
- •Foreword
- •Preface
- •Contents
- •1.1 Introduction
- •1.2 Prologue
- •1.9 Expansion of the Greater Omentum
- •3: Distal Gastrectomy
- •4: Total Gastrectomy
- •5.2 Part II: Thoracic Manipulation
- •6: Right Hemicolectomy
- •7: Appendectomy
- •8.6 Internal Pudendal Artery and Its Branches
- •8.13 Lateral Ligament
- •8.16 Fascia Propria of the Rectum: Part II
- •9: Sigmoidectomy
- •13: Hemorrhoidectomy
- •14: Right Hemihepatectomy
- •15: Left Lateral Sectionectomy
- •16: Laparoscopic Cholecystectomy
- •17: Open Cholecystectomy
- •Bibliography

Left Lateral Sectionectomy |
15 |
|
Abstract
During fetal life, blood from the placenta flows through the umbilical vein and ductus venosus and drains into the inferior vena cava of the fetus. After birth, the umbilical vein is obliterated, except for a remnant that becomes the umbilical portal vein and is replaced by the round ligament of the liver, while the ductus venosus also closes and becomes the ligamentum venosum. In left lateral sectionectomy, the part of the liver to the left of these old
structures is cut off, and here the ligamentum venosum serves as a good landmark for determining the transection line. The duct of Arantius, which surgeons often use as a reference, is the obliterated ligamentum venosum and is occasionally mentioned in this chapter. The standard operation time is 2 h and 30 min.
Keywords
Umbilical vein · Ductus venosus · Left lateral sectionectomy · Duct of Arantius
© Springer Nature Singapore Pte Ltd. 2020 |
369 |
H. Shinohara, Illustrated Abdominal Surgery, https://doi.org/10.1007/978-981-15-1796-9_15 |
|
370 |
15 Left Lateral Sectionectomy |
|
|
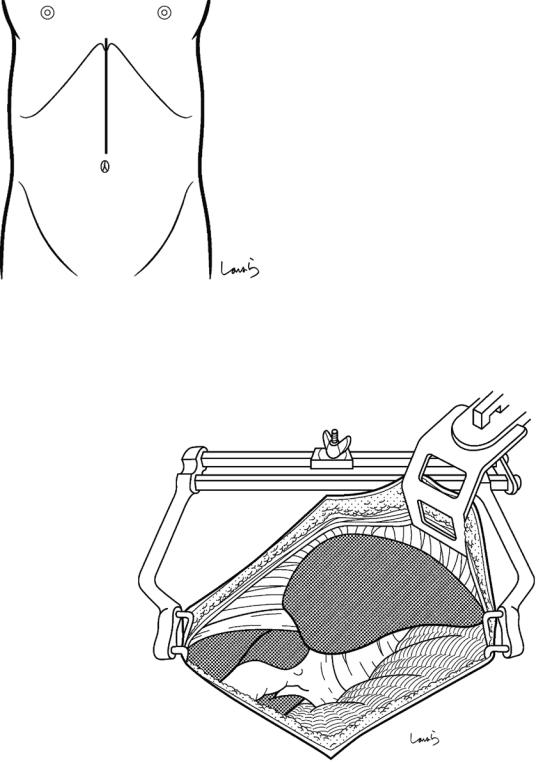
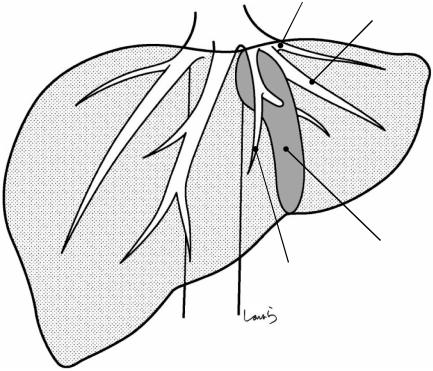
Fig. 15.1 The surgeon stands on the right side of the patient and makes an upper abdominal midline incision extending from the xiphoid process to the umbilicus to open the abdomen to the left of the round ligament of the liver
Fig. 15.2 A wound retractor and a left rib retractor are applied to secure the operative field. A surgical laparotomy sponge is placed over the stomach, spleen, and transverse colon
15 Left Lateral Sectionectomy |
371 |
|
|
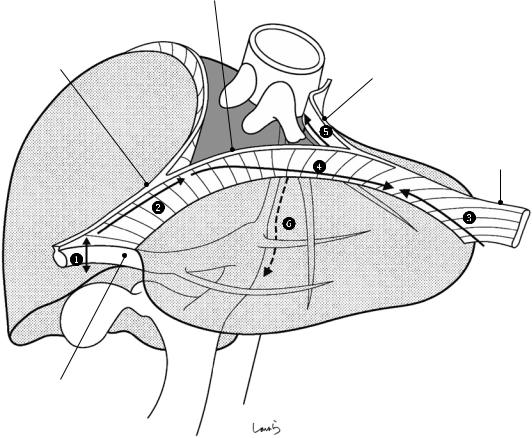
Ant. layer of L coronary lig.
|
IVC |
Falciform lig. |
Post. layer of L coronary lig. |
|
L triangular lig.
