
Cardiology / English / Internal_diseases_propedeutics._Part_II._Diagnostics_of_cardiovascular_diseases
.pdf-Reduced |
HDL |
|
-symptomatic arterial disease |
|
cholesterol |
|
|
Advanced |
hypertensive |
-Raised LDL cholesterol |
|
retinopathy |
|
|
-Microalbuminuria |
in |
|
-haemorrhages or exudates |
|
diabetes |
|
|
-papilloedema |
|
-Impaired |
glucose |
|
|
|
tolerance |
|
|
|
|
-Obesity |
|
|
|
|
-Sedentary lifestyle |
|
|
|
|
-Raised fibrinogen |
|
|
|
|
-High risk socioeconomic |
|
|
|
|
group |
|
|
|
|
-High risk ethnic group |
|
|
|
|
-High risk geographic |
|
|
|
|
region |
|
|
|
|
|
|
|
|
|
1 - "Target Organ Damage" corresponds to previous WHO Stage 2 hypertension
2 "Associated Clinical Conditions" corresponds to previous WHO Stage 3 hypertension.
Table 9.
Stratification of Risk to Quantify Prognosis
Other |
Risk |
Grade 1 |
Grade 2 |
Grade 3 |
|
Factors |
& |
SBP 140-159 or |
SBP 160-179 or |
SBP і 180 or |
|
Disease History |
DBP 90-99 |
DBP 100-109 |
DBP і 110 |
|
|
|
|
|
|
|
|
I. no other |
risk |
LOW RISK |
MED RISK |
HIGH RISK |
|
factors |
|
|
|
|
|
|
|
|
|
|
|
II. 1-2 risk |
MED RISK |
MED RISK |
V HIGH RISK |
|
|
factors |
|
|
|
|
|
|
|
|
|
|
|
III. 3 or more risk |
HIGH RISK |
HIGH RISK |
V HIGH RISK |
|
|
|
|
|
|
|
|
|
|
|
71 |
|
|
factors or |
TOD1 |
|
|
|
|
|
or diabetes |
|
|
|
|
|
|
|
|
|
|
|
|
|
IV. ACC2 |
|
V |
HIGH |
V |
HIGH |
V HIGH RISK |
|
|
RISK |
|
RISK |
|
|
|
|
|
|
|
|
|
Risk strata (typical 10 year risk of stroke or myocardial infarction): Low risk = less than 15%; medium risk = about 15-20% risk; high risk = about 20-30%; very high risk = 30% or more
1.TOD – Target Organ Damage (Table 2)
2.ACC – Associated Clinical Conditions, including clinical cardiovascular disease or renal disease (Table 8)
Classification of essential hypertension (hypertensive disease)
According to great attention to cardiovascular risk evaluation in hypertensive patients there is designed transition to classifications with distinction of BP elevation grades with simultaneous risk assessment (low, medium, high, very high). This approach was stipulated in WHO and ISAH experts recommendations (1999) and was supported in Russian national recommendations on AH (2000). Recently used in Russia classifications are presented below. Until now classification of essential hypertension (hypertensive disease) by WHO (1962) is widespread in Russia.
Classification of essential hypertension (hypertensive disease) by WHO (1962).
I stage — BP elevation >160/95 mmHg without organic changes of cardiovascular system;
II stage — BP elevation > 160/95 mmHg in combinatio n with changes of target organs (heart, kidneys, brain, fundal vessels), caused by hypertension, but without their functional alterations;
III stage — hypertension, combined with target orga ns damage (heart, kidneys, brain, fundal vessels) with their functional alterations.
72
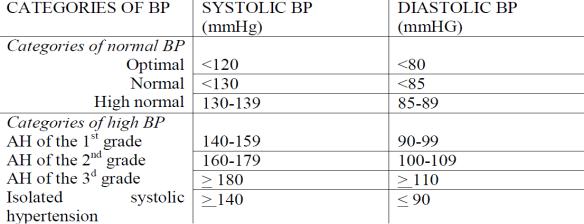
Table 10
Definitions and Classification of Blood Pressure Levels
Recently both classifications are recommended in Russia; it is necessary to indicate stage of disease as well as BP grade.
Clinical manifestations depend on damage of target organs.
