMA
Henle
Horizontal part of duodenum
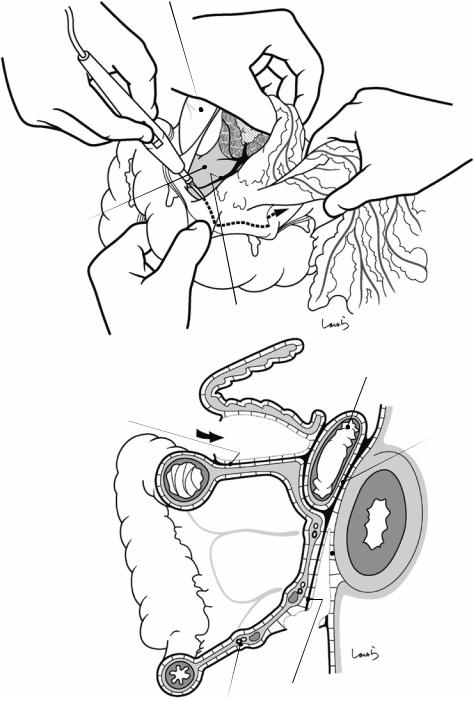
Fig. 6.17 The accessory right colic vein, which drains into the gastrocolic trunk of Henle, is ligated and divided. The transverse mesocolon widely covers the anterior aspect of the pancreatic uncinate process from the lower side (b), making the base of the mesocolon flabby and considerably thick. The accessory colic vein and the middle
colic vein, which both drain the colon, run over the top and bottom surfaces of the mesocolon, respectively. Now the release of fixation of the right colon by reverse play is completed. Two openings are made with electrocautery on the transverse mesocolon on both sides of the right branch of the middle colic vessels (two dotted ellipses in a)
204 |
6 Right Hemicolectomy |
|
|
Duodenal bulbus
1
R br. of mid. colic a.
Root of mid. colic v.
Ascending part of duodenum
Acc. R colic v.
R colic a. (root)
* 
No.213
 Ileocolic a. (root)
Ileocolic a. (root)
No.203
Fig. 6.18 Again, the mesocolon is widely expanded as described in Fig. 6.5. Any residual adhesion to the duodenum (asterisk) should be dissected. The right branch of
2
the middle colic vessels ( ) and the marginal artery and vein near the planned dissection lines on the colon and ileum ( ) are ligated and divided
6 Right Hemicolectomy |
205 |
|
|
|
|
a |
Trimming of colon |
|
Marginal a. (cut)
R br. mid.  colic a.(cut)
colic a.(cut)
b |
Trimming of ileum |
Fig. 6.19 Straight arteries and veins are trimmed around the planned transection lines of the colon (a) and ileum (b). The mesoileum contains multiple loops of marginal arteries and veins and, to compensate for this, more
numerous but shorter straight arteries and veins than in the mesocolon. Moreover, the presence of thicker mesenteric fat near the ileal wall makes trimming of this area more difficult than trimming of the jejunal area
206 |
6 Right Hemicolectomy |
|
|
Intestinal clump
Stump clump
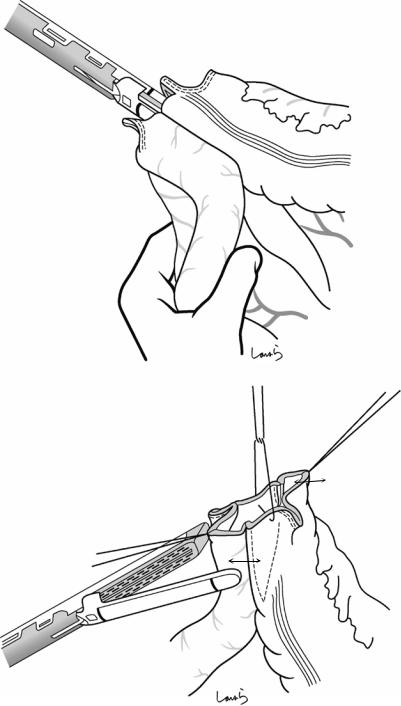
Fig. 6.20 An intestinal clamp and a stump clamp are placed slightly apart from each other and the intestine is transected along the Akiyama-type clamp with a pointed blade
Fig. 6.21 Ileotransversostomy is performed with an Albert-Lembert suture. End-to-end anastomosis can be achieved even between stumps of different diameters if the difference is not too great
6 Right Hemicolectomy |
207 |
|
|
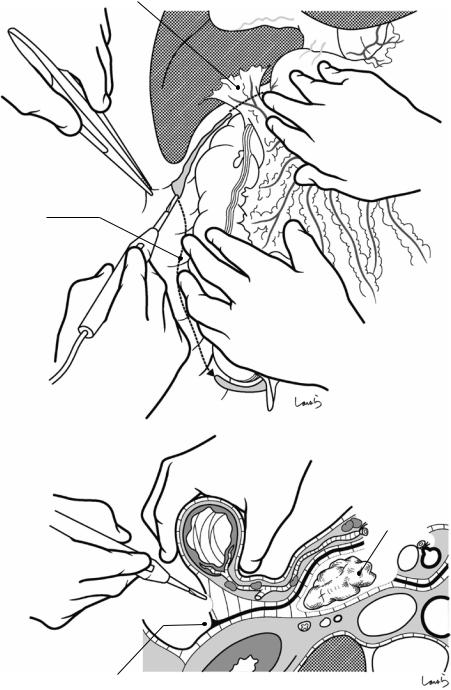
Fig. 6.22 An easy-to- perform alternative is functional end-to-end anastomosis with a linear stapler. After the colon and ileum have been transected with the stapler, small openings are made on the wall of each intestine contralateral to the mesentery. Another linear stapler is placed through the openings and fired to form a V-shaped anastomotic orifice (a). Two stay sutures are placed orthogonally 1 cm away from the staple lines along which the intestines were transected and are pulled in opposite directions. With these two sutures and another stay suture placed at the midpoint, the opening is lifted and closed using a final linear stapler (b), forming an anastomosis with four staple lines slightly apart from each other
a
b
1cm
1cm
208 |
6 Right Hemicolectomy |
|
|
L br. of mid. colic a. & v.
Horizontal part of duodenum covered
by mesentery
R paracolic gutter
 Ileal a. & v.
Ileal a. & v.
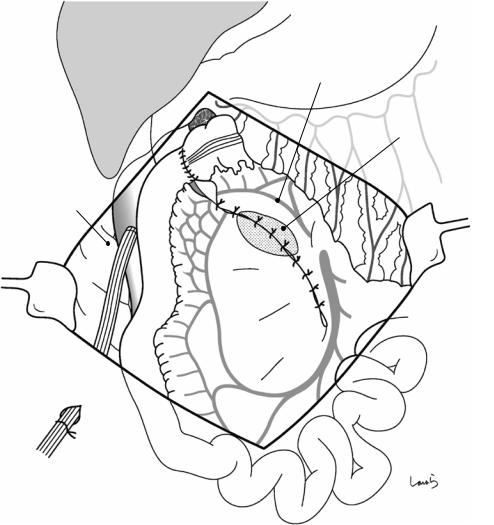
Fig. 6.23 The mesentery is closed with interrupted 3-0 Vicryl sutures. The peritoneal defect in the right lateral abdomen is filled with the anastomosed ileum placed in its natural form. After washing the abdominal cavity, an
8-mm duple drain is placed in the right paracolic gutter and the operation is completed by closing the abdominal wall, suturing in three layers