Ligamentum teres
Fig. 15.3 The procedure begins with mobilization of the lateral segment and is performed in the following order: dividing the round ligament, dividing the falciform ligament, dividing the left triangular liga-
ment, dividing the anterior layer of the left coronary ligament, dividing the posterior layer of the left coronary ligament, and dividing the attachment of the lesser omentum to the liver
372 |
15 Left Lateral Sectionectomy |
|
|
Falciform lig.
Ligamentum teres
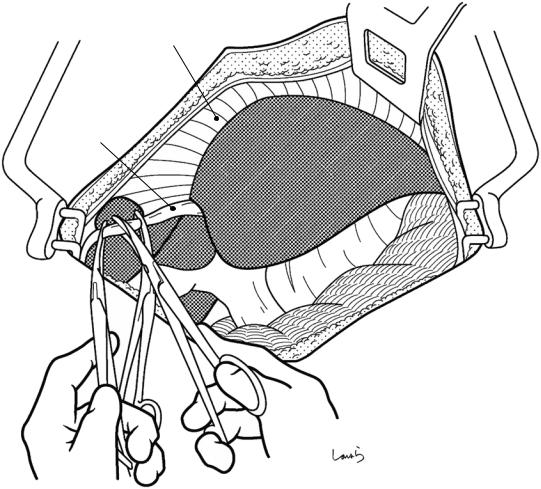
Fig. 15.4 The round ligament is ligated and divided at a point closer to the abdominal wall side. The suture thread on the liver side is kept long enough to allow for later traction and is grasped with Pean forceps
15 Left Lateral Sectionectomy |
373 |
|
|
L coronary lig.
Falciform lig.
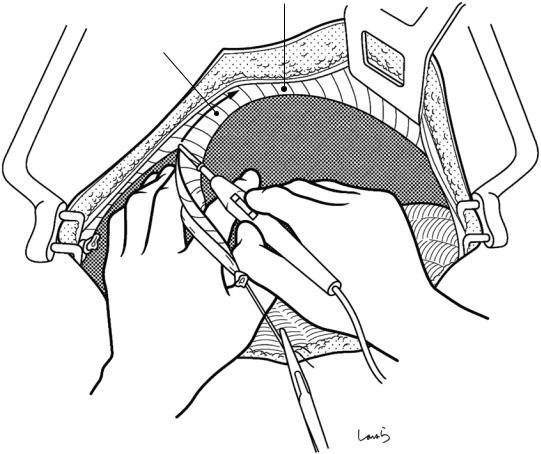
Fig. 15.5 The falciform ligament is divided along its attachment to the diaphragm with electrocautery. The falciform ligament is kept attached to the liver so that it can be used as a “lid” to cover the dissection plane of the liver
afterward. The dissection proceeds up to the point where the ligament divides into a V-shape to become the right and left coronary ligaments
374 |
15 Left Lateral Sectionectomy |
|
|
L coronary lig.
L triangular lig.
Fig. 15.6 With the lateral segment pulled caudally, the left triangular ligament is divided with electrocautery. Because the triangular ligament is formed by fusion of the anterior and posterior layers of the coronary ligament,
dividing this ligament about 3 cm medially from the tip of the lateral segment causes the coronary ligament to split into the anterior and posterior layers, forming an opening
15 Left Lateral Sectionectomy |
375 |
|
|
Fig. 15.7 The anterior layer of the left coronary ligament is divided with electrocautery while being scooped with dissection forceps. Our dissection line should approach
L triangular lig. (divided)
the liver parenchyma gradually to avoid damaging the phrenic vessels
376 15 Left Lateral Sectionectomy
Mid. hepatic v. |
L hepatic v. |
|
|
||
|
|
|
R coronary lig. |
|
|
|
|
|
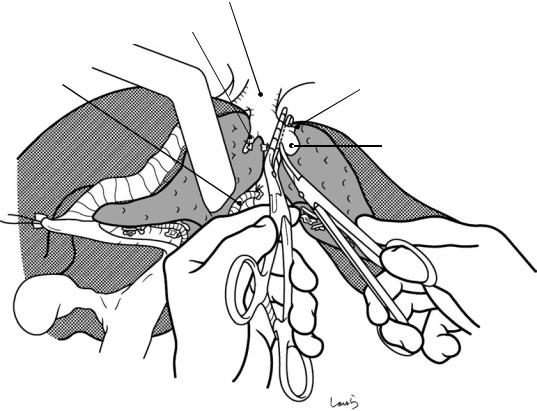
Fig. 15.8 The connective tissue surrounding the left and middle hepatic veins are roughly dissected with Metzenbaum scissors. These two veins often form a com-
mon trunk at their root. Cutting the right coronary ligament slightly may make it easier to identify the hepatic veins
15 Left Lateral Sectionectomy |
377 |
|
|
*L sup. hepatic v. |
Post. layer of |
|
L coronary lig. |
L hepatic v. |
|
Fig. 15.9 The posterior layer of the left coronary ligament is divided with electrocautery (arrow). During this procedure, the left hepatic vein or a superficial vein (the left superior hepatic vein, asterisk) appears as it courses rather transversely as shown, and we need to be careful not to
damage it by moving the electrocautery device too much. It is safer to switch from electrocautery to Metzenbaum scissors when the dissection approaches the root of the left hepatic vein. The left superior hepatic vein may independently converge with the inferior vena cava (IVC)
378 |
15 Left Lateral Sectionectomy |
|
|
L hepatic v.
