
Cardiology / English / Internal_diseases_propedeutics._Part_II._Diagnostics_of_cardiovascular_diseases
.pdfIn functional or relative mitral incompetence mitral valve is not changed but its ostium is enlarged and valve leaflets close it incompletely. Relative incompetence may develop owing to left ventricle dilatation in myocarditis, myocardidystrophy, myocardiosclerosis, when circular muscle fibers, forming muscle ring around the atrioventricular ostium weaken, and also in papillary muscles damage.
Hemodynamics abnormalities
Hemodynamics in mitral incompetence is characterized by partial blood regurgitation into the left atrium in incomplete closure of mitral valve leaflets. The atrium filling increases since the regurgitated part of blood adds to usual blood volume, arrived from pulmonary veins. Pressure in the left atrium increases, it dilates and hypertrophies.
During diastole greater than normal blood volume flows from overfilled left atrium into the left ventricle, that leads to left ventricle overfilling and dilatation. Left ventricle should work with overload, due to which its hypertrophy develops. Overwork of hypertrophied left atrium and left ventricle protractedly compensates possessed mitral incompetence (Application Fig. 1-3).
In decrease of hypertrophied left atrium contractile capacity congestive phenomena in lesser circulation circle appear and pressure rises, that demands overwork of right ventricle.
So in time in mitral incompetence the right ventricle hypertrophy may develop.
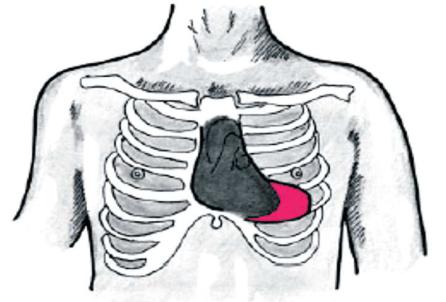
On the heart percussion its dullness enlargement to the left and upwards due to left atrium and left ventricle dilatation is revealed. The heart acquires mitral configuration with smoothed cardiac waist. On right ventricle hypertrophy cardiac dullness also shifts to the right (Fig. 8,9).
21

Fig.8. Radiography of t he chest in combined heart defect shows mitral configuration of the heart.
Fig.9. Mitral configuration II of the hea rt.
Aortic heart configur ation – the reasons of this configurati on are stenosis of aortic ostium and aortic incompetence, arterial hypertension.
22
Stenosis of aortic ostium (aortic stenosis, stenosis ostii aortae) creates difficulty for blood ejection into aorta on the left ventricle contraction. Acquired aortic valve stenosis often results from progressive degeneration and calcification of a congenitally bicuspid valve. Rheumatic fever, bacterial endocarditis and arteriosclerotic degeneration are rarer causes.
This valve disease appears owing to adhesion of valve cusps or fibrous narrowing of aortic orifice.
Hemodynamics abnormalities
A little narrowing of aortic orifice doesn’t cause significant circulation alteration. If the degree of stenosis is high, during systole the left ventricle empties incompletely, as all blood volume has no time to pass across narrow orifice into aorta. On diastole normal blood volume from the left atrium adds to this residual blood portion, that leads to left ventricle overfilling and pressure rising within it. This abnormality of intracardiac hemodynamics is compensated by left ventricle overwork, and causes its hypertrophy (Application Fig.7)
On percussion the displacement of relative dullness borders to the left and aortic heart configuration (with accentuated cardiac waist), caused by left ventricular hypertrophy are detected (Fig.10,11).
Fig.10. Aortic heart configuration.
23

Fig.11. Radiograph y of the chest in aortic incompetence s hows typical aortic configuration of the heart.
Aortic incompetence (i nsufficientia valvulae aortae) is valv e disease in which the semilunar cusps close in completely the aortic orifice and during diastole blood regurgitates from aorta into left ventricle. Aortic regurgitation oc curs if the aortic valve ring dilates, as a result of dissecting aneurysm, ankylosing spondylitis or syphilis for example, or if the valve cu sps degenerate, such as after rheumat ic fever, atherosclerotic lesion or endocarditis.
Anatomical changes d epend on etiology of aortic lesion. After rheumatic fever inflammatory-sclerotic process at the base of valvular cusps lead s to their wrinkling and shortening. In syphilis and a therosclerosis pathologic process may affect only aorta itself, causing its dilatation and taking-up of valvular cusps with out their affecting, or connective tissue expands on valvular cusps and deforms the m. In sepsis ulcerous endocarditis leads to destruction of valve parts, defects forming in the cusps and their subsequent scarring and sho rtening.
