
- •Foreword
- •Preface
- •Contents
- •1.1 Introduction
- •1.2 Prologue
- •1.9 Expansion of the Greater Omentum
- •3: Distal Gastrectomy
- •4: Total Gastrectomy
- •5.2 Part II: Thoracic Manipulation
- •6: Right Hemicolectomy
- •7: Appendectomy
- •8.6 Internal Pudendal Artery and Its Branches
- •8.13 Lateral Ligament
- •8.16 Fascia Propria of the Rectum: Part II
- •9: Sigmoidectomy
- •13: Hemorrhoidectomy
- •14: Right Hemihepatectomy
- •15: Left Lateral Sectionectomy
- •16: Laparoscopic Cholecystectomy
- •17: Open Cholecystectomy
- •Bibliography

5.2 Part II: Thoracic Manipulation |
153 |
|
|
5.2\ Part II: Thoracic Manipulation
III
IV
V
M axillary line
Anterior border of latissimus dorsi
Pillow
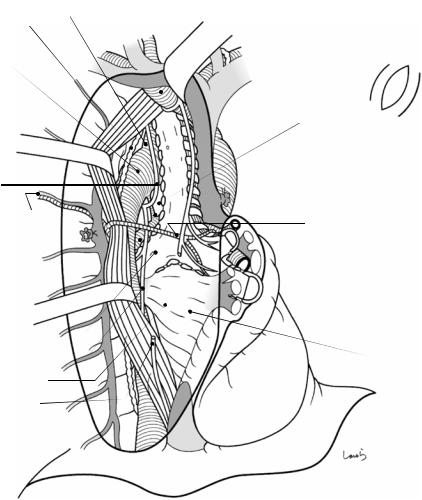
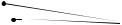
Fig. 5.20 The patient is repositioned to left lateral recumbency and the right arm is immobilized, with the axillary angle slightly obtuse and the elbow at a right angle. A pillow is placed under the patient, below the lower border of the scapula. The thoracotomy procedure is described in detail here because gastrointestinal surgeons are not generally familiar with it
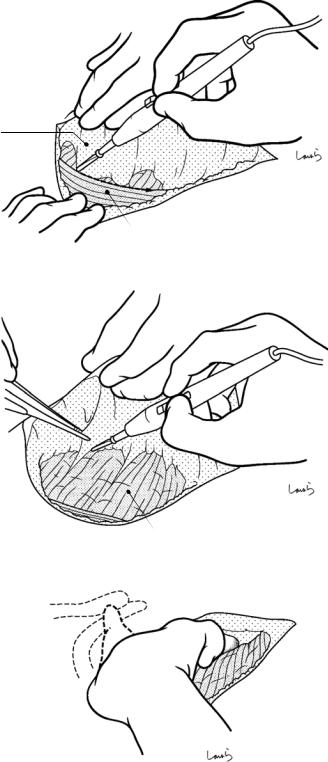
The surgeon stands on the back side of the patient and makes an anterior axillary incision for thoracotomy through the fourth intercostal space. First, the third rib needs to be identified. As the ribs are palpated from upper to lower along
the midaxillary line, the groove suddenly gets deeper and becomes less easily palpable at a certain point. The last palpable rib is the third one. A skin incision is made along the arc extending from the intersection of the third rib and the midaxillary line, through a point one-finger medial from the anterior border of the latissimus dorsi (palpable as a bulge) and then anteroinferiorly toward the fifth intercostal space. In female patients, note that care is needed to avoid damaging the mammary gland. If excessive tension occurs, the curved line may be slightly extended anteriorly from the intersection of the third rib and the midaxillary line
154 |
5 Ivor Lewis Esophagectomy: A Curative Operation for Esophageal Cancer |
|
|
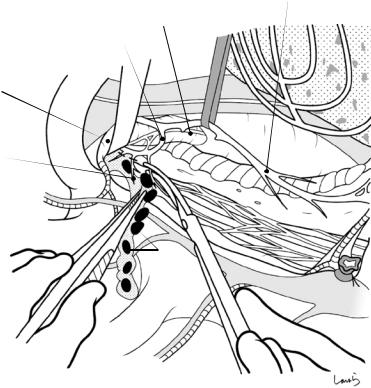
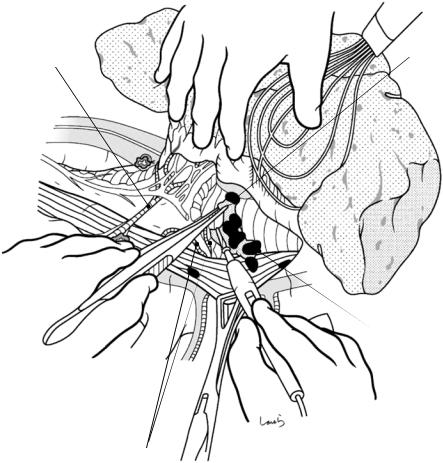
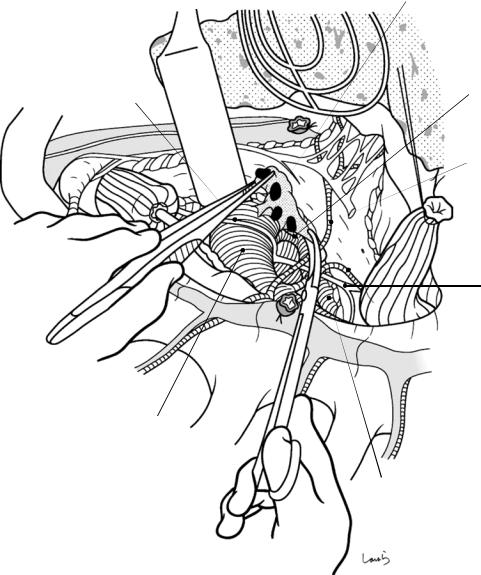
Fig. 5.21 In the fourth intercostal space, the subcutaneous tissue (on the anterior side) and the latissimus dorsi (on the posterior side) are detached from the fascia of the serratus anterior using electrocautery (a). Once the serratus anterior is exposed (b), the location of the intercostal space to be opened should be confirmed again. The hand is advanced cranially along the thoracic wall and bumps into the clavicle and the first rib (c). The hand is then advanced backward while palpating the second and third ribs. The third and lower ribs are aligned nearly horizontally. Subsequently, the fourth and fifth ribs are palpated
a
Subcutaneous
tissue
Latissimus dorsi
b
Serratus anterior
c
Clavicle
1st rib
5.2 Part II: Thoracic Manipulation |
155 |
|
|
Fig. 5.22 Starting from the upper border of the fifth rib, the serratus anterior is incised longitudinally along the muscle bundles. The left index and middle fingers are inserted between the serratus anterior and thoracic wall to lift the muscle, and the muscle bundles are divided with electrocautery (a). On the posterior side, the latissimus dorsi is retracted with a flat spatula and the incision is advanced dorsally. When the thoracodorsal artery and vein are encountered under the latissimus dorsi, these vessels should be ligated and divided (b)
a
Serratus anterior 
Latissimus dorsi 
b
Thoracodorsal a. & v. 