Lesser omentum
Fig. 15.10 After the lateral segment is everted to the right, right-angled dissection forceps are inserted downward from the cut edge of the posterior layer of the coronary ligament (arrow) to scoop up the peritoneum and divide it with electrocautery. This peritoneum covers the
right crus of the diaphragm, which forms the esophageal hiatus, and continues as the lesser omentum. Repeating this procedure twice or more allows the tip of the forceps to reach the omental bursa
15 Left Lateral Sectionectomy |
379 |
||
|
|
|
|
|
|
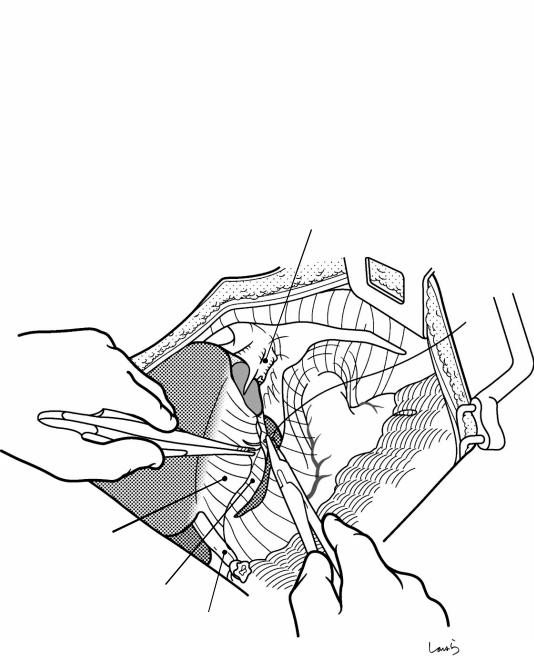
R crus |
|
Lobule of Spiegel within |
IVC |
||
caudate lobe |
|||
Duct of Arantius |
|
||
|
|||
|
|
||
|
|
|
|
Ligamentum teres
Transverse portion of
L portal v.
Fig. 15.11 After opening the omental bursa, the lobule of Spiegel within the caudate lobe makes its appearance. In the groove between this part and the lateral segment is the duct of Arantius, which used to be a major blood vessel during fetal life that connected the umbilical portal vein and the IVC but is now a cord that is attached to the lesser omentum. It is rather surprising that the attachment of the
lesser omentum to the liver, which is not much considered during gastrectomy, lies longitudinally (not horizontally) like this. As shown, the lesser omentum is divided along the duct of Arantius up to the vicinity of the hepatoduodenal ligament (arrow). If the left accessory hepatic artery arising from the left gastric artery is encountered, ligate and divide it
380 |
15 Left Lateral Sectionectomy |
|
|
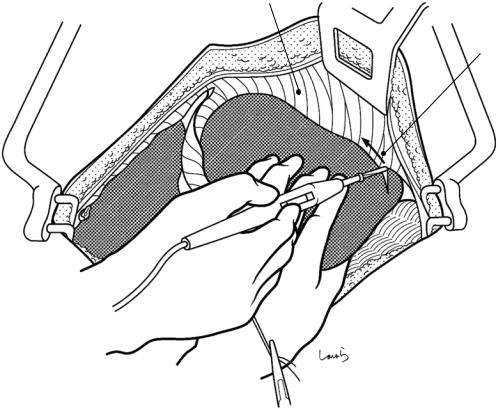
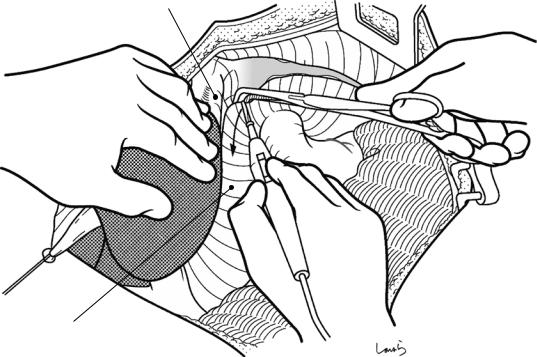
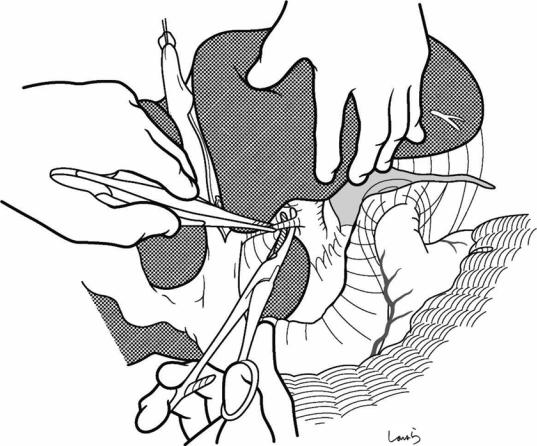
Fig. 15.12 We move on now to dissection of the Glissonean vessels. The suture thread applied to the round ligament is pulled cranially but slightly to the right to cause the lateral segment to stand upright. If the liver parenchyma forms a bridge overlying the umbilical portal vein, scoop the bridge with dissection forceps at once and divide with electrocautery
