
- •Foreword
- •Preface
- •Contents
- •1.1 Introduction
- •1.2 Prologue
- •1.9 Expansion of the Greater Omentum
- •3: Distal Gastrectomy
- •4: Total Gastrectomy
- •5.2 Part II: Thoracic Manipulation
- •6: Right Hemicolectomy
- •7: Appendectomy
- •8.6 Internal Pudendal Artery and Its Branches
- •8.13 Lateral Ligament
- •8.16 Fascia Propria of the Rectum: Part II
- •9: Sigmoidectomy
- •13: Hemorrhoidectomy
- •14: Right Hemihepatectomy
- •15: Left Lateral Sectionectomy
- •16: Laparoscopic Cholecystectomy
- •17: Open Cholecystectomy
- •Bibliography

Hemorrhoidectomy |
13 |
|
Abstract
Organ-specific expertise is being increasingly emphasized within the already narrow field of gastrointestinal surgery. This trend is becoming more apparent outside of university hospitals too. However, given the universality of the anatomy on which surgery is based, I feel it a huge waste to limit the surgeon’s skill to particular organs all in the name of specialty. As gastrointestinal surgeons, we should bear in mind that the continuity of membranes and the
major principles of total mesenteric resection are applicable to all organs as a whole.
Although simple, hemorrhoidectomy is a gastrointestinal surgical procedure that self- proclaimed specialists are encouraged to master. It takes only about 10 min to remove 1 hemorrhoid and just 30 min for 3 hemorrhoids.
Keywords
Hemorrhoidectomy · Surgical anatomy Organ-specific expertise
© Springer Nature Singapore Pte Ltd. 2020 |
319 |
H. Shinohara, Illustrated Abdominal Surgery, https://doi.org/10.1007/978-981-15-1796-9_13 |
|
320 |
13 Hemorrhoidectomy |
|
|
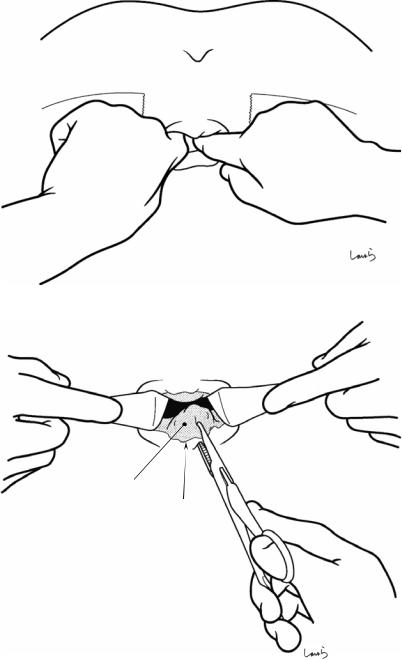
Fig. 13.1 Lumbar anesthesia is administered with the patient in the sitting position. After 3–5 min, the patient is repositioned to the jack-knife position, with the gluteal region exposed to the right and left and fixed with adhesive plasters. Because patients with hemorrhoids tend to have anal stenosis, it is advisable to insert the
index fingers of both hands into the anus to adequately relax the muscles of the anal sphincter before starting the operation
Fig. 13.2 Internal hemorrhoids commonly occur at the 3, 7, and 11 o’clock positions, although the pattern of onset varies considerably from patient to patient. First, two flat retractors are inserted into the anus to assess the overall morphology of the hemorrhoids and imagine the final picture. To prevent postoperative stenosis, up to 3 (at very most 4) mucosal resections should be made even for a nearly circumferentially developed hemorrhoid. The largest hemorrhoid should be resected first. The mucosa near the dentate line is grasped with Pean forceps
Internal hemorrhoid
Dentate line
13 Hemorrhoidectomy |
321 |
|
|
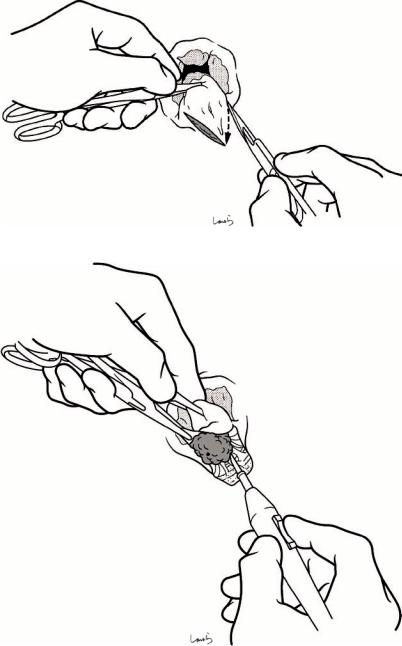
Fig. 13.3 With the hemorrhoid lifted up with the forceps, a V-shaped skin incision is made on the anal verge with a scalpel (arrow)
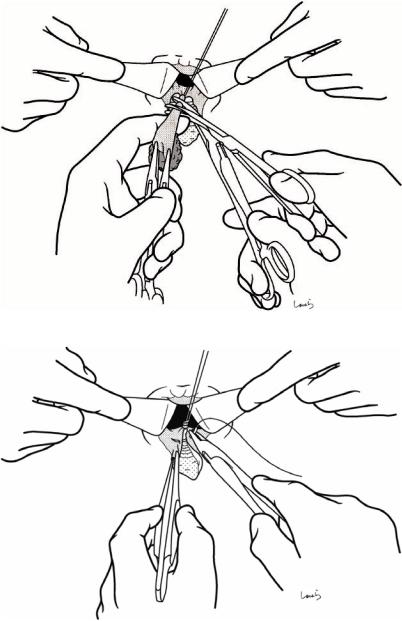
Fig. 13.4 The apex of the V-shaped incision is grasped with another pair of Pean forceps. The left index finger is placed on the medial side of the hemorrhoid, and then the two pairs of forceps are pulled slightly upward which serves to lift the darkened hemorrhoidal varix. The loose connective tissue between the varix and anal wall is dissected using an inactivated electrocautery device as a spatula, with care taken not to rupture the varix. At this point, the hemorrhoid can be lifted quite a lot. The remaining task is to dissect streaks of residual connective tissue with activated electrocautery. The circular muscle fibers of the internal anal sphincter can be seen on the anal wall side
 Int. anal sphincter
Int. anal sphincter
Internal hemorrhoid (varix)
322 |
13 Hemorrhoidectomy |
|
|
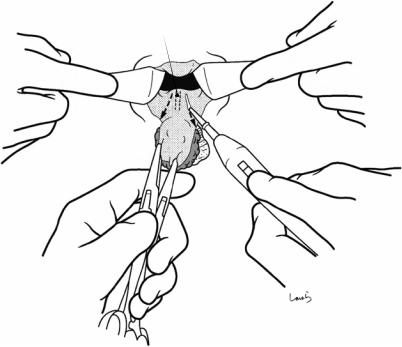
Hemorrhoidal a. (br. of superior rectal a.)
