
Cardiology / English / Internal_diseases_propedeutics._Part_II._Diagnostics_of_cardiovascular_diseases
.pdf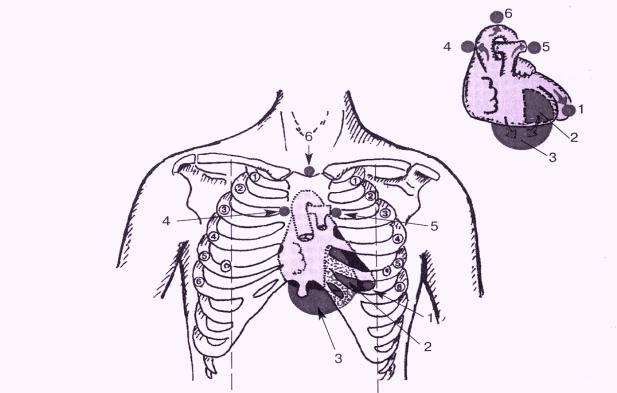
The properties of the apex beat (left ventricular) (AB): localization (specify intercostal space and the relation to the left midclavicular line), power (weakened, strengthened), square (limited, diffuse), the amplitude (high-amplitude — lift, lowamplitude), resistance, raise or not. In the norm the apex beat is localized in V intercostal space at 1.5 cm medially from the left midclavicular line, at the position on the left side is shifted by 1-1. 5 cm to the left, staying in the V intercostal space.
Fig. 1. Consequence of heart palpation
1. apex beat; 2. cardiac beat; 3. Epigastric pulsation; 4.aorta; 5.pulmonary atery; 6. the jugular fossa
(aorta)
11
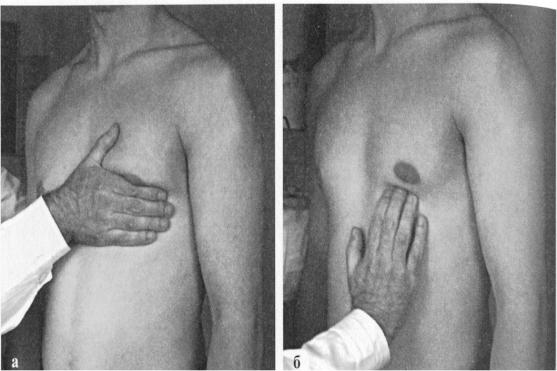
Fig.2 The position of the hands of the doctor at a palpation apex beat.
a. tentative palpation; b. the precise localization, square and power
The reasons for the displacement AB to the left — l eft ventricular hypertrophy
(LVH), right ventricular hypertrophy (RVH), right-sided pneumothorax and hydrothorax, pleuropericardial adhesions and fibrosis on the left.
The reasons for the displacement AB to the right - dextrocardia.
The reasons for the displacement AB up — pregnancy, |
ascites, meteorism, free gas |
in the abdominal cavity. |
|
The reasons for the displacement AB down — viscerop |
tosis, cachexia, post-Natal |
period. |
|
The reasons for the "disappearance" of AB — hydrope ricardium, left-sided hydrothorax.
The reasons for the increase in the area AB (diffuse) - LVH, thin chest, wrinkling the bottom edge of the left lung, enlarged intercostal space and the tumor of the mediastinum.
The reasons for the reduction of the AB (limited) — obesity, swelling of subcutaneous tissue, narrow intercostal space, pulmonary emphysema.
The reasons for increasing the amplitude and strength of the AB — LVH, physical activity, anxiety, thyrotoxicosis.
12
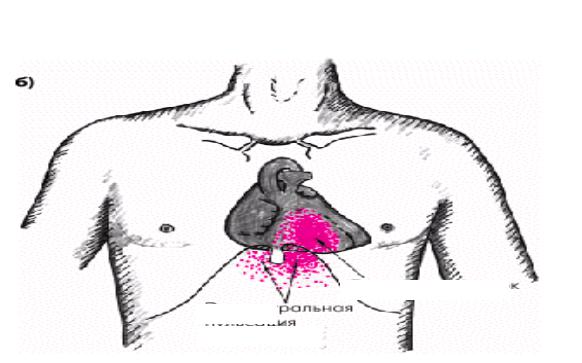
Cardiac (right ventricular)
pathological
epigastric pulsation
Fig. 3. Cardiac (right ventricular) beat and pathological epigastric pulsation. Cardiac (right ventricular) beat (CB) is a normal palpable as a faint pulsation in the
IV intercostal space at the left edge of the sternum. When hypertrophy and dilatation of the right ventricle shifts CB in the epigastric region, leading to pathological epigastric pulsation (Fig.3).