a |
b |
Wrong shape |
Correct shape |
Fig. 15.13 The lateral segment of the liver is generally thought to have a pyramidal shape (a), but it is actually flat- shaped (b), with its longitudinal cross section not triangular-shaped but rather spindleor comma-shaped
15 Left Lateral Sectionectomy |
381 |
|
|
a
b
|
8 |
|
7 |
8 |
|
|
2 |
|
|
4b |
|
|
|
3
7
6
4a
6
5
5
c
d
5 4a
5
3
6
8 4b
2
6
8
7
7
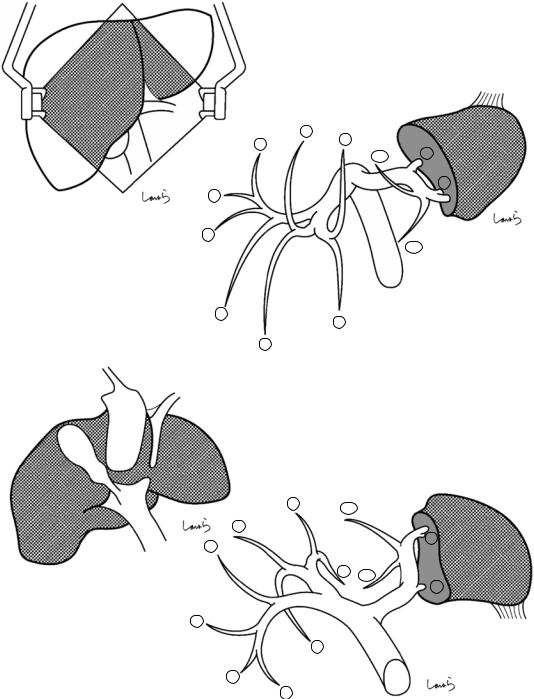
Fig. 15.14 When the liver is in its natural position as seen on abdominal opening (a), the cranial part is S2 and the caudal part is S3 (b). But when the round ligament is pulled up and the lateral segment rises upward (c), then
the upper part is S3 and the lower part is S2 (d). This follows the same logic as the liver becoming upside down when repositioned for portal manipulation during right lobectomy (see Fig. 14.20)
382 |
15 Left Lateral Sectionectomy |
|
|
Ligamentum teres
Cut edge of lesser omentum
Lobule of Spiegel within caudate lobe
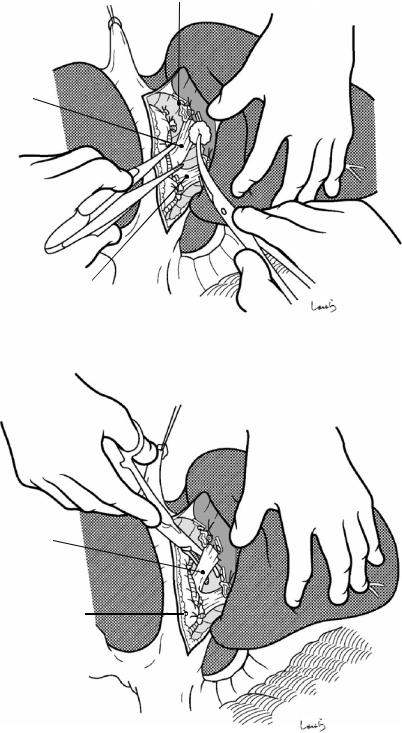
Fig. 15.15 In front of the umbilical portal vein, right- angled dissection forceps are inserted upward from the preformed cut edge of the lesser omentum to scoop just
the peritoneum (arrow) and divide it with electrocautery. The dissection line should ascend along the left margin of the round ligament
15 Left Lateral Sectionectomy |
383 |
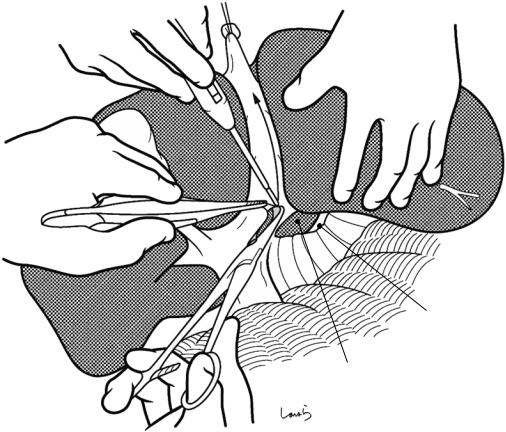
|
|
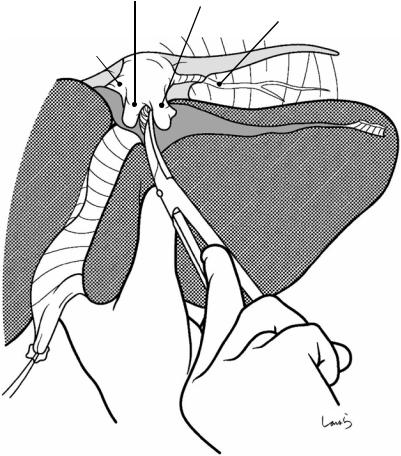
Fig. 15.16 Opening the round ligament exposes fat and loose connective tissue, in which the portal vein, artery, and bile duct are embedded. As the connective tissue is peeled off laterally with a gauze ball, many small branches
leading to the left lateral segment are exposed. The forceps are switched to Metzenbaum scissors and the connective tissue is dissected carefully to roughly expose the branches
384 |
15 Left Lateral Sectionectomy |
|
|
P4a
A4a from mid. hepatic a.