Pectoralis major
IV
V
VI
156 |
5 Ivor Lewis Esophagectomy: A Curative Operation for Esophageal Cancer |
|
|
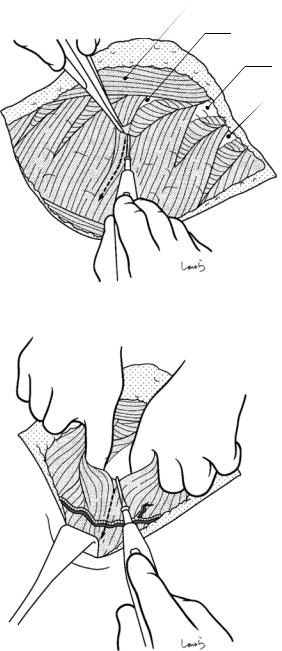
Fig. 5.23 After one-lung ventilation has been established and the right lung has been collapsed, a thin layer of the external intercostal muscle is dissected using electrocautery, starting from the upper border of the fifth rib (a). Then, thin layers of the internal intercostal muscle and the innermost intercostal muscle are scooped with dissection forceps and divided to expose the parietal pleura (b). After confirming the absence of adhesion between the lung and the pleura, a small area of the pleura is grabbed with forceps and incised with a pointed blade (c). Then, after access to the thoracic cavity has been confirmed, the pleural incision is extended using Metzenbaum scissors
a
IV
Ext. intercostal m.
V
Int intercostal m.
b
V
c
Parietal pleura
5.2 Part II: Thoracic Manipulation
Fig. 5.24 The incision of the intercostal muscles and parietal pleura is extended in the anterior and posterior directions using electrocautery. After the incision has proceeded to a certain extent, a small rib retractor is placed to gradually widen the wound as the incision continues, while the first assistant protects the lung with gauze held with forceps (a). When the anterior incision approaches the costochondral junction, the incision is oriented superiorly and continued slightly beyond that area. The posterior incision is extended up to the costal angle, which is about 5 cm away from the vertebra (b)
a
Int./ext. intercostal m.
b |
Costal cartilages |
Vertebra 
157
Small rib retractor
158 |
5 Ivor Lewis Esophagectomy: A Curative Operation for Esophageal Cancer |
|
|
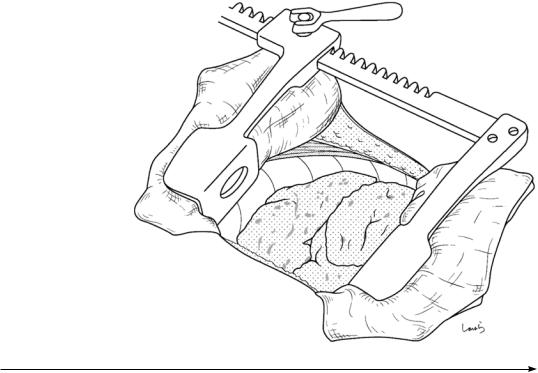
Fig. 5.25 The small rib retractor is removed, the upper and lower ribs are protected with a surgical laparotomy sponge, and
a large rib retractor is
placed. We can avoid rib Large rib retractor fracture by slowly
turning the retractor handle and widening by one increment at a time. Further widening may be achieved by allowing a longer interval between handle turns. Usually, a wound of 10–12 cm width can be obtained this way
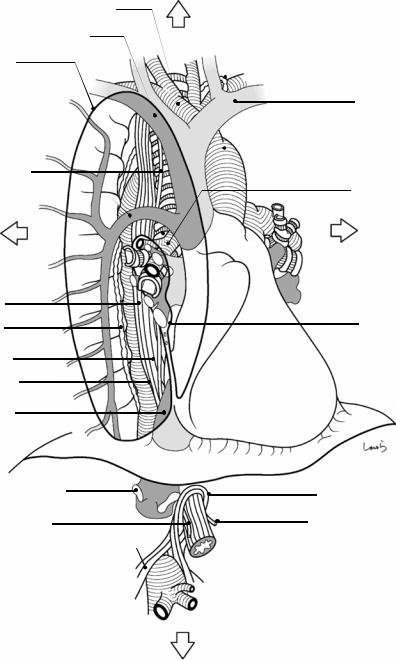
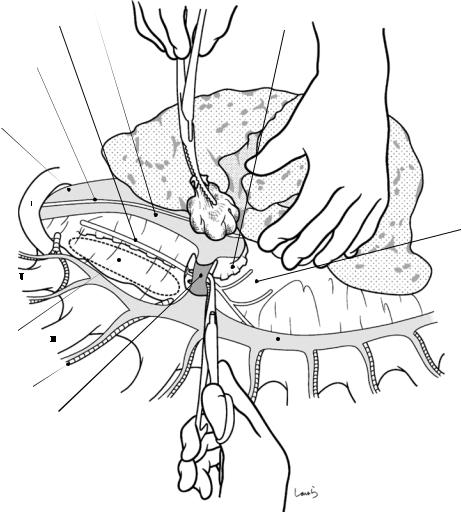
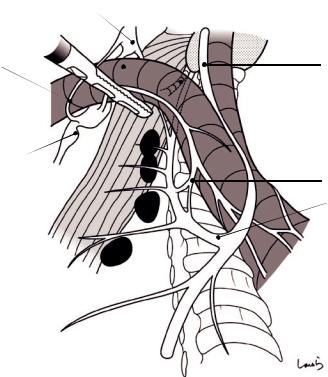
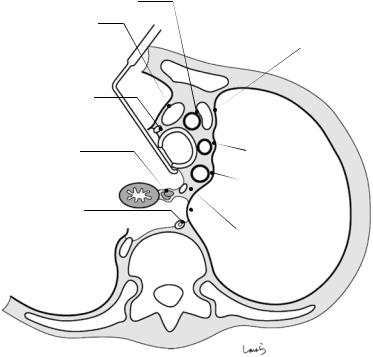
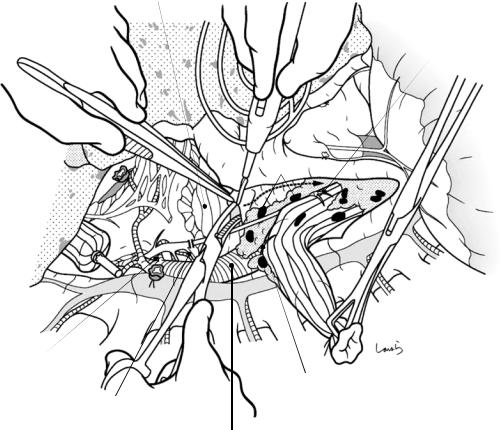
Fig. 5.26 Before going any further, let us quickly review the anatomy of the mediastinum. The vessels, trachea, and esophagus in the mediastinum form a complicated threedimensional crossover structure like a highway junction, and their positional relationship varies depending on the angle from which they are viewed. Also, during esophageal surgery, a “twist” can occur and cause anterior-poste- rior and/or left-right reversal of their positions. For example, when using a regular right thoracotomy approach, we tend to assume that we have a view of the mediastinum from the exact right side. However, once the right lung is retracted anteriorly through thoracotomy, then we will be viewing the mediastinum from its posterior side. Also, when the hilum of the right lung is significantly displaced (“twisted”) by releasing the “tension” generated by the azygos vein, the posterior aspect (membranous part) of the trachea and the dorsal surface of the heart are exposed, and eventually the posterior aspects of the left bronchus and vessels constituting the left hilar vasculature, such as the left inferior pulmonary vein. Because dissection of lymph nodes in the left side of the superior mediastinum (e.g., No. 106-recL, 106-tbL, and 109-L) is required during esophageal cancer surgery, we need to get used to the uncomfortable feeling of “viewing the posterior side of the left mediastinum through a right thoracotomy”
This and subsequent illustrations of the mediastinum (Figs. 5.26–5.28) are designed to help surgeons perform image training, where the mediastinum is placed vertically (in its natural position) in a fixed right oblique frontal view, which most clearly shows the entire
three-dimensional crossover structure, with small increments of “twist” applied