Thrills in the heart area – is determined by palpat ion. It is necessary to estimate its localization and relation to the phases of cardiac (systolic or diastolic) cycle. Mitral stenosis, for example, leads to diastolic thrill in the apex of the heart. Aortic stenosis leads to a systolic thrill in the II intercostal space to the left of the sternum.
Blood pressure may be measured satisfactorily with a sphygmomanometer of either the aneroid or the mercury type.
Examination of the jugular veins and their pulsations allows quite accurate estimation of the central venous pressure, and therefore gives important information about cardiac compensation.
Plesh test (Plesh J., 1878-1957, Hungarian therapist), syn.: abdominaljugular (or hepato-jugular) reflux. Positive Plesh test occurs in patients with CHF. Palm of the hand for short duration (10 seconds) is pressed against the projection area of the liver in the direction from the bottom upwards. Blood is displaced from the liver into the
13
inferior vena cava and then up to the right atrium, which is manifested by swelling of the neck veins and increase of venous pressure. Pressure on the anterior abdominal wall and an increase in venous blood flow to the heart normally, with adequate contractility of the right ventricle is not accompanied by swelling of the neck veins and increase in central venous pressure (CVP).
In patients with chronic heart failure, with a decrease in the pumping function of the right ventricle and the congestion in the veins of the systemic circulation, abdominaljugular test leads to increased swelling of neck veins and increases CVP at least on 4 cm of water column. Positive abdominal-jugular test indirectly reflects not only the deterioration of hemodynamics of the right heart, but also possible increase in left ventricular filling pressure, i.e. severity of bi-ventricular CHF.
Evaluation of abdominal-jugular test results in most cases helps to clarify the cause of peripheral edema, especially when patients have no significant neck veins extension or other external signs of right ventricular failure. Positive test results indicate the presence of congestion in the veins of the systemic circulation due to the right ventricular failure. Negative result of the test excludes heart failure as the cause of edema. In these cases, one should think of another genesis of edema (hypooncotic edema, shins deep vein thrombophlebitis, calcium antagonists intake, etc.).
Palpation of vessels
Localization of the abdominal aorta pulsation— the lean people, the epigastric region under the xiphoid process, but lower than in prostatic hyperplasia, decreases with a deep breath.
Localization of abnormal aortic arch aneurysm pulsation — the jugular fossa or the handle of the sternum, the so — called retrosternal pulsation.
Localization of abnormal extension of the ascending part of the aorta pulsation - to the right of the sternum in the second intercostal space.
14
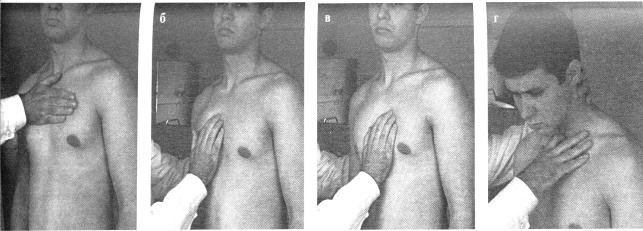
Fig.4. Consequence of vessel palpation.
Examination of arterial pulse. Properties of the pulse at the radial artery (a. radialis). Rate, rhythm, strain, filling, conture, quality of pulse. Equality of pulse on both limbs (Popov-Savelyev's sign).
Examples of changes of the pulse: when aortic stenosis is small, slow, rare; with aortic insufficiency – a large, galloping, frequent .
In case of arrhythmia, specify its type. Pulse deficiency (pulse deficiency is defined [counted] in the presence of atrial fibrillation, at early premature beats).
Arterial pulses can be palpated over the carotid, axillary, brachial, radial, femoral, popliteal, dorsalis pedis, and posterior tibial arteries.
Heart percussion
Main goals of heart percussion are:
1.Disclosure of ventricular and auricular dilation;
2.Disclosure of vascular bundle dilation.
Defining of relative cardiac dullness borders. At first right, left and upper borders of relative cardiac dullness are defined. It is necessary to obtain beforehand an indirect impression about the level of diaphragm standing which influences the results of percussion defining of relative cardiac dullness size. For this purpose the lower border of the right lung is defined along the midclavicular line which is normally located at the level of rib VI.