Many of patients are asymptomatic, and frequently hypertension is detected occasionally. There may be neurosis signs, headaches, particularly in the mornings; nausea, flashing of ―midges in front of eyes; pain in precordium, palpitation, rapid fatigability, epistaxis (nasal bleedings), hyperexcitability, irritability, sleep disturbance. In later stages coronary events may appear. Severity of these symptoms, in particular, headaches, not always corresponds to BP elevation grade.
On medical history analysis it is necessary to obtain information about family history of hypertension as well as other conditions, worsening prognosis in their presence – diabetes mellitus, coronary heart disease, stroke, dyslipidemia. Information about duration and level of BP arising, previous drug and non-pharmaceutical therapy effectiveness are important. It is necessary to elicit patient's lifestyle peculiarities, including diet (fats, excessive salt and alcohol consumption), smoking, physical activity level, excessive body mass or obesity.
On examination one attracts attention on excessive body mass. A face hyperemia as well as pallor due to peripheral arteriolar spasm are noticed.
On heart examination sign of left ventricular hypertrophy (apical impulse shift to the left) - key syndrome in hypertension - is detected, that confirmed by ECG, X-ray and,
73
especially, ECO examinations. On elevated BP there is typical pulse strain increase, due to grade of which may be approximately assessed level of BP. Moreover, elevated BP is characterized by accent of S2 at the aorta appearance.
ECG changes are initially characterized by decrease of T-wave amplitude in the left chest leads. Left ventricular hypertrophy is revealed by high-amplitude R-wave with oblique depression of ST segment in V4-6. Left bundle-branch block may develop.
On ECO hypertrophy of interventricular septum and left ventricular posterior wall is verified. Sometimes these changes are accompanied by dilatation, increase of end-systolic and end-diastolic left ventricular dimensions. Appearance of hypokinetic and even dyskinetic zones in the myocardium is the sign of left ventricular contractile capacity decline.
Different metabolic disorders: hyperinsulinemia, impaired glucose tolerance (in some cases – diabetes mellitus, type II), dyslipide mia (reduced HDL cholesterol, raised LDL cholesterol), obesity were frequently marked during last years.
Hypertensive crisis. Clinical course of hypertension may be complicated by hypertensive crisis. It is fast, additional, significant BP rise. It may be provoked by different physical and mental loading, excessive dietary sodium, water, alcohol intake; cessation of drug therapy. Very high BP is detected in patient (diastolic BP may exceed 130—140 mmHg). In the majority of cases on the back ground of such BP elevation cerebral signs (nausea, vomiting, vision reduction) appear.
Simultaneously or later other signs and complications of hypertension may increase: coronary heart disease (CHD) exacerbation, acute left-sided heart failure occurrence and stroke. On severe crisis fundal hemorrhages, papilledema may appear.
Kidneys damage. During the late stage of hypertension due to arteriolosclerosis development the signs of kidneys damage appear: impaired concentrative capacity, decrease of urine relative density, proteinuria, hematuria, and in the terminal stage – azotic wastes retention. Parallel signs of eyes fundum damage develop: increasing retinal arteries narrowing and tortuosity, especially in comparison with veins; veins dilation, may be fundal hemorrhages, and later degenerate foci in retina.
74
Central nervous system damage determines various signs, concerned with intensity and location of vascular disorders. Vascular narrowing (due to their spasm) leads to focal brain ischemia with partial fall-out of its functions and in more severe cases is accompanied by brain hemorrhages. In sharp BP elevation there may be arterial wall ruptures with massive hemorrhage.
Primary hypertension is asymptomatic until complications in target organs develop (eg, left ventricular failure, atherosclerotic heart disease, cerebrovascular insufficiency with or without stroke, renal failure). Dizziness, flushed facies, headache, fatigue, epistaxis, and nervousness are not caused by uncomplicated hypertension.
A fourth heart sound and broad, notched P-wave abnormalities on the ECG are among the earliest signs of hypertensive heart disease. Echocardiographic evidence of left ventricular hypertrophy may appear later. Chest x-ray is often normal until the late dilated phase of hypertensive heart disease. Aortic dissection or leaking aneurysm of the aorta may be the first sign of hypertension or may complicate untreated hypertension. Polyuria, nocturia, diminished renal concentrating ability, proteinuria, microhematuria, cylindruria, and nitrogen retention are late manifestations of arteriolar nephrosclerosis.