In this first figure in the series, we see the non-twisted state. The right lung is cut off at the hilum. The mediastinum, which is seen through the parietal pleura after right thoracotomy, corresponds to the area surrounded by the thick line (note: the parietal pleura in this area is specifically referred to as the mediastinal pleura). In the hilum of the right lung, the right principal bronchus, right pulmonary artery, right superior pulmonary vein, and right inferior pulmonary vein are located in that order from the cranial side. The pleura between the right inferior pulmonary vein and the diaphragm forms a fold, also referred to as the pulmonary ligament, that anchors the inferior lobe of the right lung to the mediastinum. The azygos vein, after collecting blood from intercostal veins, travels transversely above the right principal bronchus and drains into the superior vena cava. The aortic arch seen curving to the left when viewed from the front is seen curving posteriorly when viewed from this angle. In the superior mediastinum, after serving as a pillow for the superior vena cava, trachea, and esophagus, which are aligned in that order from the anterior side, the aorta travels backward toward the thoracic spine (to the left when viewed from the front), then gradually approaches the thoracic spine, and, after passing through the diaphragm, finds itself almost in front of the thoracic spine. The esophagus is pushed by the interposing descending thoracic aorta and gradually proceeds away from the thoracic spine; it is immediately in front of the descending thoracic aorta at the level of esophageal hiatus
5.2 Part II: Thoracic Manipulation |
159 |
|
|
Cranial side
Brachiocephalic a.
R brachiocephalic v.
Mediastinal pleura
I
Upper thoracic
esophagus  II
II
R vagus n.
Arch of azygos
III
Dorsal side
IV
Middle thoracic esophagus
Thoracic duct
Lower thoracic esophagus
Descending thoracic orta
Inf. vena cava
Thoracic duct
L brachiocephalic v. (innominate v.)
Ascending aorta
 Sup. vena cava
Sup. vena cava
R principal bronchus
R pulmonary a.
Ventral side
 R sup. pulmonary v.
R sup. pulmonary v. 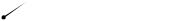 R inf. pulmonary v.
R inf. pulmonary v.
Hilum of R lung
 Pulmonary lig.
Pulmonary lig.
R hepatic v. |
Esophageal opening |
|
|
R vagus n. |
L vagus n. |
Aortic opening |
|
|
Celiac a. |
Caudal side
160 |
5 Ivor Lewis Esophagectomy: A Curative Operation for Esophageal Cancer |
|
|
R brachiocephakic v.
R subclavian a. 
L brachiocephalic v. (innominate v.)
R recurrent n.
R vagus n. 
R principal bronchus
Arch of azygos
R pulmonary a.
Pulmonary br. of R vagus n.
R sup. pulmonary v.
R inf. pulmonary v.
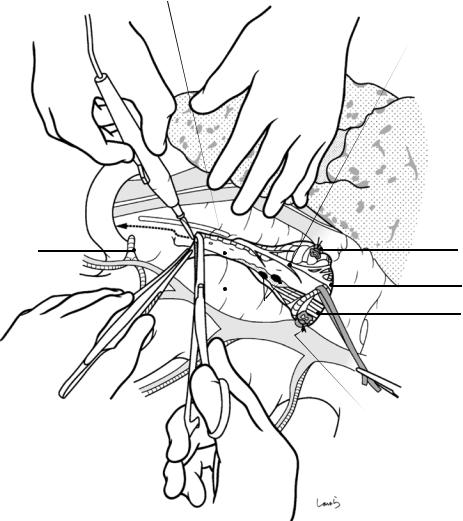
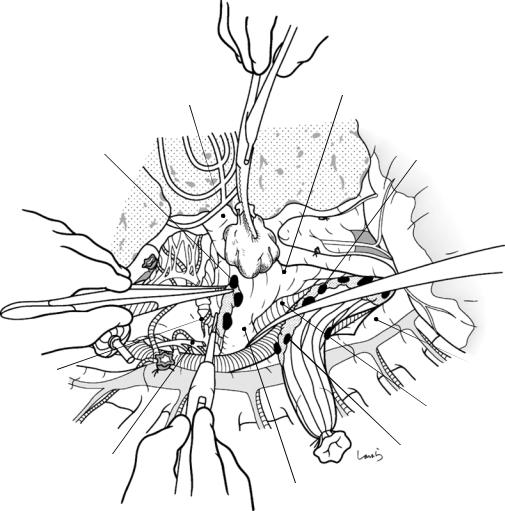
Fig. 5.27 In this second figure in the series, the right lung is retracted anteriorly. This procedure applies a “small twist” to the mediastinum and allows us to see some of the structures in the back side of the hilum of the right lung through the pleura, including the membranous part (posterior wall) of the right principal bronchus and the posterior aspect of the right inferior pulmonary vein (but not the right pulmonary artery or right superior pulmonary vein, which are located more ventrally). This twist means that the membranous part of the lower trachea is also exposed. The azygos vein is extended in length as a result of twist
With this “small twist” being applied, retracting the right brachiocephalic vein cranially allows us to identify
the origin of the right recurrent laryngeal nerve, as shown. The right vagus nerve, after entering the mediastinum, branches off the right recurrent laryngeal nerve beyond the right subclavian artery. This nerve turns around the right subclavian artery and then ascends along the right border of the trachea, making itself looking like a reverse J when viewed from the front, but a normal J when viewed from the angle of this figure as it branches and travels backward. After giving off the right recurrent laryngeal nerve, the main trunk of the vagus nerve descends to the right of the trachea, passes under the azygos vein, and then descends along the esophagus. On the way, it also gives off the pulmonary and cardiac branches
5.2 Part II: Thoracic Manipulation |
161 |
|
|
R subclavian a.
L subclavian a. Thoracic duct
Arch of aorta
L recurrent n.
R 3rd intercostal a.
Azygos v. (divided) 
L pulmonary a.
L principal bronchus
L vagus n.
L inf. pulmonary v.
R vagus n.