A4b from L hepatic a.
Mid. hepatic a.
Common hepatic duct
P3 A3
UP |
Small br. entering from UP to lat. |
|
segment |
||
|
TP
P2 A2
L hepatic a.
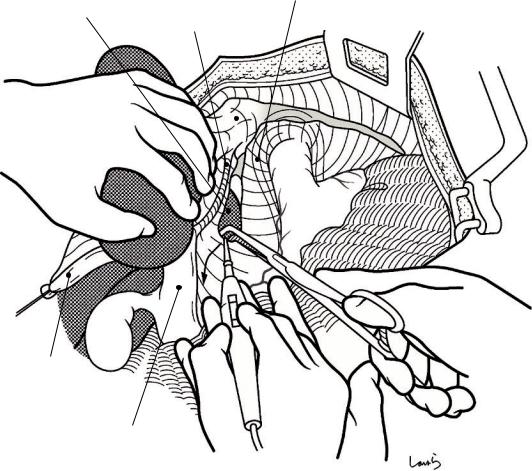
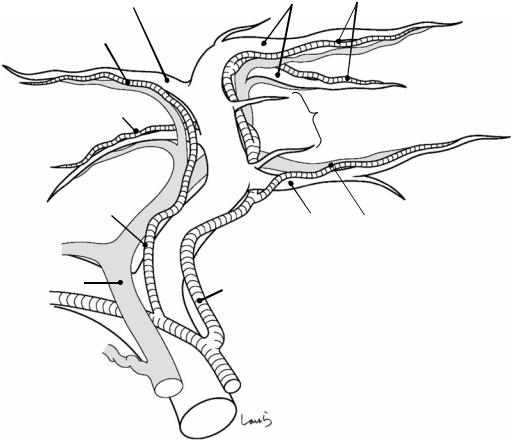
Fig. 15.17 When looking at these branches more closely, the transverse portal vein (TP) gives off the P2 branch from the lateral side of the corner of the curve before it becomes the umbilical part (UP) and the main P3 branch arises from the end of the UP. There is usually one P2 branch and often two P3 branches. Between P2 and P3 are several small branches about 1 mm in diameter, in addition to the main branch. It might be surprising to see so many branches because they are rarely visualized by extracorporeal ultrasonography
Although there are many variations to the course of the left hepatic artery, it commonly travels to the upper left
while crossing in front of the UP and gives off the A2 branch. From there, the A3 branch dives under (or crosses) the P2, ascends along the left border of the UP, and enters the liver parenchyma along with the main P3 branch. The middle hepatic artery supplying S4 can either arise as an independent branch outside the liver or arise from the left hepatic artery while ascending along the left border of the UP and passing behind the UP before entering S4, or it can be a mixture of the two patterns as shown. So, dissecting the left hepatic artery in front of the UP may result in sacrificing A4. The bile duct is at the deepest level and cannot be identified on opening the round ligament
15 Left Lateral Sectionectomy |
385 |
|
|
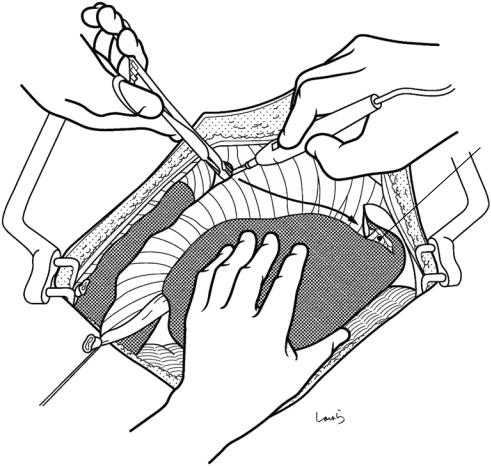
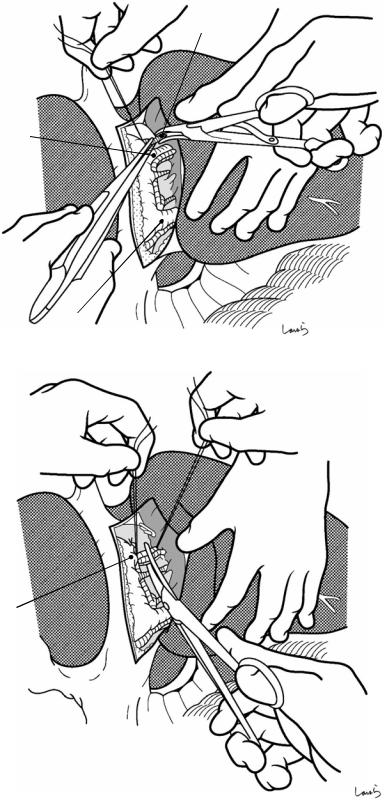
Fig. 15.18 Portal branches are then dissected. In the order of encounter during dissection from the surface, branches are sequentially scooped up with right-angled forceps, ligated on the proximal side, clipped on the resection side, and divided with Metzenbaum scissors
Fig. 15.19 The main branches are ligated on both the proximal and resection sides with a 3-0 Vicryl suture and then divided. Accompanying arterial branches are also ligated and divided together with veins. To avoid damaging small portal branches that may be present behind the main branches, adequately expose these main branches with dissectors or other instruments before scooping with forceps. Because the A4 branch, which must be preserved, may arise from the artery ascending along the left border of the UP
(Fig. 15.17), dissect the branch only after confirming its distribution to the lateral segment
Main P3 br.