Retinal changes may include retinal hemorrhages, exudates, papilledema, and vascular accidents. On the basis of retinal changes, Keith, Wagener, and Barker classified hypertension into groups that have important prognostic implications: group 1-- constriction of retinal arterioles only; group 2--constriction and sclerosis of retinal arterioles; group 3--hemorrhages and exudates in addition to vascular changes; group 4 (malignant hypertension)--papilledema.
Diagnosis
Diagnosis of primary hypertension depends on repeatedly demonstrating higher- than-normal systolic and/or diastolic BP and excluding secondary causes
ATHEROSCLEROSIS. ISCHEMIC HEART DISEASE
Atherosclerosis is a form of arteriosclerosis characterized by patchy subintimal thickening (atheromas) of medium and large arteries, which can reduce or obstruct blood flow. Atherosclerotic plaque consists of accumulated intracellular and extracellular lipids,
75
smooth muscle cells, connective tissue, and glycosaminoglycans. Circulating low-density lipoprotein (LDL) migrate through the endothelial barrier of the arterial wall and penetrate into the intima. Some plaques, covered by a thin fibrous cap, may undergo spontaneous fissure or rupture. These plaques are unstable or vulnerable and are more closely associated to the onset of an acute ischemic event.
Ischemic heart disease (IHD; also known as coronary heart disease (CHD) is usually caused by structural disorder of the coronary arteries (coronary artery disease − CAD).
Ischemic heart disease produces six clinical syndromes:
-angina pectoris − stable or unstable, and variant ;
-myocardial infarction (MI);
-postMI cardiosclerosis or old MI;
-heart failure;
-arrhythmias;
-sudden cardiac death.
76
Ischemic heart disease has uncontrollable (advanced age, male sex, genetic predisposition) and modifiable [smoking (risk is almost double), hypertension (risk is double if systolic blood pressure is >180 mm Hg), hyperlipidemia, glucose intolerance or diabetes mellitus, obesity (weight >30% over ideal), hypothyroidism, left ventricular hypertrophy (LVH), sedentary life-style, oral contraceptive use, cocaine use, low serum folates level) risk factors.
Angina pectoris is characterized by discomfort that occurs when myocardial oxygen demand exceeds the supply. Myocardial ischemia can be asymptomatic (silent ischemia), particularly in diabetics.
Pain is located behind the sternum. The usual distribution is referral to all or part of the sternal region, the left side of the chest, and the neck and down the ulnar side of the left forearm and hand.
The most important diagnostic factor is the history.
The physical examination is of little diagnostic help and may be totally normal in many patients.
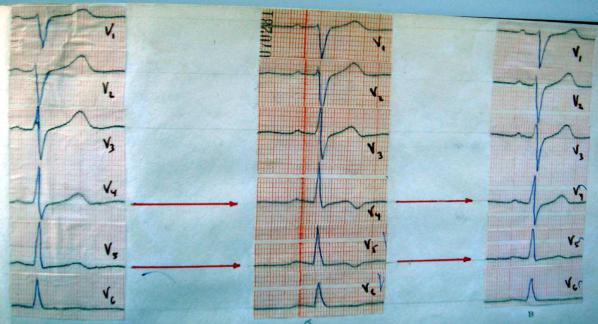
An ECG taken during the acute episode may show transient T-wave inversion or STsegment depression or elevation (may be either convex and concave), but some patients may have a normal tracing.
Fig.27. ECG before, during attack of angina pectoris and after taking nitrates.
77
Ambulatory (Holter) electrocardiographic monitoring can detect silent ischemia (ischemic ECG changes without accompanying symp-toms), which occur in >50% of patients with unstable angina.
Coronary angiography is performed to define the location and extent of coronary disease; this is indicated in selected patients who are candidates for CABG (coronary artery bypass grafting) surgery or angioplasty.
Myocardial infarction (MI) is characterized by necrosis resulting from an insufficient supply of oxygenated blood to an area of the heart.
One distinguishes:
-non−Q wave MI: Area of ischemic necrosis is limit ed to the inner one third to half of myocardial wall;
-Q wave MI: Area of ischemic necrosis penetrates the entire thickness of the ventricular wall. MI may be caused by
• Coronary atherosclerosis
• Coronary artery spasm
• Coronary embolism (caused by infective endocarditis, rheumatic heart disease, intracavitary thrombus)
• Periarteritis and other coronary artery inflammat ory diseases
•Dissection into coronary arteries (aneurysmal or iatrogenic)
•Congenital abnormalities of coronary circulation
•MI with normal coronaries (MINC syndrome): more f requent in younger patients and cocaine addicts.