Leaf-shaped area (No.106-tbL LN)
 L venous angle
L venous angle
Aortic arch
L pulmonary a.
Leaf-shaped area
Lig. arteriosum
 Azygos v. (divided)
Azygos v. (divided)
R bronchial a.
 R inf. pulmonary v.
R inf. pulmonary v.
Pericardium
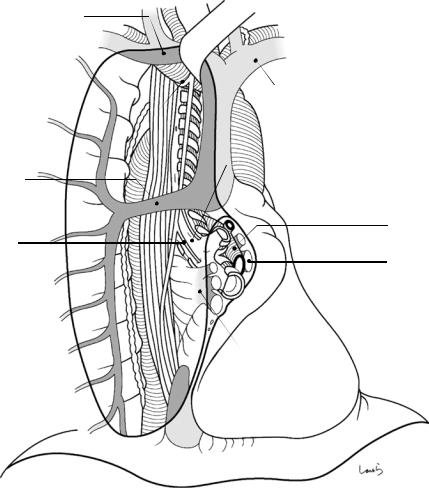
Fig. 5.28 In this third figure in the series, the tension generated by the azygos vein is released and the parietal (mediastinal) pleura is dissected above and below this vein, which applies a “major twist” to the mediastinum. This exposes structures at the back side of the hilum of the left lung, including the membranous part (posterior wall) of the left principal bronchus and the posterior aspect of the left inferior pulmonary vein. When looking at the trachea, it is also partially exposed, ranging from the membranous part to the left border of the tracheal cartilages
Dissecting the azygos vein exposes the hidden right bronchial artery. The right bronchial artery arises from the descending aorta to form a common trunk with the right third intercostal artery, then travels over the esophagus anteriorly, and reaches the right principal bronchus. So, any attempt to further twist the vessel will be hampered at this time by the tension generated by the artery. Retraction of the esophagus posteriorly, taking care not to pull this artery apart, exposes the aortic arch, which has given off the left subclavian artery and entered its descending phase. The left bronchial artery arises directly from the descending aorta and reaches the left principal bronchus. When the leaf-shaped area bordered by the left principal
bronchus and the aortic arch (No. 106-tbL lymph nodes) is burrowed a bit more, the left pulmonary artery and ligamentum arteriosum are encountered
Dissecting the No. 106-tbL lymph nodes exposes the origin of the left recurrent laryngeal nerve. The left vagus nerve, after entering the mediastinum, branches off the left recurrent laryngeal nerve in a reverse J shape, or anteriorly, beyond the aortic arch. This nerve then ascends all the way along the left border of the trachea. Extra care should be taken to avoid damaging this nerve during lymph node dissection in this area (No. 106-recL). The main trunk of the left vagus nerve continues to descend along the esophagus while giving off pulmonary and cardiac branches
Another important vessel in the mediastinum is the thoracic duct, which ascends along the anterior aspect of the vertebrae and enters the thoracic cavity through the aortic hiatus. After traveling a distance upward parallel to the azygos vein, the duct merges to the left at the level of the fifth thoracic vertebra, passes behind the aortic arch and across the left border of the esophagus, and drains into the left venous angle. So, we should be mindful of the thoracic duct behind the upper thoracic esophagus and be sure to identify the duct correctly to avoid damaging it inadvertently during dissection
162 |
5 Ivor Lewis Esophagectomy: A Curative Operation for Esophageal Cancer |
|
|
Sup. vena cava |
|
R vagus n. |
Tracheal cartilage |
|
|
R phrenic n. |
|
R brachiocephalic v. |
|
R principal bronchus
Esophagus visible beneath
R 3rd intercostal a.
Arch of azygos
Azygos v.
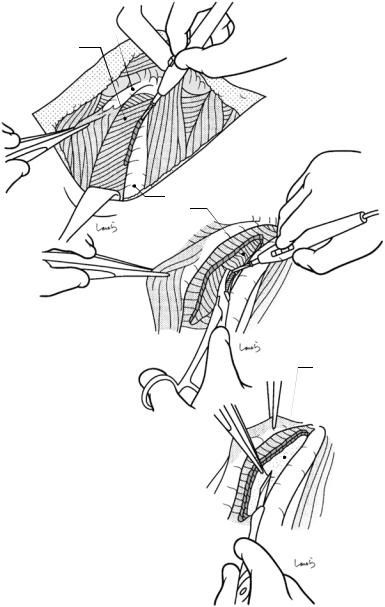
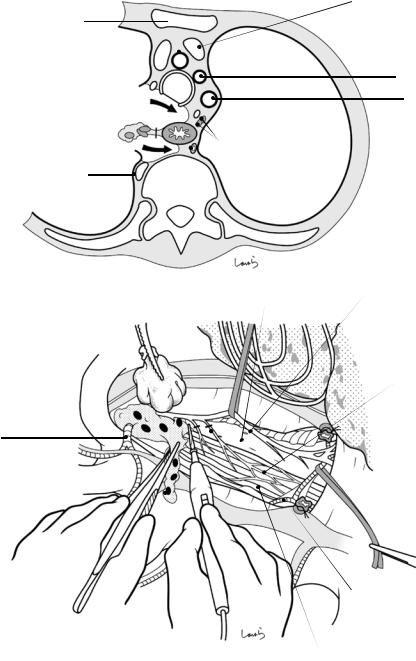
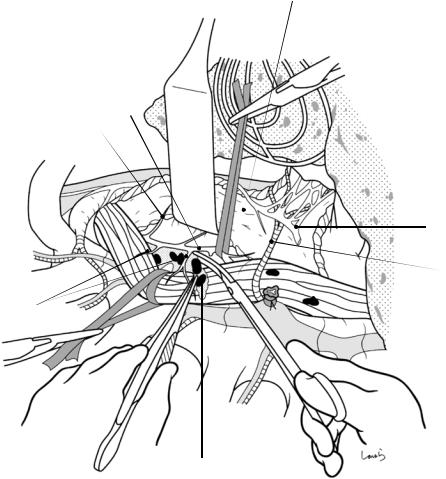
Fig. 5.29 We move on now to mediastinal manipulation. Using the left hand, the first assistant retracts the right lung toward the anterior chest wall, which applies a “small twist” to the mediastinum. A moderately large-sized gauze ball can also be used to retract the lung; this is also useful for developing a focus point
The first step is to transect the azygos vein. The mediastinal pleura is divided along the upper border of the azygos vein with electrocautery. The vein is isolated with right angle dissection forceps, taking care not to damage
the right bronchial artery, which runs right behind on the cranial side of the azygos arch and located very close to the vein. The tip of the forceps is opened slowly to secure a sufficient margin for transection, followed by ligation and division of the vein.
Immediately after transection of the azygos arch, the right bronchial artery is identified and taped without detaching the surrounding supportive tissue. This artery should be preserved as much as possible to maintain blood flow to the trachea
5.2 Part II: Thoracic Manipulation |
163 |
|
|
Trachea
R vagus n.
