
Cardiology / English / Internal_diseases_propedeutics._Part_II._Diagnostics_of_cardiovascular_diseases
.pdf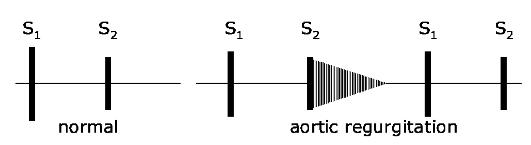
in significant cusps destruc tion it may not to be heard. In syphi litic and atherosclerotic lesion of aorta S2 may be cl ear enough.
The typical auscultativ e sign of aortic incompetence is diast olic murmur, listened at the aorta and at the BotkinErb's point, which is best heard by sitting the patient upright, leaning forward in full ex piration. It usually is soft, blowing protodiastolic murmur, weakening to the end of diastole as blood pressure decreasing i n aorta and blood flow slowing (Application Fig.4, Fig. 24).
Fig. 24. Diastolic mur mur in aortic regurgitation is located at the 2nd - 4th left interspaces and radiates to the apex, to the right sternal border. The murmur is highpitched, blowing in quality, may be mistaken for breath sounds. I t is heard best with the patient sitting, leaning forwa rd, with breath held in exhalation.
In aortic incompetence at the apex murmurs of functional origin may be also heard. So, in large left ventricular dilatation relative mitral incompeten ce occurs and systolic murmur at the apex appears. Rarely diastolic (presystolic) murmur - Flint's murmur appears due to mitral valve cusps raising by a strong stream of blo od regurgitating during diastole from aorta to left ventricle. It results in difficult blood flow from LA to LV during active atrium systo le. Sometimes in this valve disease two sounds (Traube's doubling sound) and the Vin ogradov-Duroziez‘s doubling murmur heard over the femoral artery are revealed. They are explained by vibration of arterial wal l on systole and diastole during pulse wave passing.
Aortic stenosis: on the heart auscultation at the apex diminished S1, connected with left ventricle overfilling and lengthening of its systole, is listen ed. At the aorta S2 is diminished, in case of adh ered valve cusps immobility it may not be heard. Rough systolic murmur, connected with blood flow across the narrow orifice, at the aorta is
41
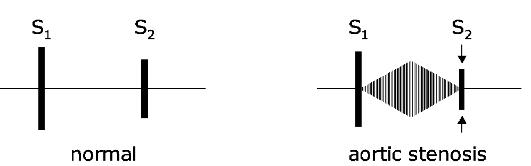
characteristic. It radiates along blood flow direction to the carotids , and sometimes it may be heard at the interscapular area (Application Fig.7, Fig. 25).
Fig. 25. Midsystolic murmur in aortic stenosis is heard in the 2nd right intercostal space, radiates often to the n eck and down the left sternal border, even to the apex. Heard best with the patient sitting a nd leaning forward. A2 decreases as th e stenosis worsens.
Although examination of the alimentary and respiratory sys tems forms part of the complete clinical as sessme nt, palpation of the abdomen for hepat omegaly, firm pressure over the sacrum for dependent oedema, and auscultation over the lung bases are important for the clinical evaluation of the cardiovascular system.
Functional murmurs all the functional murmurs are conditionally divided into three groups:
1.dynamic murmurs, based on significant blood flow velocity increase in absence of any organic cardiac diseases ( for example, dynamic murmurs in thyrotoxicosis, cardiac neurosis, febrile conditions).
2.anemic murmurs, caused by decrease of blood viscosity and certain blood flow acceleration in patients with anemias of different genesis;
3.murmurs of relative valv ular incompetence or relative narrowi ng of valvular openings caused by various valvula r function lesions, including patient s with organic cardiac diseases.
