
Учебники / Head_and_Neck_Cancer_Imaging
.pdf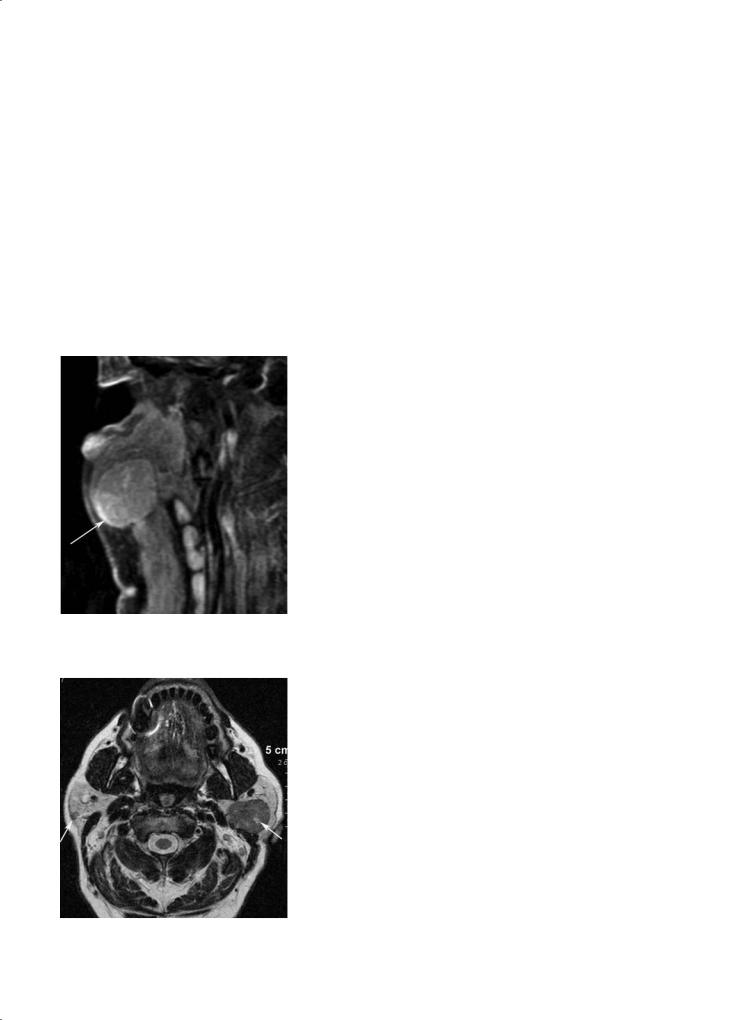
Parotid Gland and Other Salivary Gland Tumors |
227 |
a 
 b
b
|
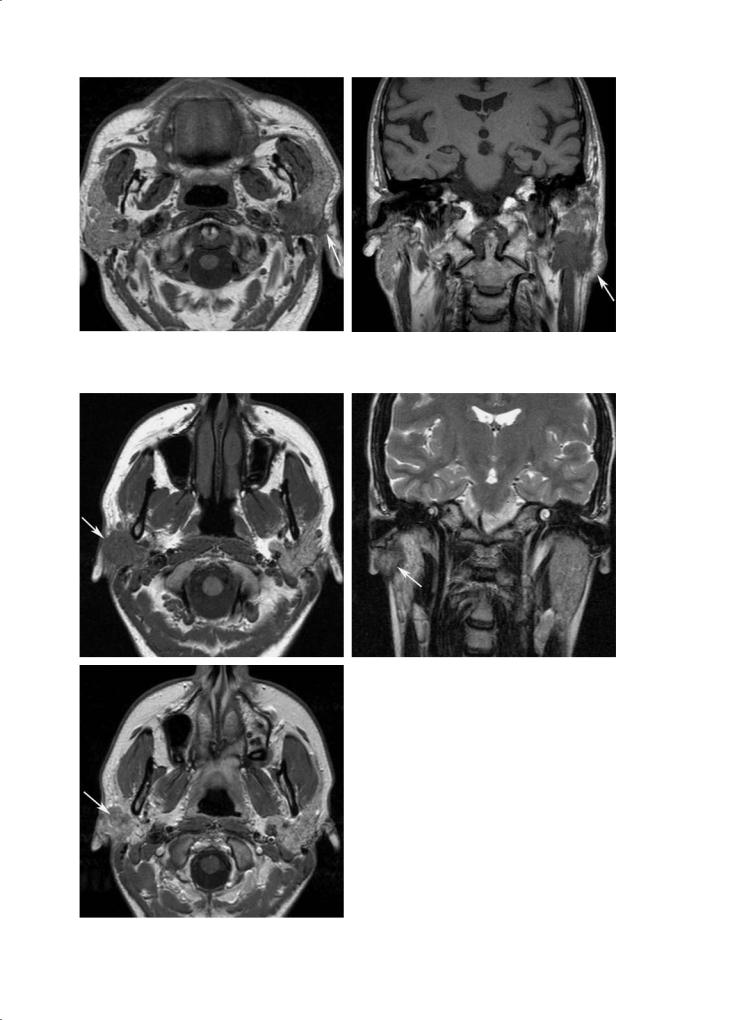
Fig. 12.12a–c. Typical Warthin’s tumor in the superficial lobe of the right |
|
parotid gland showing a low T1-weighted signal intensity with small high |
|
signal intensity areas (arrow, a), a low T2-weighted signal intensity (b), |
|
and a mild enhancement most pronounced in the periphery of the mass |
c |
(arrow, c) |
Fig. 12.13. Typical Warthin’s tumor involving both the superficial and deep lobe of the left parotid gland. The tumor shows a low T1-weighted signal intensity (arrow) with small spontaneously hyperintense areas (due to hemorrhagic changes and cholesterol crystals). Note the small contralateral Warthin’s tumor (arrow)

228 |
F. Dubrulle and R. Souillard |
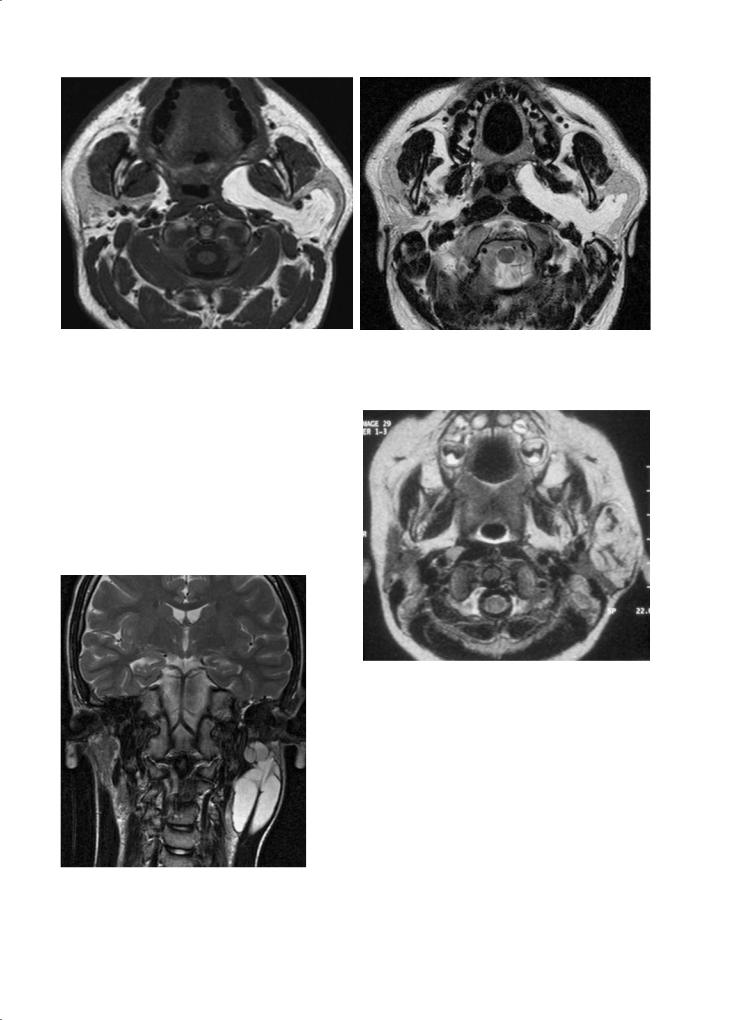
a 
 b
b
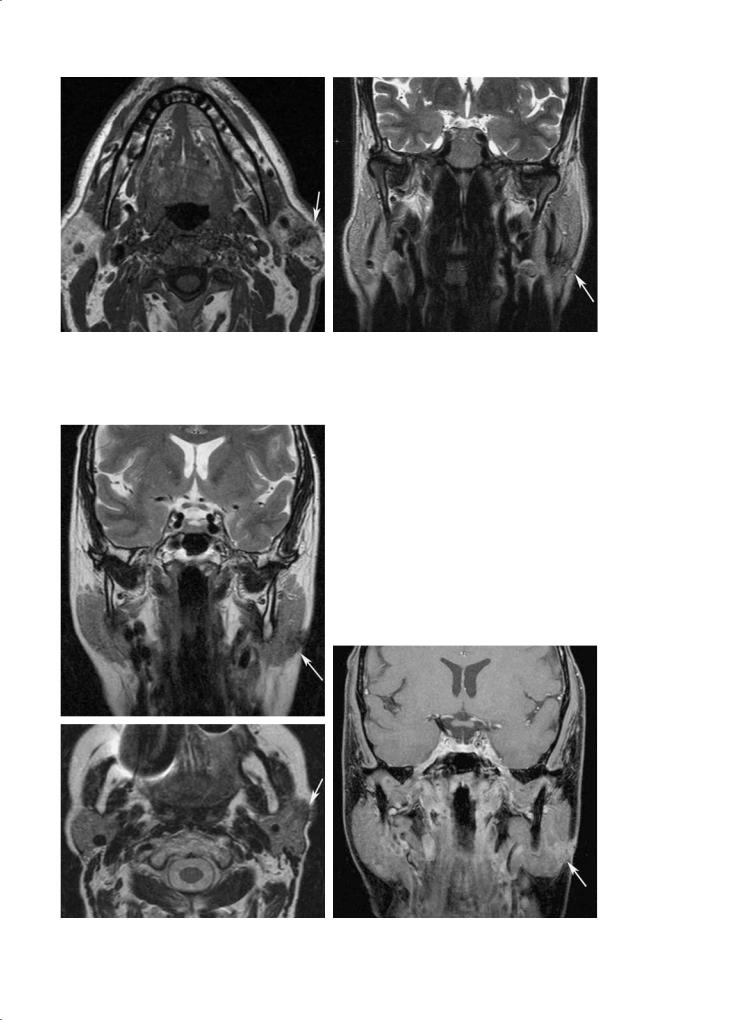
