
- •Foreword
- •Preface
- •Contents
- •1.1 Introduction
- •1.2 Prologue
- •1.9 Expansion of the Greater Omentum
- •3: Distal Gastrectomy
- •4: Total Gastrectomy
- •5.2 Part II: Thoracic Manipulation
- •6: Right Hemicolectomy
- •7: Appendectomy
- •8.6 Internal Pudendal Artery and Its Branches
- •8.13 Lateral Ligament
- •8.16 Fascia Propria of the Rectum: Part II
- •9: Sigmoidectomy
- •13: Hemorrhoidectomy
- •14: Right Hemihepatectomy
- •15: Left Lateral Sectionectomy
- •16: Laparoscopic Cholecystectomy
- •17: Open Cholecystectomy
- •Bibliography

8.13 Lateral Ligament |
239 |
|
|
8.11\ Structure ofthePrerectal Space
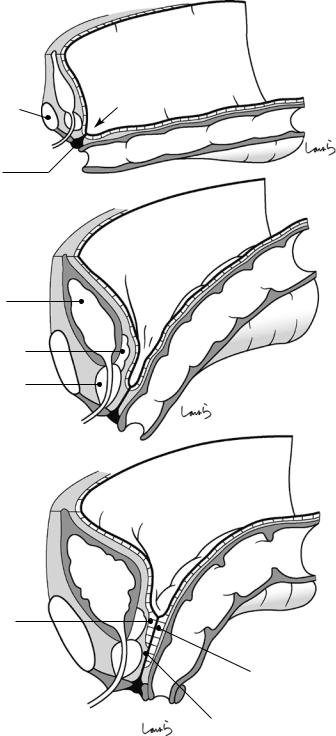
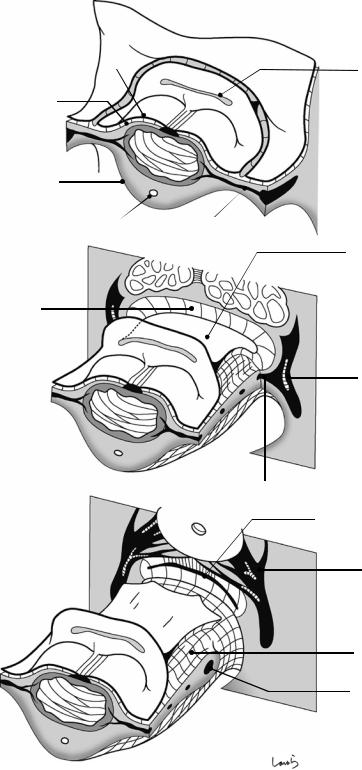
Let us take a look now at the anatomy of the prerectal space. During fetal life, there is a recess (the pouch of Douglas) between the rectum and the urogenital organs (seminal vesicle, prostate gland, and vagina) that is connected to the perineal body. As organs grow, the tip of the recess is pulled by the perineal body and then the peritoneum, accompanied by the subperitoneal fascia, fits into the recess. This forms a deep trough in that area. The apposed peritoneal membranes are then fused, and the lower end of the pouch of Douglas is closed. During this process, superficial epithelial cells are lyzed and fused with connective tissue to form “the fascia of Denonvilliers,” a structure consisting of essentially the same components as the fusion fascia of Toldt. The layer between the peritoneum and the subperitoneal fascia containing loose connective tissue forms a space as a result of the subperitoneal fascia folding back. Although the fascia of Denonvilliers, which descends like a thick curtain, partitions this space into the “prerectal space” on the rectal side and the “retroprostate space” on the prostate side, clinically both layers can be collectively recognized as the “prerectal space.” Another similarity of this fascia to the fusion fascia of Toldt is that the spaces both above and below the fascia can be entered.
which has descended along the sacrum, beyond the rectosacral fascia after reaching the coccyx, forming a single layer ( ). This fascia expands while covering the levator ani muscle and its tendon of insertion, the anococcygeal body (described in Figs. 8.3 and 8.4), and finally adheres to the rectum and merges with the fascia propria of the rectum. This turnaround point is the lower end of the supralevator space and the end point of retrorectal dissection.
Now let us look at the prerectal space. The objective of TME can be achieved only by prerectal dissection, but if that were true, the space either above or below the fascia of Denonvilliers could be entered. However, during actual surgery, it is more natural to enter above the fascia for ease of dissection and proceed with the fascia of Denonvilliers remaining attached on the rectal side. This will expose the seminal vesicle, which is covered only by the thin retroperitoneal fascia. Beyond the seminal vesicle, nerve fibers extending from the NVB enter between the fascia of Denonvilliers and the posterior surface of the prostate gland, making the retroprostate space narrower. So, the fascia of Denonvilliers needs to be dissected once so that the dissection layer can be switched to the prerectal space (route indicated by the arrow). This route also ends where the lower end of the fascia of Denonvilliers is connected to the perineal body. This is the end point of prerectal dissection.