Main P2 br.
P3 + A3
Small portal br.
386 |
15 Left Lateral Sectionectomy |
|
|
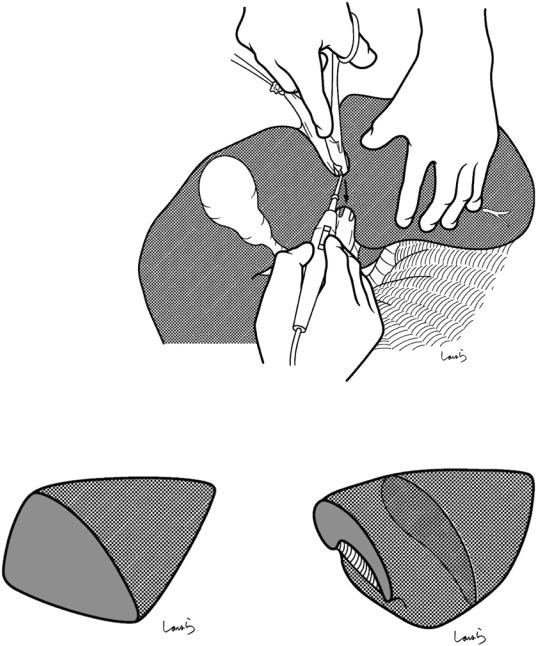
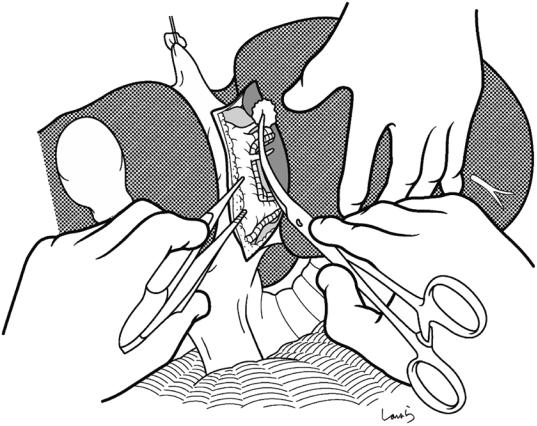
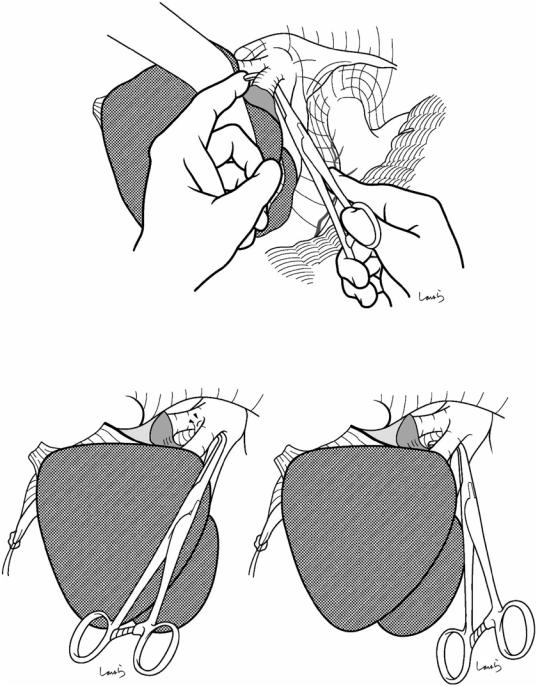
Fig. 15.20 The bile duct has a fibrous pattern/structure and cannot be identified easily. The connective tissue is peeled off laterally with a gauze ball to expose the bifurcation of the B3 and B2 (a). Then, dissection forceps are inserted along the liver parenchyma to scoop up each duct close to the bifurcation and then ligate/divide them (b). The ducts can be ligated en bloc before the bifurcation if the resulting ligated bundle is not too thick
a |
P3 +A3 |
|
(ligated on proximal side) |
||
|
B3
B2
b
B3
P2 + A2
(ligated on resection side)
15 Left Lateral Sectionectomy |
387 |
|
|
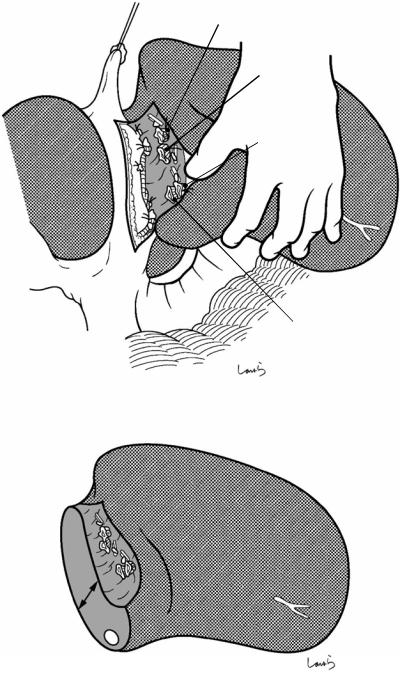
Fig. 15.21 Once the Glissonean vessels are dissected, the lateral segment is quite mobile (a). The remaining liver parenchyma is thinner than often expected, which again makes us appreciate the flat shape of the lateral segment. The parenchyma is only about 1.5 cm thick in a resected specimen (b)
a |
P3 + A3 (ligated) |
|
|
|
B3 (ligated) |
P2 + A2 (ligated)
B2 (ligated)
b
1.5 cm
L hepatic v. 
388 |
15 Left Lateral Sectionectomy |
|
|
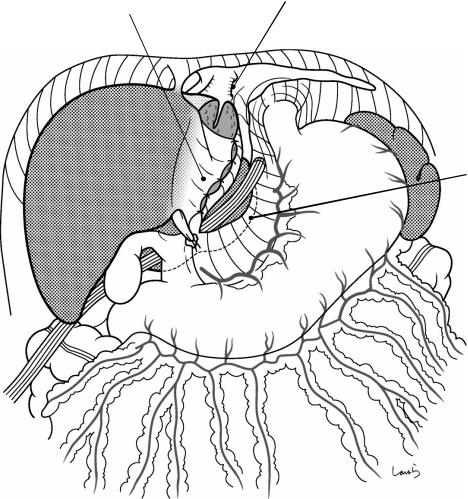
L hepatic v.