Extracardiac murmur s
Pleuropericardial (ple ural extrapericardial) rub occurs w hen the inflammation process captures part of the pleura, close to the heart, and simu ltaneously the external pericardial layer. This murmur is heard not only in the resp iratory phases, but is synchronic with the heartbeats. To distinguish it from the true pe ricardial rub caused by
42
friction of the inflamed pericardium layers, their attitude to breathing serves. While in true pericarditis friction rub is best heard at breath holding, pleuropericardial rub is best heard at inhalation, sometimes at exhalation, because under these conditions, larger pleural layers surfaces contact with each other (Pletnev D.D., 1928).
Cardiopulmonary murmurs occur in adjacent to the heart parts of the lungs, expanding during systole due to the reduced heart volume. Air penetrating into these parts of the lungs, gives murmur, vesicular in nature («vesicular breath-ing») and systolic in time [«vesicular breathing» with the heart rate] (Chernorutsky M.V., 1954).
Auscultation of vessels
Vinogradov-Durozier's murmur (Vinogradov N.A., 1831-1885, Russian clinician; Durozier Paul Louis, 1826-1897, French physician) is a combination of systolic and diastolic murmurs detected by pressing a stethoscope on the projection area of the femoral artery; it occurs in aortic insufficiency due to reciprocating blood flow through the major arteries.
Murmurs are not heard in a healthy person in ordinary peripheral arteries auscultation. If stethoscope slightly presses on the carotid, subclavian, brachial or femoral arteries, murmur of stenotic origin may appear during their auscultation.
In aortic insufficiency, during auscultation of the femoral artery with a little pressure of stethoscope on it, two murmurs (Vinogradov-Durozier's double murmur) are heard instead of one that can be heard in the normal condition. «First» murmur is caused by artificial narrowing of the arteries, «second» - by the reverse blood flow.
Traube's dual sound (Traube L., 1818-1876, German physician) - auscul-tatory phenomenon: double sound which is heard over the femoral artery. The appearance of Traube's dual sound is a sign of the aortic valve insufficiency.
Two sounds can be heard on auscultation of the carotid and subclavian arteries, one sound is heard on auscultation of the femoral artery, no sound is heard over the brachial artery normally in a healthy person. First sound is quiet, connected with the sudden strain of the arterial wall during admission of blood wave. Second sound (diastolic) is the usual
43
II heart sound, heard on auscultation of the heart and caused by slamming of the aortic valve, but held by the blood flow to the carotid and subclavian arteries.
In case of aortic insufficiency over femoral artery instead of normal one audible sound there two loud sounds are identified, similar to the sound of gun shots (Traube's dual sound).The first sound is caused by the sudden tension of the arterial wall during admission of blood wave, and the second is due to its sudden relaxation because of sharp decrease in blood supply of the femoral artery caused by blood regurgitation into the left ventricle. One should remember, that in aortic insufficiency classic II heart sound disappears and heard over the femoral artery sound is not the II heart sound, held here, but an independent sound, emerging in the femoral artery itself.
It should be kept in mind that both Traube's dual sound, and Vinogradov-Duroziez's dual murmur can be observed not only in aortic insufficiency, but also in infectious diseases, Graves' disease and severe anemia, apparently due to the lowering of the arterial walls tonus (Gubergrits A.J., 1956).
Techniques for improving the auscultation
Sirotinin-Kukoverov's sign (Sirotinin V.N, 1855-1936, Russian therapist; Kukoverov N.G. - assistant doctor of Sirotinin clinic) is appearance (or enhancement in its presence) of systolic murmur at the point of aortic valve auscultation with the patient's raised hands (e.g., at the location of the hands on the hind head). This is the sign of atherosclerotic lesion of ascending thoracic aorta.