Hemodynamics abnor malities
In aortic incompetence during diastole blood comes in the left ventricle not only from left atrium but regurgitates from aorta too. It causes left ventricle overfilling and
24

stretching on diastole. Durin g systole left ventricle contracts with grater force to eject into aorta increased stroke volu me. Left ventricle overwork leads to its hypertrophy, and increase of systolic blood vo lume in aorta causes its dilatation . Sharp fluctuation of blood pressure within aorta during systole and diastole is characteristic for aortic incompetence. Increased as compared with normal blood volume within aorta during systole causes increase of systolic blood pressure, and as a part of blood vo lume regurgitates into ventricle during diastole, dia stolic pressure rapidly decline (Application Fig.5-6).
"Trapezoidal" config uration of the heart - the heart has a trapezoid shape, waist of the heart, angle between vena cava superior and right atrium a nd angle between right atrium and diaphragm "di sappear", the reason of configuration is hydropericardium (Fig.12).
Fig.12 "Trapezoidal" configuration of the heart.
" Spherical” configuration of the heart when the ventricular septal defect due to the discharge of blood from the left to the right ventricle.
25

Fig.13"Spherical” configuration of the heart. in a patient with a congenital heart defect. The chest radiograph of a patient with a ventricular septal defect (direct view): the shadow of the heart increased at the expense of both ventricles, visible bulging arc pulmonary trunk (arrow), pulmonary picture in the basal parts of the lungs are strengthened.
"Drip" configuration of the heart - the left and right border of cardiac dullness is shifted medially, the area of cardiac dullness is diminished, the heart becomes "drip" form, cause - emphysema of the lungs (Fig.14).
26
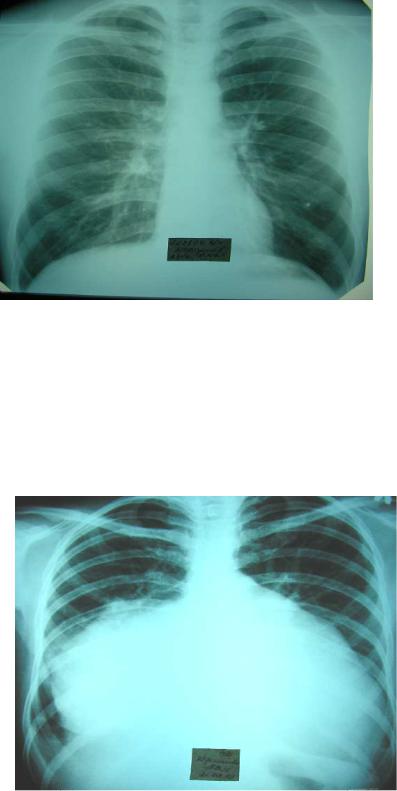
Fig.14. "Drip" configuration of the heart
"Cor bovinum" ("bu ll" heart) - the area of cardiac du llness is increased by hypertrophy and/or dilatatio n of its main offices in cardiomyopathy, advanced forms of heart failure.
Fig.15. "Cor bovinum"
27
Auscultation of the heart and blood vessels.
Auscultation points of the heart valves do not coincide with the projection places of the valves on the anterior chest wall (only pulmonic valve auscultation point practically coincides with the projection of the pulmonary artery valve).
Places of three heart valves projection - pulmonary, aortic and mitral - are located very close to each other, about the place of the III rib attachment to the sternum (therefore to distinguish particular sounds associated with damage of each of these valves, when listening to their places of projection is not possible). The diameter of the valves openings is large enough and is 2-3 cm for pulmonary, aortic and mitral valves and 3-6 cm for tricuspid valve. Therefore, in determining the projection of the heart valves it must be taken into account their length, as projection of the valve is not the point, but rather the line of few centimeters.
The surface projections of the heart valves on the anterior chest wall (approximately) are as follows (Fig. 16):
1.The pulmonic valve is located at the place of attachment of the upper edge of III left costal cartilage to the sternum (1/2 portion of the valve is located behind the rib cartilage, 1/2 part of the valve-behind the sternum).
2.Aortic valve is located just medially, slightly lower and deeper than pulmonary valve - almost in the middle of the sternum at the level of the III mid-rib.