8.12\ End Point of Preand Retro-
Rectal Dissection
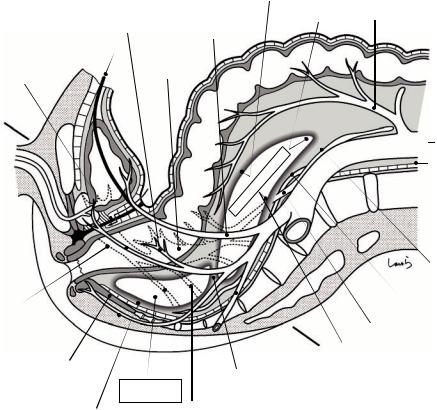
The fascial anatomy described in Figs. 8.9, 8.10, and 8.11 is illustrated in a sagittal cross section. The upper and lower borders of the retrorectal space are formed by the iliac triangle and the rectosacral fascia, respectively. The prehypogastric nerve fascia forming the posterior wall of the retrorectal space fuses with the presacral fascia,
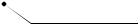
8.13\ Lateral Ligament
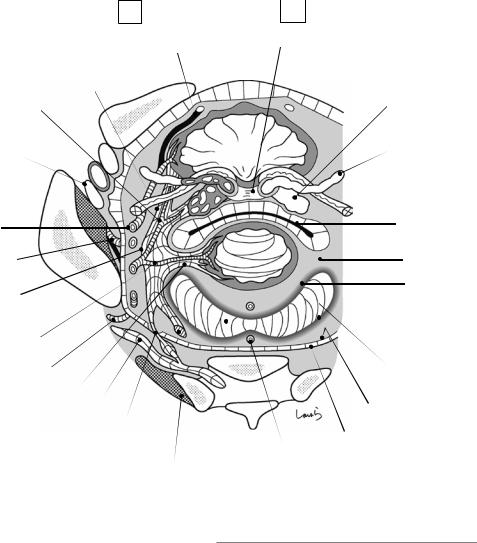
Figure 8.13 shows the look-down view of the cross section through line AB from Fig. 8.12. The plane at this level passes through the fascia of Denonvilliers, the lateral ligament, and the rectosacral fascia. The fascia, after turning around along the hypogastric nerve in a “ ” shape, surrounds the lateral ligament, which was driven into the rectum like a wedge, to complete its role as a mesenteric base. From this angle, it is clear
240 |
8 Anatomy of the Rectum and Surrounding Structures |
|
|
a
Pubis |
Recess |
|
Rectum
Perineal body
b
Bladder
Seminal vesicle
Prostate
c
Retroprostate space
Prerectal space
Fascia of Denonvilliers
Fig. 8.11 Structure of the prerectal space
8.13 Lateral Ligament |
241 |
|
|
Fascia propria of |
|
rectum |
Upper border of |
|
retrorectal space SRA |
Lateral |
Mid. rectal a. |
Sup. vesical |
|
|
|||
|
|
||
umbilical lig. |
|
|
|
Fascia of |
Pelvic plexus |
||
Denonvilliers |
|||
|
|
||
A
Retrorectal |
space |
|
Pre-sacral fascia
 Fascia transversalis
Fascia transversalis
Perineal  body
body
Sup. hypogastric plexus
NVB |
|
Med. sacral a. |
|
|
|
|
|
Hypogastric n. |
Inf. vesical a. |
|
B Pre-hypogastric |
Anococcygeal body |
|
nerve fascia |
Rectosacral |
|
|
Int. pudendal a. |
|
|
fascia |
Obturator a. |
|
|
|
|
Fusion of pre-hypogastric nerve |
Pelvic splanchnic n. |
|
|
|
|
fascia and pre-sacral fascia, forming a |
|
|
single layer (*) |
|
|
Fig. 8.12 End point of preand retro-rectal dissection
242 |
8 Anatomy of the Rectum and Surrounding Structures |
|
|
|
|
L |
|
R |
|
Lateral umbilical lig. |
Prostate gland (base) |
NVB
Inf. vesicala.
Femoral n.
V
A
N
Int. obturatorm.  Sup. vesical
Sup. vesical
Obturator a. & n.
Pelvic plexus
Mid. rectal a.