Fig. 15.22 Dissection of the left hepatic vein: With the lateral segment everted to the right, the connective tissue around the lateroposterior aspect of the left hepatic vein is roughly excised with dissectors
15 Left Lateral Sectionectomy |
389 |
|
|
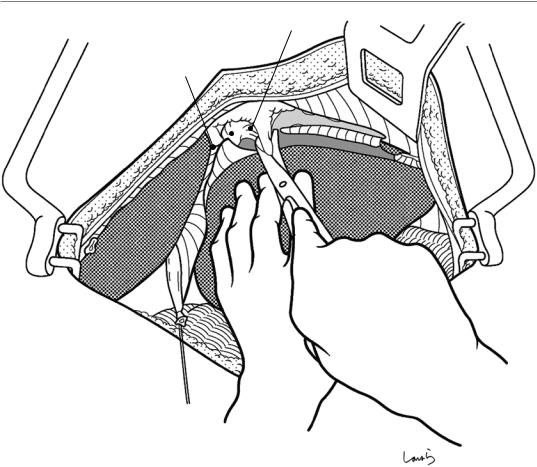
Fig. 15.23 Then, the lateral segment is retracted cranially to the extent that it attaches tightly to the diaphragm. After dissecting the connective tissue around the medio-
posterior aspect of the left hepatic vein, the convergence of the duct of Arantius can be identified
390 |
15 Left Lateral Sectionectomy |
|
|
Fig. 15.24 The duct of Arantius is ligated and divided close to the root of the left hepatic vein. Although dissecting this duct is not essential in left lateral sectionectomy,
it helps achieve a relatively long margin at the root of the left hepatic vein
15 Left Lateral Sectionectomy |
391 |
|
|
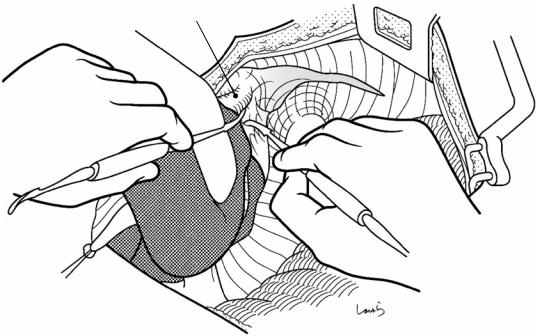
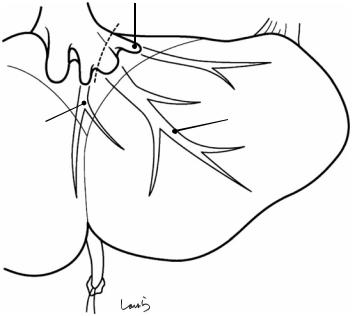
Fig. 15.25 After being repositioned to the original natural position, the lateral segment is grasped with the left hand and pulled caudally. To expose the medial border of the left hepatic vein, the connective tissue is scraped off with Metzenbaum scissors so that the concavity at the bifurcation of the left and middle hepatic veins can be identified
Mid. hepatic v. L hepatic v.