15
The level of diaphragm
The right border of relative cardiac
The upper border of relative cardiac dullness
The left border of relative cardiac dullness
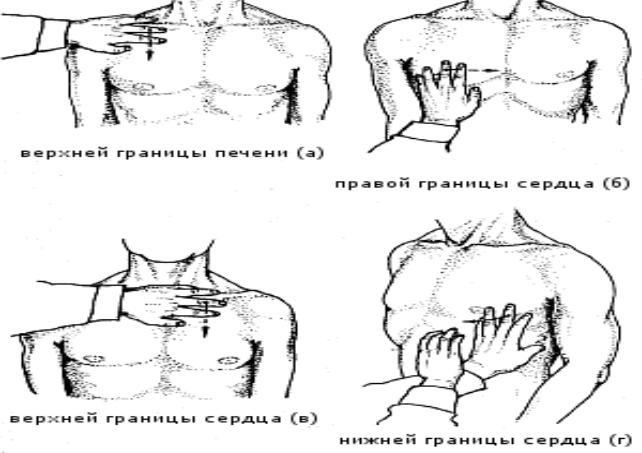
Fig.5. Starting position and future direction of pleximeter finger percussing the borders of relative cardiac dullness.
The right border of relative cardiac dullness, formed by the right atrium (RA), is found by percussing one rib above the found lower lung border (usually in the IV intercostal space), moving vertically placed pleximeter finger strictly along the intercostal space. Normally it situated at the right sternum edge or 1 cm laterally (Fig.5).
The left border of relative cardiac dullness formed by the left ventricle (LV) is defined after preliminary palpation of the apical impulse, usually in the V intercostal space, moving from anterior axillary line towards the heart. Normally it situated medial to the midclavicular line for 1-2 cm.
The upper border of relative cardiac dullness, formed by auricle of left atrium and pulmonary artery trunk is defined by percussing from top to bottom, 1 cm lateral from left sternal line (but not along left para-sternal line!). Normally it situated at the III rib level.
16
|
absolute (total) |
|
cardiac dullness |
The right border of relative |
The left border of relative |
cardiac dullness |
cardiac dullness |
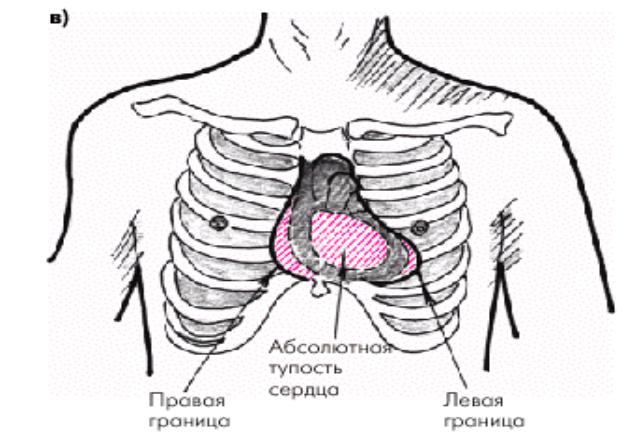
Fig.6. The relative and absolute (total) cardiac dullness borders
Normal borders of the absolute cardiac dullness: right - in the IV intercostal space along the left edge of the sternum, the upper - level of the lower edge IV R. at the left parasternal line, left - 1-2 cm medially from the left border of relative cardiac dullness.
Changes of heart dullness borders may be caused by extra cardiac reasons. So, while high diaphragm level heart takes a horizontal position that leads to increasing of the transverse heart size. At low diaphragm level heart takes a vertical position, and, accordingly, its transverse size becomes less. Pleural fluid or free pleural air in one of the pleural cavities brings to displacing of .the cardiac dullness borders to the healthy side, atelectasis or lung shrinking, fibro thorax – to th e sore side. Area of superficial cardiac dullness sharply decreases or disappears at the emphysema and increases at the lung shrinking. Increase of superficial cardiac dullness area also occurs in heart ante displacement by mediastinal tumour, pericardium effusion, right ventricle dilation.
17
Relative cardiac dullness borders are displaced because of the heart chambers dilation. Relative dullness borders displacement to the right is caused by right atrium and right ventricle dilation. Relative dullness is displaced upwards because of left atrium and pulmonary artery trunk dilation. Relative dullness borders displacement to the left is the result of left ventricle dilation. It is necessary to remember, that sharply dilated and hypertrophied right ventricle shoving back the left ventricle also can displace relative dullness border to the left. Aortic dilation leads to dullness diameter increase in the 2nd intercostal space.