Seminal vesicle
Pubis
Vas deferens
|
Fascia of |
|
Denonvilliers |
|
R lateral lig. |
|
Fascia propria of |
SRA |
rectum |
Int. pudendal a. |
Pre-hypogastric |
|
n. fascia |
L laterallig. |
|
Sciatic n. |
Pre-sacral fascia |
|
|
Pelvicsplanchnic n. |
|
Hypogastric n. |
Fascia transversalis |
Rectosacral fascia |
Med. sacral a. |
Piriformism. |
|
Fig. 8.13 Lateral ligament
that the dorsal and ventral sides of the lateral ligament are lined by the turned-around fascia in the retrorectal and prerectal spaces, respectively. The spaces can be seen as the “inner moat” that surrounds the rectum, with the lateral ligament as a “dirt bridge” that connects the pelvic wall and the inner side of the moat (rectum). Beyond the lateral ligament, the rectum is no longer attached by the mesorectal base and is circumferentially surrounded by the fascia propria of the rectum (Fig. 8.15).
8.14\ Three-Dimensional
Construction of the Rectum
and Nerves
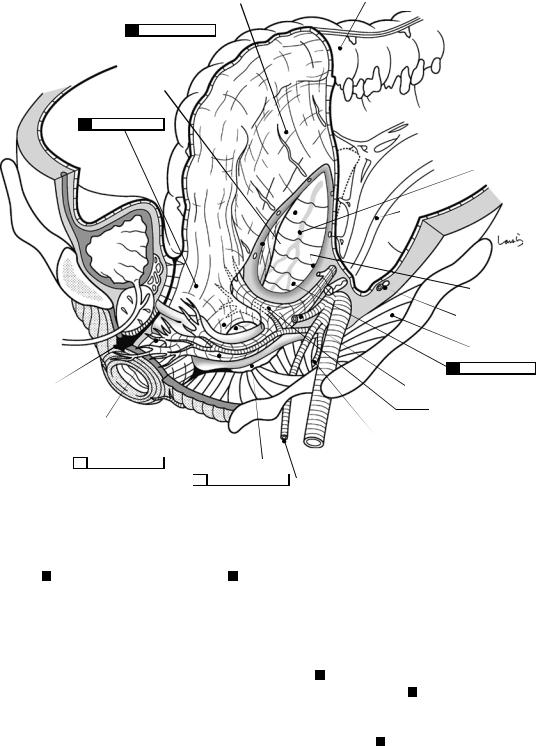
Figure 8.14 shows the three-dimensional construction of the rectum and surrounding structures with its five “spaces.” In this figure, approximately the front left quarter of the pelvis is cut off to expose the nerves and arteries. The fascia transversalis is omitted. Also, the left half of the peritoneum is detached so that the subret-
8.14 Three-Dimensional Construction of the Rectum and Nerves |
243 |
|
|
Subperitoneal fascia |
Peritoneum |
1
Fascia propria of rectum
4
*
Perineal body
Fascia of Denonvilliers and post. aspect of prostate gland
|
|
|
Ext. iliac a. |
5 |
|
|
Coccyx |
|
|
|
|
|
NVB and inf. vesical a. |
2 |
Int. obturator m. |
|
|
|
Fig. 8.14 Three-dimensional construction of the rectum and nerves
Sup. hypogastric
 plexus
plexus
Med. sacral a.
Ureter
Pre-hypogastric n. fascia
Gonadal a. & v.
Iliac m.
3
Sup. vesical a.
Lateral lig. and mid. rectal a.
Int. pudendal a.
roperitoneal fascia is exposed. The “retrorectal space” 1 and the “supralevator space” 2 are opened, but the rectosacral fascia, which partitions the two spaces, is unfortunately hidden behind the lateral ligament in this figure. The asterisk ( ) indicates the approximate area where the upper border of the retrorectal space is located.
Let us recap what we have covered so far. The right and left hypogastric nerves branching off from the superior hypogastric plexus merge with the pelvic splanchnic nerves derived from the S2–S5 spinal nerves to form the pelvic plexus. Part of the nerve bundle branches off at
a sharp angle as the lateral ligament and runs to the side of the Rb. The lower border of the retrorectal space is formed by the rectosacral fascia at the midpoint, but laterally, because the fascia turns around at the lateral ligament, the space ends at a slightly higher level (this bulging area is often referred to as the “laterorectal space” 3 ).