R sup. intercostal a. |
Azygos (divided) |
|
R bronchial a. |
No.105 LN |
Esophagus |
Azygos (divided)
Parietal pleura in sup. mediastinum
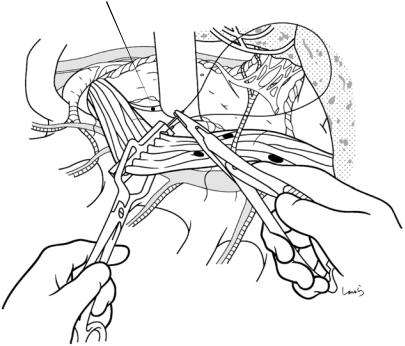
Fig. 5.30 Dissection should be started from the superior mediastinum. The mediastinal pleura is divided along the esophagus between the stump of the azygos arch and the right subclavian artery. The right vagus nerve, which
descends along the surface of the tracheal cartilage, is seen through the membrane as a cord-like structure as thick as the lead of a colored pencil
164 |
5 Ivor Lewis Esophagectomy: A Curative Operation for Esophageal Cancer |
|
|
a
Brachiocephalic a.
R brachiocephalic v.
R vagus n. 
 L recurrent n.
L recurrent n.
No.105 LN
No.106-recL LN
R sup. intercostal v.
Thoracic duct
b |
Esophageal br. of vagus n. |
Trachea |
|
|
R sup. intercostal a.
Dissected No.105 LN |
Vertebra |
|
L brachiocephalic v.
(innominate v.)
L common carotid a.
L subclavian a.
R vagus n.
Esophageal plexus
3rd intercostal a.
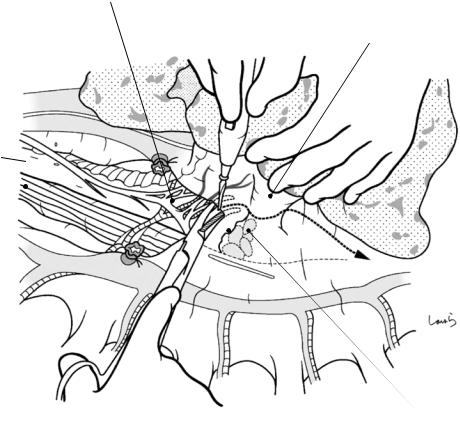
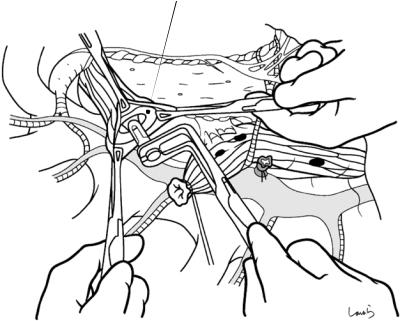
Fig. 5.31 This pleural incision causes a “small twist” to the superior mediastinum (a). While the fatty connective tissue containing the upper thoracic paraesophageal lymph nodes (No. 105) is being dissected from caudal to cranial with electrocautery, the esophagus is detached from the membranous part of trachea and the anterior aspect of the vertebrae. Several esophageal branches arise
from the right vagus nerve and merge with esophageal branches from the left vagus nerve and sympathetic nerves to form the esophageal plexus. These branches should be identified and dissected (b). If metastasis to the No. 105 lymph nodes is suspected, remove the right bronchial artery together with the lymph nodes
5.2 Part II: Thoracic Manipulation |
165 |
|
|
|
|
a |
R vagus n. |
|
Inf. cardiac n. |
||
|
||
|
R subclavian a. |
|
R subclavian a. |
|
Esophageal 
br.
No.106-rebR LN
No.105 LN
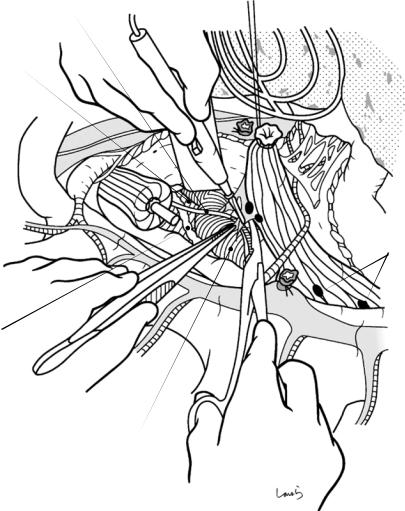
Fig. 5.32 When the right subclavian artery is reached, dissection is continued along the artery from proximal to distal (a). When the vessel tape placed around the right vagus nerve is gently pulled caudally, the right recurrent laryngeal nerve can be identified as it turns around and dives into a deeper layer while winding around the artery. After the fatty connective tissue containing the lymph nodes around the right recurrent laryngeal nerve (No. 106-recR) has been carefully removed, the fatty connective tissue is pulled caudally to further proceed with dissection around the esophagus and removed along with the No. 105 lymph nodes dissected in the previous step. Avoid the use of electrocautery around the recurrent laryngeal nerve and use Cooper scissors instead The anatomy of the right recurrent laryngeal nerve (b). After branching from the right vagus nerve, the right recurrent laryngeal nerve travels along a curved path toward the posterior side of the right subclavian artery and then ascends along the groove between the trachea and esophagus while making contact with the inferior thyroid artery. On the way, the nerve
gives off three to four branches to the esophagus. In this area, keep in mind the anatomy of sympathetic nerves. The cervical sympathetic trunk descends over the anterior surface of the vertebrae and connects to the thoracic sympathetic trunk. The inferior cervical ganglion of the former trunk is usually fused with the first thoracic ganglion, forming a larger ganglion referred to as the stellate ganglion. The inferior cardiac nerve, originating from the stellate ganglion, descends clinging to the posterior surface of the right subclavian artery and enters the cardiac plexus. On the way, it may give off a communicating branch to the recurrent laryngeal nerve, as shown in (b)
The No. 106-recR lymph nodes are mostly located behind the recurrent laryngeal nerve. Dissection should proceed while confirming that the esophageal branches of the recurrent laryngeal nerve are distributed to the esophagus and confidently pushing aside these branches with Metzenbaum scissors (some amount of bravery is required though)
166 |
5 Ivor Lewis Esophagectomy: A Curative Operation for Esophageal Cancer |
|
|
b |
Medium cervical |
|
ganglion |
|
R subclavian artery |
|
Ansa subclavia |
Inf. cervical ganglion 
Stellate ganglion |
1st thoracic |
|
ganglion |
 Esophageal br. of recurrent laryngeal n.
Esophageal br. of recurrent laryngeal n.
Fig. 5.32 (continued)
Inf. thyroid a.
 Thyroid gland
Thyroid gland
R vagus n.
 Common carotid a.
Common carotid a.
 Inf. cardiac n.
Inf. cardiac n.
Communicating branch
R recurrent n.
5.2 Part II: Thoracic Manipulation |
167 |
|
|
Pulmonary br. of R vagus n.
R inf. pulmonary v.