Rivero Carvallo sign (Rivero Carvallo J.M.R.) - pathophysiological phenomenon: enhancement of auscultation phenomena (mainly systolic murmur), related to the activities of the right heart, with breath holding during or at the height of a deep inhalation, helps to identify defects of the tricuspid valve. In some guidelines there is error in naming the symptom, it is written incorrectly «Rivero-Carvallo sign». J.M.R. Carvallo was Mexican doctor working at the National Heart Institute in Mexico City. This sign he described in 1946. According to S. Mangione (2004), «medical folklore attributed to him partner (Dr. Rivero), so the sign is often named Rivero-Carvallo sign. In fact, Rivero is one of Carvallo's names.
44

Palpation of the radial pulse
Feeling the right radial pulse has been by tradition the first invasion of a patient's person by his physician. This first contact should therefore transmit warmth, confidence and reassurance. If your hands are cold you should rub them vigorously to warm them. Hold the patient's hand firmly in one hand and feel the pulse with the fingers of the other hand. The first important issue to settle is whether the pulse is present and palpable or absent due to any local or generalized vascular disease.
Next, you need to answer questions about four features of the pulse (Table 5).
The first two of these are comparatively easy and can be answered by counting the pulse rate at least 30 seconds. This is long enough to form an initial opinion about the rhythm, whether regular or irregular due to ectopic beats or completely chaotic as in atrial fibrillation.
|
Table 5. |
|
|
Examination of the pulse |
|
|
|
|
Feature |
Interpretation |
|
|
|
|
Rate |
Resting, 60-80 beats per minute-1 Tachycardia, 90 or more beats per minute- |
|
|
1 Bradycardia, 60 or less beats per minute-1 |
|
|
|
|
Rhythm |
Regular |
|
|
Irregular - ectopic beats or atrial fibrillation Chaotic - atrial fibrillation |
|
|
|
|
Volume |
Normal |
|
|
Large - hypertension, diastolic overload Small - low output states |
|
|
|
|
Character |
Normal |
|
|
Collapsing - aortic incompetence Slow rising - aortic stenosis Bisferiens - |
|
|
aortic stenosis and incompetence |
|
|
|
|
Volume. This is the upstroke of the pulse wave as appreciated by the pulps of the examining fingers, and reflects the pulse pressure or the difference between the systolic and diastolic pressures. It gives some idea about the diastolic burden, output and contractility of the left ventricle. A great deal of experience is required to decide whether
45
a particular pulse volume is normal, small or large. It is advisable to feel your own pulse simultaneously and develop a habit of making a decision about the volume of the patient's pulse.
A large volume pulse suggests hypertension or diastolic overload (e.g. aortic or mitral incompetence, patent ductus arteriosus, severe anaemia, fever, thyro-toxicosis, etc.). A small volume pulse is usually associated with low output states such as mitral or aortic stenosis and any condition with blood pressure.
Character. The character of a pulse is the entire waveform as felt by the examining fingers. This is better appreciated by feeling the brachial pulse with the thumb; the arm of the patient should be kept straight and your thumb should gently press the artery against the bone until the entire upstroke is absorbed into the pulp of the thumb. This method should be practiced as it can be quite useful in detecting the slow rising.pulse of aortic stenosis, and bisferiens pulse of mixed aortic valve disease and severe aortic incompetence.
An exaggerated upstroke, or a bounding pulse, may be felt in patients with elevated stroke output (mitral regurgitation, ventricular septal defect, high fever), sympathetic overactivity (thyrotoxicosis), and in patients with rigid, sclerotic aorta. A slow upstroke (pulsus tardus) is felt in cases of left ventricular outflow obstruction, and may be associated with a thrill felt over the carotids (carotid shudder).
A large volume pulse may have a collapsing character which can be detected by lifting the arm of the patient, with the four fingers of your one hand placed firmly on his wrist, and the palm of your other handplaced over the brachial artery. A collapsing (Corrigan's) pulse will impart a flick across your fingers on both hands, and suggests a large upstroke (due to diastolic overload) and quick downstroke due to a runoff either at the aorta valve (aortic incompetence) or from the aorta into the left pulmonary artery (patent ductus arteriosus). It is the change of character on lifting the arm and not simply its easy palpability that is specific to a collapsing pulse. Corrigan's pulse can be seen and felt in the neck over the carotid artery.