L inf. phrenic v.
R hepatic v.
392 |
15 Left Lateral Sectionectomy |
|
|
a
b |
c |
Unsafe |
Safe |
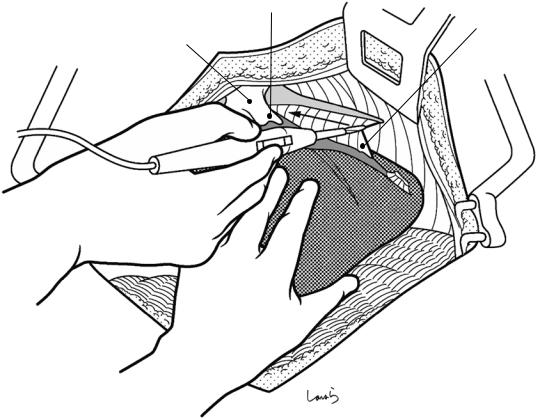
Fig. 15.26 A right-angled forceps is carefully passed under the left hepatic vein to scoop the vein, with a fingertip applied to the concave surface of the bifurcation to direct the tip of the forceps to the correct exit (a). Do not push the forceps if any resistance is felt, but instead retract the forceps and dissect the connective tissue
again—advancing the forceps with the tip facing upward might rupture the bifurcation (b). So, be sure to advance the forceps along the liver parenchyma (c). After encircling the left hepatic vein, a vascular tape is passed around the vein and grasped with mosquito forceps
15 Left Lateral Sectionectomy |
393 |
|
|
L sup. hepatic v.
Main br. of L hepatic v.
Umbilical fissure v.
Fig. 15.27 The root of the main trunk of the left hepatic vein is quite wide when it receives the left superior hepatic vein, adjunctive veins such as the umbilical fissure vein (left middle hepatic vein) that ascends along the UP while receiving venous return from S3 and S4, and the duct of Arantius, which was previously dissected. An imaginary
dissection line is set distal to the convergence of the umbilical fissure vein but including the main trunk and the left superior hepatic vein (dotted line). If it is difficult to accurately encircle the veins, do the parenchymal dissection first and then ligate the hepatic veins
394 |
15 Left Lateral Sectionectomy |
|
|
L sup. hepatic v.
L hepatic v.
 Br. from S3
Br. from S3
Dissection plane of liver
Umbilical fissure v.
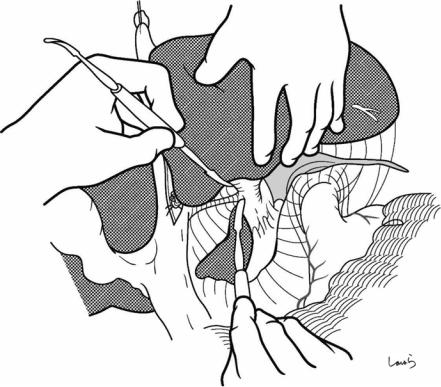
Fig. 15.28 At this point, the lateral segment is discolored dark red, bordered by the falciform ligament. Parenchymal dissection is performed along the imaginary dissection line set 1 cm to the left of the ligament. The procedure is the same as that for right lobectomy. A relatively thick
branch extending from S3 and draining into the umbilical fissure vein may be encountered around the upper border and should be ligated and divided. The dissection area is small, so the dissection can be completed very quickly
15 Left Lateral Sectionectomy |
395 |
|
|
Mid. hepatic v. |
|
Umbilical fissure v. |
|
Duct of Arantius |
|
(divided) |
L sup. hepatic v. |
|
L hepatic v. |
Fig. 15.29 The parenchyma around the root of the left hepatic vein is carefully dissected by fragmentation and aspiration with a Cavitron Ultrasonic Surgical Aspirator while also ensuring a sufficient margin for dissection of
the vein. Then, a hemostat is applied to the vein and the specimen is excised. The stump is closed with a 5-0 Prolene suture
396 |
15 Left Lateral Sectionectomy |
|
|
Sutured stump of L hepatic v.
Falciform lig.
Cut edge of lesser omentum
Ligamentum teres
Fig. 15.30 After achieving hemostasis of the dissection plane, the falciform ligament is placed over the plane as a “lid.” If the ligament is broad enough, the entire plane can
be covered with the ligament. Suturing the ligament to the cut edge of the lesser omentum will result in a beautiful lid that you know will be secure
15 Left Lateral Sectionectomy |
397 |
|
|
Sutured stump of L hepatic v.
Dissection plane of liver covered by falciform lig.
Contour of caudate lobe
Fig. 15.31 After washing the abdominal cavity, an 8-mm duple drain is inserted via the right abdominal wall through the foramen of Winslow to the vicinity of the dis-
section plane of the liver. The operation is then completed by closing the abdominal wall, suturing in three layers