Esophagus
No.107 + 109-R LN
Tracheal cartilage
Fig. 5.33 The operative field is diverted to the middle mediastinum to dissect the lymph nodes around the tracheal bifurcation (No. 107) and under the right and left principal bronchi (No. 109). The first assistant retracts the right lung ventrally to apply a “small twist” to the middle
mediastinum so that the posterior aspect of the hilum of the right lung can be viewed from the anterior. Starting around the stump of the azygos arch, the mediastinal pleura is divided along the right principal bronchus
168 |
5 Ivor Lewis Esophagectomy: A Curative Operation for Esophageal Cancer |
|
|
R inf. pulmonary v.
Pericardium
No.107 + 109-R LN
Fig. 5.34 After identifying the pulmonary branch of the right vagus nerve and the preserved right bronchial artery over the surface of the membranous part (posterior wall) of trachea, the No. 109-R and No. 107 lymph nodes are detached from the bronchial wall, taking care to avoid damaging these branches as much as possible. The left bronchial artery migrates into the top of the No. 107
lymph nodes and should be ligated and divided when deemed necessary. Once the No. 107 lymph nodes have been removed, the pericardium over the left atrium can be seen between the right and left bronchi at their bifurcation. The right vagus nerve should be dissected beyond the origin of its pulmonary branch
5.2 Part II: Thoracic Manipulation |
169 |
|
|
Stretched R bronchial a. |
No.109-L LN |
R vagus n.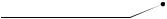 (cut)
(cut)
No.107 + 109-R LN
L bronchial a.
Fig. 5.35 The right lung is further retracted ventrally to apply a “major twist” to the middle mediastinum. The paraesophageal tissue is then grasped with a clamp to pull the esophagus dorsally (toward the surgeon). With this manipulation, the posterior aspect of the hilum of the left lung, in particular the membranous part of the left principal bronchus, finally makes its appearance. Being mindful of the left bronchial artery winding around the bronchial wall, the No. 109-L lymph nodes are removed. Dissection of the lymph nodes around the tracheal bifurcation and
those under the right and left bronchi should be started at the caudal portion of the No. 109-R lymph nodes, as described in the previous step, and advanced through the No. 107 up to the caudal portion of the No. 109-L lymph nodes, as if drawing a chevron shape. However, this causes substantial tension to the right bronchial artery, which runs across the front of the esophagus. If the tension of this artery precludes the development of an adequate operative field, we can perform No. 109-L lymph node dissection after esophageal transection (see Fig. 5.45)
170 |
5 Ivor Lewis Esophagectomy: A Curative Operation for Esophageal Cancer |
|
|
Thoracic duct
L mediastinal pleura
Fig. 5.36 After achieving increased mobility of the upper and middle esophagus, the operative field is reverted to the superior mediastinum to dissect lymph nodes around the left recurrent laryngeal nerve (No. 106-recL). Before doing so, the posterior side of the upper esophagus should be additionally dissected. The pleural detachment from the anterior aspect of the vertebrae was completed in the step described in Fig. 5.31, and now the detachment is further advanced to the left mediastinal pleura. Apart from avoiding rupture of the pleura, we should pay attention to the course of the thoracic duct in this area. After ascend-
ing parallel to the azygos vein over the anterior aspect of the vertebrae, the thoracic duct merges to the left at the level of the fifth thoracic vertebra and travels behind the aortic arch and across the left border of the esophagus. Therefore, the thoracic duct approaches closest to the esophagus in this area. In cases of middle to lower esophageal cancer eligible for intrathoracic anastomosis, it is very unlikely that dissection of this area will be limited by direct tumor invasion into the thoracic duct, so as much as possible of the duct should be preserved
5.2 Part II: Thoracic Manipulation |
171 |
|
|
Brachiocephalic a.
R brachiocephalic v.
L brachiocephalic v (innominate v.).
R vagus n.
L common carotid a.
No.106-recL LN
L subclavian a.
Thoracic duct
L recurrent n.
L mediastinal pleura
Fig. 5.37 Now the upper esophagus is connected to the left border of the trachea just via the connective tissue containing the left recurrent laryngeal nerve and its associated lymph nodes. The operative field is prepared to the left of the trachea by pulling the trachea up with a retracting spatula and pulling the esophagus dorsally toward the surgeon. The left recurrent laryngeal nerve, which ascends
within the connective tissue between the trachea and esophagus, is identified by careful exploration, isolated with a clamp (the clamp should be applied along the esophageal wall to avoid damaging the nerve), and taped with a cotton tape, while ensuring that the preserved thoracic duct is not taped
172 |
5 Ivor Lewis Esophagectomy: A Curative Operation for Esophageal Cancer |
|
|
Trachea
L recurrent n. Br. of L recurrent laryngeal n. to trachea
 No.108
No.108
Esophageal br. of L recurrent laryngeal n.
No.106-recL LN
R vagus n.
R bronchial a.
Fig. 5.38 The esophagus is pulled more firmly dorsally with the cotton tape to secure an adequate operative field to the left of the trachea for dissection of the No. 106-recL nodes along the left recurrent laryngeal nerve. This should also be done carefully so as not to pull apart the right bronchial artery traveling across the front of the esophagus. The recurrent laryngeal nerve, after having been liberated to some extent, is taped with a vessel tape and pulled gently to easily detach the lymph nodes. As far as possible, avoid the use of electrocautery because the fatty connective tissue around the nerve contains small
branches of the recurrent laryngeal nerve leading to the esophagus. Left recurrent laryngeal nerve palsy is far more frequent than right recurrent laryngeal nerve palsy and causes breathing difficulty, hoarseness, and postoperative aspiration and associated pneumonia. The surgeon should therefore take time to perform the procedure carefully. Where there is uncertainty about identification of the recurrent laryngeal nerve, the dissection should not be advanced blindly; rather, efforts should be made to identify the nerve that winds around the aortic arch in a recurrent fashion (see Fig. 3.42)
5.2 Part II: Thoracic Manipulation |
173 |
|
|
L recurrent n.
Fig. 5.39 Transection of the esophagus: After completing dissection of the No. 106-recL lymph nodes, the transection line of the esophagus is determined, taking into account the location of the lesion and the length of the gastric conduit prepared earlier. The line is usually set around the midpoint of the trachea. A purse-string instrument is applied on the oral side of the transection line, and
a 2-0 nylon suture with straight needles at both ends is passed. The resection side of the esophagus is tied with No. 1 silk suture, and the esophagus is transected along the instrument with Cooper scissors. The cut end of the suture tying the resection side should be kept long enough to be pulled
174 |
5 Ivor Lewis Esophagectomy: A Curative Operation for Esophageal Cancer |
|
|
Fig. 5.40 The |
Anvil |
purse-string instrument |
|
is removed, and the |
|
esophageal stump is |
|
grasped with three pairs |
|
of intestinal grasping |
|
forceps. Three to four |
|
additional interrupted |
|
3-0 silk sutures are |
|
placed slightly to the |
|
outer side of the existing |
|
suture for reinforcement. |
|
With the esophageal |
|
opening expanded to a |
|
triangle shape, the anvil |
|
of a 25-mm circular |
|
stapler is inserted and |
|
the purse-string suture is |
|
tied |
|
5.2 Part II: Thoracic Manipulation |
175 |
|
|
L recurrent n. |
Resection side of |
|
esophageal stump |
L subclavian a. |
|
R recurrent n. 