Pulsus bisferiens with two peaks (the tidal and percussion waves) can be felt over the carotids, but it is best felt over the peripheral pulses such as the radials, brachials and
46
femoralis in some patients with combined aortic valve disease and severe aortic regurgitation.
Pulsus alternans (equally spaced and alternating large and small beats) is a sign of left ventricular depression. It must be distinguished from pulsus bigeminus in which a premature ventricular beat occurs after every normal beat. This ectopic beat feels weak at the wrist and is easily confused with the weak beat of pulsus alternans, but in the latter the rhythm is regular whereas in the former the weaker beat always follows the short interval.
Pulsus paradoxus - the pulse volume normally decreases during inspiration, but this decrease is exaggerated when there is a reduced left ventricular stroke volume (cardiac tamponade, constrictive pericarditis), and transmission of negative intrathoracic pressure to the aorta (severe bronchial asthma, emphysema). Thus, the application of the term pulsus paradoxus, to a greater than normal decline in systolic arterial pressure (10 mm Hg or more) during inspiration, is wrong but it has the advantage of common and long usage. Although both thepulsus alternans and paradoxus can be appreciated at the radial pulse, they are easily recognized on sphygmomanometry.
Tension. An estimation of tension (systolic pressure within the artery) can be obtained by compressing the brachial artery gradually until the radial pulse disappears. The force required to obliterate the brachial arterial pulse can be given by a figure which should approximate to the measured systolic pressure. The difference between the two gets smaller with experience.
Other pulses must be examined now if the cardiovascular system alone is being examined, but the task can be deferred till the examination of the nervous system when it is convenient to feel for the pulses as well as test the tendon reflexes in the legs. You should decide upon a routine and stick to it.
The other radial artery should be palpated simultaneously to compare the volume and tension in both radials. The femoral artery should be located in the inguinal region and felt to both sides, and if its volume is suspected to be low then it should be felt simultaneously with the radial to look for the radiofemoral delay. In obstructive lesions
47
of the aorta (coarctation of the aorta; atheroma, dissection, compression by a tumour) the femoral pulse, which is normally ahead of the radial, is delayed and reduced in volume.
Of the other pulses the popliteal can be difficult to feel, particularly when it is important (namely in peripheral vascular insufficiency) to decide whether it is palpable and of normal volume. With the knee joint semiflexed the popliteal fossa should be palpated with both hands. In difficult cases the palpable pulse may be felt in the prone position. The posterior tibial and the dorsalis pedis pulses are comparatively easier to feel in their appropriate places.
The carotid pulse because of its proximity to the heart can be very informative and, as an extension of the outflow tract, reflects faithfully the events at and below the aortic valve. It can be felt inside the sterno-mastoid muscle with the thumb. The anacrotic pulse can be appreciated by the pulp and the collapsing pulse can be felt as well by following movements of the thumb (Corrigan's sign).
The waveform of the carotid pulse may be difficult to appreciate in some patients with a large adipose or muscular bulk. For this reason it is important to cultivate the habit of palpating the brachial pulse.
Popov-Saveliev's sign (Saveliev N.A., Russian therapist; Popov V.O. - Russian physician) - a weakening of the pulse wave in the left radial artery, especially when lying on the left side (a sign of stenosis of the left atrioventricular opening).
Blood pressure
This important task should be undertaken towards the end of the examination, or at least after 15 minutes rest, when the patient is more likely to be relaxed and accustomed to the environment and examination. Blood pressure is measured with a stethoscope and a sphygmomanometer. The width of the cuff should be about 40% of the circumference of the limb used for determining the blood pressure. The standard size, a 14 cm wide cuff, is used for adult with an arm of average size. The cuff width should be 7 cm for young children, and 22 cm for obese and heavily built subjects. The mercury manometer should be kept at a level corresponding to the heart of the patient to rule out the influence of gravity.