Echocardiography can evaluate wall motion abnormalities and identify mural thrombus or mitral regurgitation, which can occur acutely after MI.
Clinical presentation of MI:
•Crushing substernal or retrosternal chest pain usually lasts longer than 30 min.
•Pain is unrelieved by rest or sublingual nitroglycerin or is rapidly recurring.
•Pain radiates to the left or right arm, neck, jaw, back, shoulders, or abdomen and is not pleuritic in character.
•Pain may be associated with dyspnea, diaphoresis, nausea, or vomiting.
78
•There is no pain in approximately 20% of infarctions (usually in diabetic or elderly patients).
Physical findings:
Skin may be diaphoretic, with pallor (because of decreased oxygen).
•Rales may be present at the bases of lungs (indic ative of CHF).
•Cardiac auscultation may reveal an apical systoli c murmur caused by mitral regurgitation secondary to papillary muscle dysfunction; S3 or S4 may also be present.
•Physical examination may be completely normal.
•Serum cardiac enzyme studies: damaged necrotic he art muscle releases cardiac isoenzymes (CK, LDH) into the blood stream in amounts that correlate with the size of the infarct. Electrophoretic fractionation of the enzymes can pinpoint certain isoenzymes (CK-MB and LDH-1) that are more sensitive indicators of MI than total CK or LDH. • Cardiac troponin levels: cardiac-specific troponin T (cTnT) and cardiacspecific troponin I (cTnI) are new markers for acute Ml.
On the ECG in Q wave infarction, there is development of: Common signs
1. (-)T: (ischemia);
2. ST ABOVE CONTOUR, a synonym for "monophasic curve" (damage heart muscle);
3. PATHOLOGICAL Q (necrosis of the heart muscle): the extension Q > 0,03; Q > 1/4R;
4. The DISCORDANCE of the OFFSET ST: ST in leads opposite to the localization of infarction;
5. DYNAMICS (acute phase (injury)-acute-subacute-cicatricial stage). STAGE OF MIOCARDICAL INFARCTION (table 11).
1. Stage of ISCHEMIA;
2. PREACUTE phase (stage of injury): ST above contour;
3. In the ACUTE stage (formation of necrosis): ST above contour with the transition in (-) T; the formation of pathological Q;
79
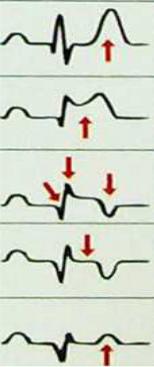
4.SUBACUTE stage (resorption, proliferation, reparation and organization in the scar area): ST on the contour, T (-), pathological Q;
5.SCAR stage (final consolidation of the scar): ST on the contour, T (-) or (+), pathological Q – in this case, the sign of the scar .
The duration of the stages is subject to the rule of the Troika and the increases on the
rise:
(ISCHEMIA PHASE),
up to 3 days (PREACUTE STAGE),
to 3 weeks (ACUTE PHASE),
to 3 months (SUBACUTE STAGE),
the rest of life (SCAR STAGE).
|
|
|
|
|
Table 11. |
|
|
|
STAGE OF MIOCARDICAL INFARCTION |
||
|
|
|
|
|
|
STAGE |
|
|
DURATION |
|
SIGN |
|
|
|
|
|
|
Stage |
|
of |
|
|
high pointed (coronary) T |
ISCHEMIA |
|
|
to 30 min |
|
wave |
|
|
|
|
|
|
PREACUTE |
|
|
|
|
ST above contour |
phase |
|
|
up to 3 days |
|
|
|
|
|
|
|
|
ACUTE stage |
|
to 3 weeks |
|
ST above contour with the |
|
|
|
|
|
|
transition in (-) T; the |
|
|
|
|
|
formation of pathological Q; |
|
|
|
|
|
|
SUBACUTE |
|
|
|
ST on the contour, T (-), |
|
stage |
|
|
to 3 months |
|
pathological Q; |
|
|
|
|
|
|
SCAR |
stage |
the rest of life |
|
ST on the contour, T (-) or |
|
(final |
|
|
|
|
(+), pathological Q |
consolidation |
of |
|
|
|
|
the scar) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
80 |
|