 No.105 LN
No.105 LN
No.108 LN
Thoracic duct
Arch of aorta
Fig. 5.41 With the esophagus lifted up with the suture tying the resection-side stump, the fatty connective tissue containing the No. 105 lymph nodes are detached from the anterior aspect of the aorta
176 |
5 Ivor Lewis Esophagectomy: A Curative Operation for Esophageal Cancer |
|
|
No.106tbL LN
Lig. arteriosum
L recurrent n.
R bronchial a.
L bronchial a.
L vagus n.
Arch of aorta
L pulmonary a.
Fig. 5.42 Once the dissection of the posterior side of the esophagus has advanced beyond the level of the azygos arch, the esophageal stump on the resection side is passed under the right bronchial artery and drawn out to the caudal side of the artery. This expands the leaf-shaped area bordered by the left principal bronchus and the aortic arch, providing a better view of the operative field. While identifying the left recurrent laryngeal nerve as it turns around while winding around the aortic arch, the fatty
connective tissue containing the No. 106-tbL lymph nodes is carefully resected. This should be done cautiously as several left bronchial arteries arising directly from the aortic arch are embedded in this fatty connective tissue. These arteries should be preserved, especially when the right bronchial artery has already been dissected or injured. Encountering the left pulmonary artery and the ligamentum arteriosum indicates the completion of No. 106-tbL lymph node dissection

5.2 Part II: Thoracic Manipulation |
177 |
|
|
a
R inf. pulmonary v.
Pulmonary lig.
Central tendon
* *
Pericardium
R phrenic n.
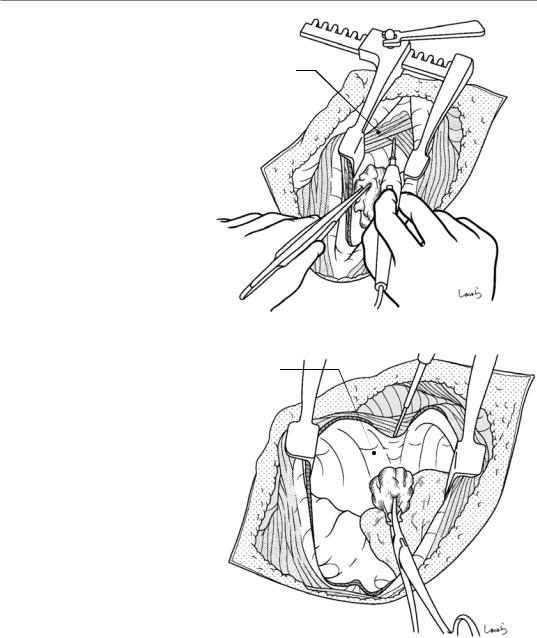
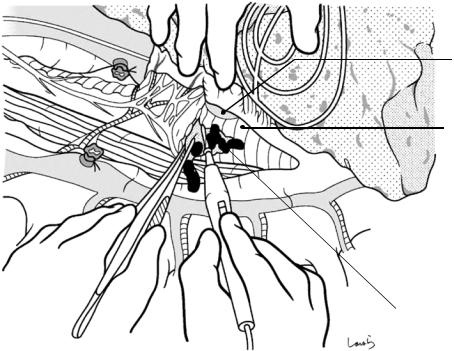
b
IVC
Fig. 5.43 We return now to dissection of the middle mediastinum. The first assistant retracts the inferior lobe of the right lung cranially. Caudal to the right bronchus is the right inferior pulmonary vein, whose lower border is anchored to the diaphragm via a fold-like membrane referred to as the pulmonary ligament, which also corresponds to the transition from the parietal pleura to the visceral pleura. This ligament should be dissected if the inferior lobe obscures the view of the operative field in the
Mediastinal pleura separated in the preceding dissection rom abdominal cavity
middle and inferior mediastinum (a). This ligament may contain branches of the proper esophageal artery and/or direct branches of the descending aorta (asterisk in (a)), which should be ligated and divided once identified
The inferior mediastinal pleura is divided. This pleura is already separated from the esophagus by the preceding dissection procedure from the abdominal cavity and is identified as a membrane through which a dark red structure can be seen deep within (b)
178 |
5 Ivor Lewis Esophagectomy: A Curative Operation for Esophageal Cancer |
|
|
Pericardium
Proper esophageal a.
No.108
R bronchial a.
L bronchial a.
Proper esophageal a.
Pulmonary br. of L vagus n.
Descending thoracic aorta
Fig. 5.44 Pulling the esophageal stump on the resection side caudally, the fatty connective tissue containing the middle paraesophageal lymph nodes (No. 108) is detached from the aorta and the pericardium. The left vagus nerve is
then dissected distal to the origin of its pulmonary branch. Two to three proper esophageal arteries branching from the descending aorta, identified as solid cords, are ligated and divided when encountered
5.2 Part II: Thoracic Manipulation |
179 |
|
|
|
L atrium |
|
R inf. pulmonary v. |
No.109L |
No.108 LN |
|
No.110 LN
L bronchial a. |
R mediastinal pleura |
L mediastinal pleura
No.112ao LN
L vagus n.
L inf. pulmonary v.