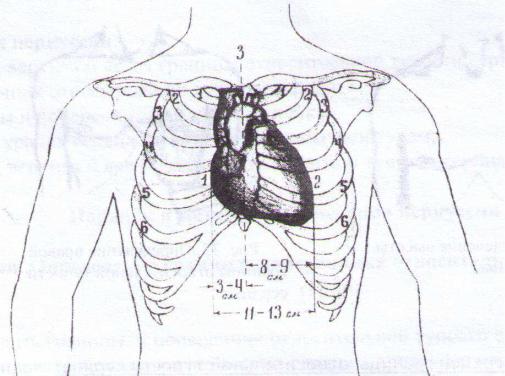
Measurement of heart diameter. For measurement of heart diameter the distances from right and left borders of relative cardiac dullness to midsternal line are defined. Normally these distances make respectively 3-4 cm and 8-9 cm, and heart diameter makes 11-13 cm (Fig.7).
Fig.7. Measurement of heart diameter.
Defining of vascular bundle borders. The vascular bundle including aorta, vena cava superior and pulmonary artery is not simple to percuss. Soft percussion is applied, moving vertically placed pleximeter finger along the II intercostal space on the right and on the left towards the sternum. Normally vascular bundle borders coincide with right and left edges of the sternum, its width doesn't exceed 5-6 cm (Fig.8).
18
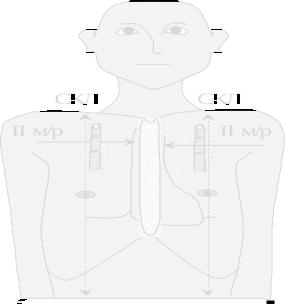
Fig.8. Defining of vascular bundle borders
Defining of heart configuration. For defining of heart configuration the borders of right and left contours of relative cardiac dullness are additionally defined by percussing in the right III intercostal space and in the left III and IV intercostal spaces. Having connected all the points corresponding the borders of relative cardiac dullness, one can obtain the idea about heart configuration. Normally an obtuse angle is clearly defined along the left heart contour between the vascular bundle and the left ventricle - the socalled waist of the heart.
The arc of the right contour of the heart in norm – vena cava superior– on the edge of the sternum to R. III, right atrium in the 3-4 intercostal spaces 1 cm outwards from the right edge of the sternum. The angles of the right contour of the heart in norm – angle between vena cava superior and right atrium and between the right atrium and diaphragm in the 5 intercostal space from the sternum.
The arc of the left contour of the heart in norm - I intercostal space at the edge of the sternum - aortic arch, II intercostal space at the sternum – the arc of the pulmonary artery, level III R. over the edge of the sternum arc of the left atrium, below the arc of the left ventricle.
The "waist" of the heart is the angle between the vascular bundle and the arc of the left ventricle. The vertex of this angleleft atrium auricle . With the increase of LP waist
heart "smoothed", while increasing the LV – "stress ed".
19
Mitral configuration I - waist heart smoothed at the expense of hypertrophy of the left atrium, the vascular bundle can be extended due to the dilatation the pulmonary artery, it is possible to laterally shift the right border of relative cardiac dullness due to right ventricle hypertrophy with the development of pulmonary hypertension; the reason for the configuration is mitral stenosis.
Hemodynamics abnormalities in mitral stenosis
In compensation stage of disease: the area of mitral ostium is significantly less than normal (4-6 cm2), that leads to left atrium repletion with blood. This blood had not time to move to the left ventricle, and there is also blood, arrived from pulmonary veins. It results in left atrium hypertrophy.
In decompensation stage of disease: left atrium contractility is decreased, pressure within it increases, that leads to the pressure rise within the pulmonary veins and pulmonary capillaries. The latter leads to switching on Kitaev's reflex – the pressure rise within the pulmonary veins ostii causes the narrowing of the pulmonary arteriolesand when pressure rising within the pulmonary artery and further overload and hypertrophy of the right ventricle. The left ventricle diminishes at the rate because it performs the less work (Application Fig.4).
Mitral configuration II - the reason for the configuration is mitral incompetence. Mitral valve incompetence (insufficientia valvulae mitralis) appears in that cases
when mitral valve on left ventricle systole incompletely closes left atrioventricular ostium and blood regurgitates from the ventricle to the atrium. Mitral incompetence may be organic and functional.
Organic mitral incompetence more frequently appears as a result of rheumatic endocarditis due to which connective tissue develops in valve leaflets and later on it is wrinkled and causes shortening of leaflets and attached chordae tendinae. As a result of these changes valve edges during systole closes incompletely, forming a chink through which in ventricle contraction the part of blood regurgitates into the left atrium. Rarely wrinkling of valve leaflets and shortening of chordae tendinae develops as a result of atherosclerosis.
20