48
The cuff should be wrapped firmly around the upper arm and air pumped while the brachial or radial pulse is felt. As the pressure in the cuff exceeds the systolic pressure within the brachial artery the pulse becomes impalpable. This pressure should be noted and the cuff deflated.
Next the bell of the stethoscope should be placed lightly over the brachial artery in the antecubital fossa and the above procedure repeated. After the pressure has reached the previously noted level, the cuff should be deflated gradually. The passage of blood past the decreasing obstruction creates a series of sounds (named after Korotkoff, a naval surgeon who first described them) which are audible through the stethoscope. The first loud sound (phase I) approximates to systolic pressure. As the pressure in the cuff is further lowered, the sounds first become softer (phase II), then
louder (phase III), as the volume of blood flow through the constricted artery increases. The sounds become muffled (phase IV) when the arterial caliber increases and the arterial diastolic pressure approaches. The point of disappearance of the Korotkoff sounds (phase V) is used to define diastolic pressure. It is a good practice to record the pressure both at phase IV and phase V. In aortic regurgitation and pregnancy the disappearance point may be very low when phase IV is much closer to the diastolic pressure.
The systolic pressure should always be measured first by palpation, since in some patients with very high blood pressure the Korotkoff sounds may disappear then reappear again as the cuff pressure is lowered. This phenomena is called the auscultatory silent gap.
The blood pressure should be measured in both arms if the pulse is weaker on one side, or if you suspect vertebrobasilar insufficiency with subclavian steal. In patients with orthostatic hypotension, the measurements should be taken both in the supine and the erect positions. In patients suspected of having coarctation or atheromatous disease of the aorta, blood pressure should be measured in the arm and in the thigh where the arterial systolic pressure, which is usually about 20 mm Hg higher than in the arm, may be lower. The cuff should be applied to the thigh in the prone position, and auscultation should be carried out over the popliteal fossa.
49
In pulsus alternans, the systolic pressure may vary by more than 10 mm Hg in alternate beats. This discrepancy can be recognized by alteration in the intensity of the Korotkoff sounds. In pulsus paradoxus, the peak systolic pressure during expiration may be higher by 10 mm Hg or more than the corresponding pressure during the entire cycle of respiration.
Hill's sign (Hill L., 1866-1952, English physiologist, Nobel Prize winner in Physiology). Hill's sign is an increase of existing and normal difference of systolic blood pressure on the arms and legs.
The normal systolic blood pressure on the legs (as measured by Korotkoff method) is higher than on the arms, but not more than 10-15 mm Hg. This is due to feebly marked augmentation (amplification) phenomenon, i.e. summing of the amplitudes of the incoming and reflected waves (forming the so-called «standing wave») in the lower limbs due to greater distance from the heart to the lower extremities in comparison with the upper limbs. It should be noted that during direct intravascular measurement, blood pressure on the legs is not higher than on the arms.
Hill's sign occurs in hyperkinetic conditions due to even more enhancement (further augmentation) of blood wave at high stroke volume, when the value of «standing waves» (the «tsunami»1 effect) can be significantly increased. This occurs in case of severe aortic insufficiency, hyperthyroidism and other hyperkinetic states.
CIRCULATORY FAILURE
Circulatory failure is an extremely common problem with an incidence of 2% at age 50 years, rising to 10% at age 80 years. There is still a high mortality: 10—30% per year. Circulatory failure occurs when an adequate blood flow to the tissues cannot be maintained. This maybe caused by inadequate cardiac output (heart failure) or by a markedly reduced intravascular volume, for example after major haemorrhage, acute dehydration or in septicaemic shock (vascular failure).
Heart failure (congestive heart failure): Symptomatic myocardial dysfunction resulting in a characteristic pattern of hemodynamic, renal, and neurohormonal responses.
50