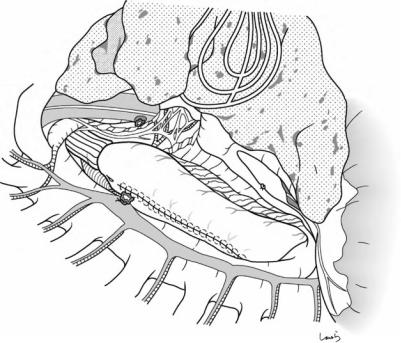
Fig. 5.45 As the dissection is further advanced between the pericardium and the aorta and as the thoracic para- aortic lymph nodes (No. 112-ao) are dissected, the left lung is seen through the left mediastinal pleura posteriorly. Any residual No. 109-L lymph nodes attached to the left bronchus should be dissected. As the pericardium is further firmly retracted ventrally and the aorta is retracted dorsally, the posterior aspect of the left inferior pulmonary vein is exposed. The dissection should be advanced
up to the vicinity of the vein. This is the actual scene where we “view the back side of the left mediastinum through right thoracotomy”
At this point, the dissection connects with the dissection of the No. 110 lymph nodes from the abdominal cavity and the detachment of the esophagus is completed. Any residual lymph nodes in the inferior mediastinum should be dissected
180
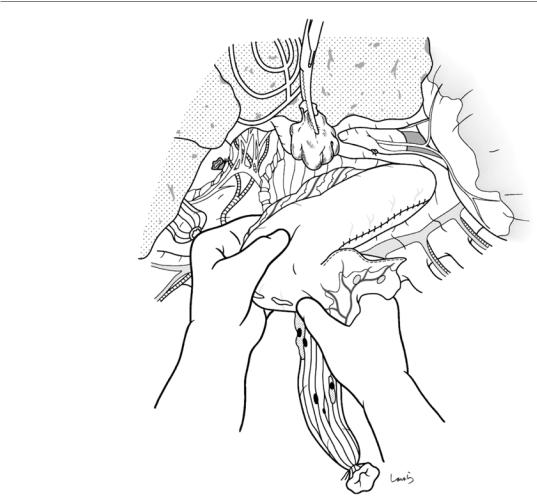
Fig. 5.46 The gastric conduit is slowly drawn into the thoracic cavity ensuring that there is no torsion; the lesser curvature side is the upper side and the greater curvature side is the lower side of the conduit. To avoid damaging the greater omentum, the greater curvature side should be firmly grasped while pulling the conduit, as shown
5 Ivor Lewis Esophagectomy: A Curative Operation for Esophageal Cancer
e |
|
|
curvatur |
e |
|
Greater |
curvatur |
|
Lesser |
||
|
5.2 Part II: Thoracic Manipulation |
181 |
|
|
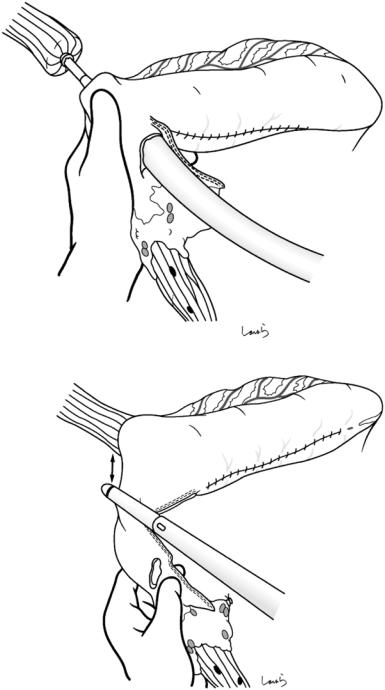
Fig. 5.47 A small incision is made on the anterior gastric wall directly below the esophagogastric junction, and a circular stapler is inserted through the incision. The center rod is advanced through the planned anastomosis site on the greater curvature side and firmly inserted into the anvil shaft placed in the esophageal stump
Fig. 5.48 The cardiac portion of the stomach, which includes the opening for inserting the circular stapler, is transected 3 cm away from the anastomosis with a linear stapler and the resected specimen is removed. Additional interrupted seromuscular 3-0 Vicryl sutures are applied to invaginate the staple line
EG junction 
3 cm
Opening for circular stapler 
182 |
5 Ivor Lewis Esophagectomy: A Curative Operation for Esophageal Cancer |
|
|
Fig. 5.49 A nasogastric tube is introduced up to the midpoint of the gastric conduit, then the conduit is pulled back to the abdominal cavity to the extent that there is no slack in the conduit, but no tension applied to the anastomosis. Failure to perform this procedure can cause retention of food in the thoracic gastric conduit and delayed passage through the esophageal hiatus
5.2 Part II: Thoracic Manipulation |
183 |
|
|
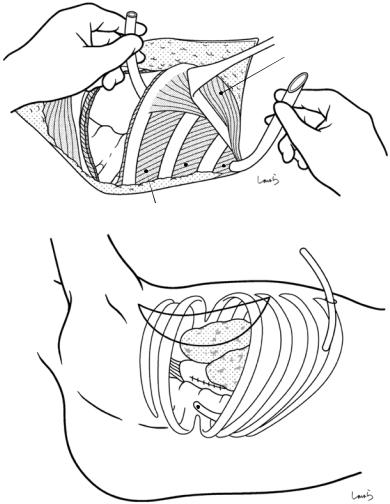
Fig. 5.50 After |
a |
washing the thoracic |
|
cavity, a thoracic drain is |
|
placed. With the serratus |
|
anterior retracted |
|
caudally, the thoracic |
|
drain is inserted through |
|
the 7th (or 6th) |
|
intercostal space (a). A |
|
skin incision is then |
|
made at a point slightly |
|
ventral from the drain |
|
insertion point in the |
|
same intercostal space, |
|
and the drain is tunneled |
|
under the serratus |
|
anterior and pulled out |
b |
of the body through the |
|
incision (b). Because the |
|
lowest point of the |
|
thoracic cavity is around |
|
the fifth intercostal space |
|
in the supine position, |
|
the tip of the drain |
|
should be placed at the |
|
level of the fourth |
|
intercostal space |
|
Serratus anterior
V VI VII
5 |
6 |
7 |
|
||
|
|
Tip of the drain
184 |
5 Ivor Lewis Esophagectomy: A Curative Operation for Esophageal Cancer |
|
|
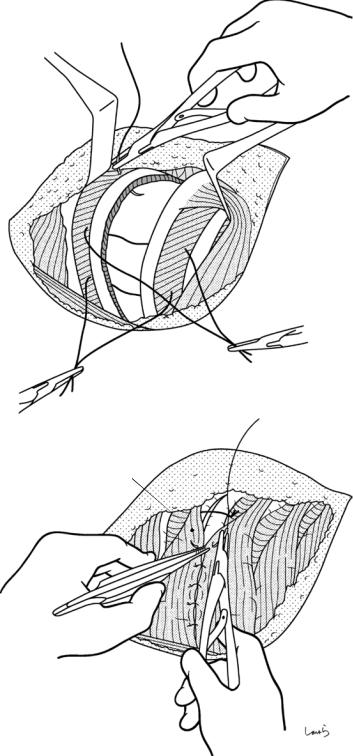
Fig. 5.51 Three Vicryl 1 sutures are passed through the upper and lower sides of the fourth intercostal space through which the thoracotomy was performed (a). After confirming that there is no damage to the intercostal arteries, the pillow placed under the patient can be removed and the sutures tied to bring the two ribs together. The divided serratus anterior is re-sutured (b)
a
IV
V
b |
Serratus anterior |
5.2 Part II: Thoracic Manipulation |
185 |
|
|
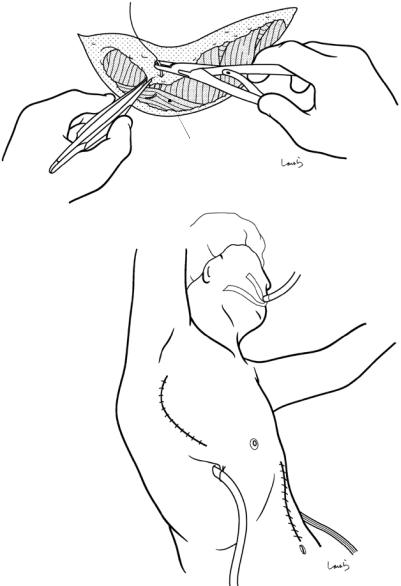
Fig. 5.52 The edge of |
a |
the latissimus dorsi and |
|
the subcutaneous tissue |
|
at the same depth are |
|
brought together by |
|
several interrupted |
|
sutures (a). The |
|
operation is completed |
|
by placing subcutaneous |
|
and skin sutures (b) |
|
b
Latissimus dorsi
Thoracic drain
Drain placed in L subphrenic space