Fig. 13.5 After the dissection from the lateral side has proceeded to a considerable point, we can then move on to dissection of the connective tissue on both sides of the hemorrhoid. After pulling the hemorrhoid laterally and palpating the hemorrhoid artery (a branch of the superior rectal artery), a mucosal incision is made on both sides of
the hemorrhoid. To prevent postoperative anal stenosis, we should minimize the width of the mucosal incision. Remember that the goal of hemorrhoidectomy is to remove varices formed under the mucosa, and mucosal resection offers only a breakthrough toward achieving this goal
13 Hemorrhoidectomy |
323 |
|
|
Fig. 13.6 The submucosal layer is entered from the mucosal incision line to completely remove the hemorrhoidal varix by scraping it off. This is done in the same way as described in Fig. 13.4, by activating the electrocautery device or using it as a spatula
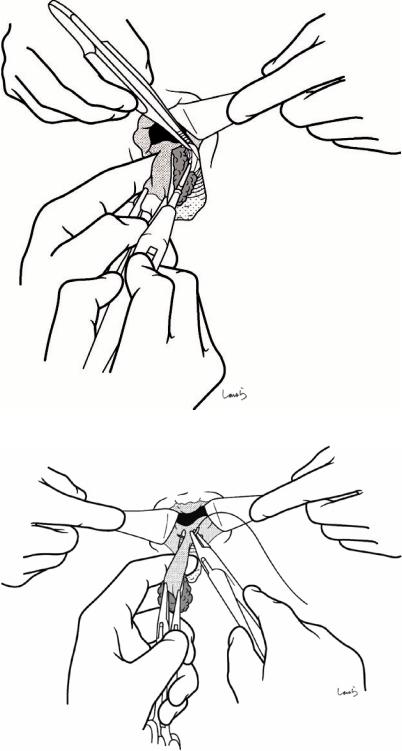
Fig. 13.7 Now that the hemorrhoidal varix has been completely detached from the internal anal sphincter and the bilateral submucosal layers, the only connective tissue remaining is a cord-like structure containing the hemorrhoidal artery. The cord-like structure is ligated by a piercing with a 3-0 Vicryl suture
 Int. anal sphincter
Int. anal sphincter
324 |
13 Hemorrhoidectomy |
|
|
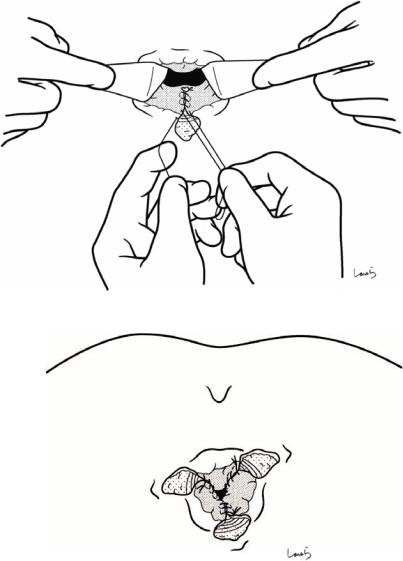
Fig. 13.8 After applying a clamp distal to the ligation and resecting the hemorrhoid, another 3-0 Vicryl suture is applied to make a double ligation. One of the two suture threads is left uncut so that we can use it as a stay suture for the next mucosal suture
Fig. 13.9 The mucosal defect formed by resection can either be left untreated as an open wound or suture-closed to achieve hemostasis at the mucosal stump and promote clean wound healing. A running 3-0 Vicryl suture is placed. The first ligation suture and stay suture are further tied to invaginate the stump
13 Hemorrhoidectomy |
325 |
|
|
Fig. 13.10 The mucosal suture should not exceed the dentate line. To prevent the formation of dead space, we should leave the skin incision unsutured as an open wound for drainage
Fig. 13.11 The procedure described above is performed for all hemorrhoids, typically 3. The operation is completed after confirming the absence of bleeding and the completeness of the mucosal sutures