Bicuspid (mitral) and tricuspid atrioventricular valves are located behind the sternum in the arcuate line connecting places of the lower part of the left III rib cartilage and the right V-VI costal cartilages attachments to the sternum.
3.Bicuspid (mitral) valve is located within the limits of upper third of this line and is located in between the attachment place of the lower edge of the III rib cartilage to the sternum and the level of the third left intercostal space.
4.Tricuspid valve is within the limits of lower 2/3 of this line and is located in between the level of the left third intercostal space and the attachment point of the right V costal cartilage to the sternum (in fact, in the lower part of the sternum body).
28
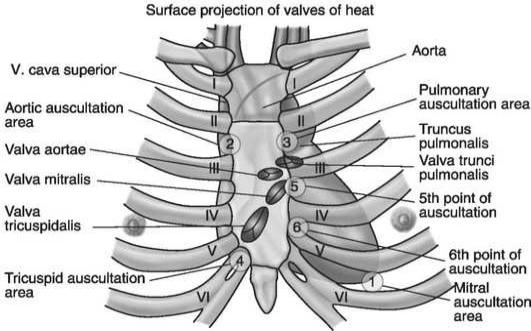
Fig. 16. Projection of the heart valves on the anterior chest wall and their auscultation points
Since all the heart valves are located close to each other, to evaluate the sound effects associated with the work of each valve there are used more remote points from the valves location, where the sound is carried either by the flow of blood, or by myocardium of the heart area, where this sound is produced and where the summation of the sounds originating in neighboring parts of the heart is minimal.
There are distinguished the 6 heart auscultation points: 4 main and 1 additional points.
«Assignment» numbers to the auscultation points (1st auscultation point, 2nd auscultation point, etc.) and listening to the heart valves in this sequence in clinical practice is determined by the frequency of their damage (i.e. the most frequently damaged mitral valve, and most rarely - tricuspid one).
1. The first auscultation point - region of the apical impulse (normally - the V intercostal space slightly medially from l. medioclavicularis sinistrum, in the pathology, apical impulse may be displaced considerably from its location in the norm). At this point, mitral (bicuspid) valve is well heard. This is because in its projection (behind sternum at the level of the lower edge of the III rib cartilage - 3rd intercostal space) mitral valve is rather deeply spaced apart from the chest wall (i.e. the sounds from it are not properly
29
heard), and at the apex of the heart, which is formed by the left ventricle, mitral valve
sounds are well conducted by dense heart muscle.
2.The second auscultation point-2nd right intercostal space close to the sternum. This point is a place of the aortic valve auscultation. As mentioned above, the aortic valve is projected on mid-sternum at the level of the III rib middle, but it is common to listen to the aorta in the right 2nd intercostal space, because aorta here comes close to the anterior chest wall and here aortic valve sounds are well conducted along by the flow of blood and the wall of the aorta.Therefore, when listening to the right 2nd intercostal space, one can be sure that the sounds and murmurs belong exactly to the aortic valve.
3.The third auscultation point - 2nd left intercostal space close to the sternum. This point is very close to the projection of the pulmonic valve (attachment of upper edge of the III costal cartilage to the sternum). Pulmonary artery valve is listened here.
4.The fourth auscultation point - on the sternum near the xiphoid process. The fourth auscultation point is somewhat lower than the projection of the tricuspid valve and is located near the site of processus xifoideusattachment to the sternum - at the lower part of the sternum to the right. 4 point is a tricuspid valve auscultation point.
5.Fifth (extra) auscultation point - 2/3 of the stethoscope should be put in the left 3rd intercostal space close to the sternum, and 1/3 - on the sternum. This is so-called Botkin-Erb's point1. Aortic valve is listened here.
Currently, auscultation of the heart only in the 5 fixed auscultation points is considered insufficient. According to M.M. Mirrahimov et al. (1981), «the selection of these points is useful when teaching students at the beginning, because it «ties» to each other regions of valve localization and the most frequent place of its auscultation on the anterior chest wall. But for the physician the heart auscultation in the standard points is insufficient due to the fact that the murmurs usually (with rare exceptions) do not cover the point, but the region. At this auscultation point the murmur can only be heard or conducted, and its maximum can be placed between the points. Meanwhile, in the majority of cases, it is possible to assess the murmur properly only in the region of its maximum sounding. This implies that one needs to listen to the entire area of the heart».
30