The “prerectal space” 4 is narrow in an anteroposterior direction but is wide enough in the transverse direction that it can be called the “pararectal space” 5. The fascia lining this space also turns around at the nerve bundle. Apart from the lateral ligament, the pelvic plexus also gives

244 |
8 Anatomy of the Rectum and Surrounding Structures |
|
|
off branches to the urinary bladder and the prostate gland (NVB). The fascia turns around at these nerve bundles while lining them from inside. So, dissection of the pararectal space should proceed by drawing an arc toward the lateral ligament while feeling for the roundedness of the rectum. If the dissection proceeds toward the side away from the rectum, the vesical branch or NVB may be damaged, causing not only bleeding, but possibly neuropathy.
8.15\ Fascia Propria of the Rectum:
Part I
The last sections of this chapter are devoted to simulating dissection around the Rb in TME. Although impossible to do in actual surgery, if we proceed with dissection around the rectum by gradually scraping off surrounding structures while preserving the rectum, the result would be what is shown in Fig. 8.15.
Figure 8.15a shows the Ra after retrorectal dissection has been completed. At this level, the mesorectal base, split into right and left, is opened to nearly 180 degrees and allows for passage of small nerve fibers extending from the hypogastric nerve into the rectum (rectal branches). Also, the SRA passes through the thick fat pad on the dorsal side of the rectum. These nerves and vessels are covered by the “fascia propria of the rectum” (in a narrow sense). By comparison, the ventral side of the rectum is covered by the peritoneum and the subperitoneal fascia. This subperitoneal fascia is, of course, a broad fascia lining the whole peritoneum, but in this area, there is no doubt that it is the “proper” fascia of the rectum. So, it can be interpreted that the broadly defined “fascia propria of the rectum” is a combination of the “anterior layer,” which continues from the subperitoneal fascia covering the ventral side of the rectum, and the “posterior layer,” which is the narrowly defined fascia propria of the rectum that covers the dorsal side of the rectum. It should also be noted that the broad subperitoneal fascia is referred to partially as the anterior layer of the renal fascia (fascia of Gerota) or the posterior
layer of the renal fascia (fascia of Zuckerkandl), and that “the anterior layer of the fascia propria of the rectum” is a term defined in the same way.
First, the peritoneum of the pouch of Douglas is incised to proceed deeper. Once a “recess” corresponding to the origin of the fascia of Denonvilliers is identified, the dissection proceeds around it. Figure 8.15b shows what is seen after the dissection has proceeded to the depth of the pelvic plexus. Compared with the small nerve fibers included in the mesenteric base, the lateral ligament derived from the pelvic plexus is a robust cord-like structure and has to be cauterized off.
It seems that the space above the fascia of Denonvilliers could be entered without problem in the anterior part. Dissection can advance easily between the fascia and the seminal vesicle and should be done without hesitating, although we should be careful when proceeding in an upper oblique direction so as to avoid damaging the NBV, which extends from the pelvic plexus toward the prostate gland when turning around the prerectal space.
Figure 8.15c shows what is left after the lateral ligament has been dissected. Because the lateral ligament is the last structure included in the mesorectal base, cutting this results in merging the anterior and posterior layers of the fascia propria of the rectum to a single membrane that surrounds the Rb circumferentially. This is why we can regard the subperitoneal fascia covering the ventral side of the rectum as the “anterior layer” of the fascia propria of the rectum in a broad sense. This means that, when looked at from another perspective, even perfect TME produces a slit-like defect in the fascia propria of the rectum at the mesorectal base. This also applies to excising the small intestine or colon because there is no fascia at the cut edge of the mesentery.
It would be difficult to proceed anteriorly due to the presence of nerve fibers from the NVB between the fascia of Denonvilliers and the posterior aspect of the prostate gland. So, we have no choice but to give up entering the space above the fascia of Denonvilliers and to cut off the fascia at this point. It seems that entering between
8.15 Fascia Propria of the Rectum: Part I |
245 |
|
|
a
Peritoneum
Subperitoneal fascia
Fascia propria of rectum
SRA |
Rectal br. |
|
b
Retroprostate space (layer above)
d
c |
Prostate |
|
Recess (origin of fascia of Denonvilliers )
 Hypogastric n.
Hypogastric n.
Fascia of Denonvilliers
 NVB
NVB
Pelvic plexus
Lateral lig.
Fascia of Denonvilliers (cut)
Prerectal space  (layer below)
(layer below)
NVB
Subperitoneal fascia (anterior layer of the broadly defined fascia propria of rectum)
Lateral lig. (dissected)
 Narrowly defined fascia propria of rectum
Narrowly defined fascia propria of rectum
(posterior layer of the broadly defined fascia propria of rectum)
Fig. 8.15 Fascia propria of the rectum: Part I