Fig. 12.14a,b. Typical bilateral Warthin’s tumor with a low T1-weighted (a) and a low T2-weighted signal intensity. Areas of cystic changes show a high T2-weighted signal intensity within the left lesion (b)
12.4.2.4
Di erential Diagnosis
x Atypical pleomorphic adenoma
x Benign lymphoepithelial lesions in HIV-positive patients
x Malignant tumor with few malignant characteristics on imaging
12.4.3
Other Benign Tumors
12.4.3.1 Lipoma
It represents 1% of all parotid gland tumors. CT and MR findings are characteristic: well-circumscribed lesion with negative HU values on CT, showing high T1-weighted and high T2-weighted signal intensities, without enhancement on contrast-enhanced T1-weighted images. The high T1-weighted signal intensity disappears on fat-suppressed sequences (Fig. 12.15).
12.4.3.2 Neurogenic Tumor
Imaging findings are non-specific but show characteristics of a benign tumor, centred on the facial nerve plane, with low T1-weighted, high T2-weighted signal intensities and homogeneous enhancement. When large in size, cystic changes may occur, making the diagnosis on imaging more difficult.
12.4.4
Congenital Tumors
12.4.4.1 Lymphangioma
Lymphangioma presents as lobulated, multiloculated, cystic mass with septations. Some of the cystic areas can show spontaneous high signal intensity. Sometimes fluid–fluid levels are seen. Cystic foci do not enhance. Cystic lymphangioma often occurs in the lower portion of the parotid gland (Fig. 12.16).
Mixed vascular malformations exist, such as the cavernous lymphangioma, composed of (enhancing) solid areas and dilated lymphatic spaces.
12.4.4.2
Infantile Hemangioma
A schwannoma of the intraparotid portion of the facial nerve may occur but remains exceptional in this localization. It can be solitary or multiple.
This is the most frequent tumor of the parotid space in infants and young children. This tumor shows a three-phase evolution: rapid growth until the age of
Parotid Gland and Other Salivary Gland Tumors |
229 |
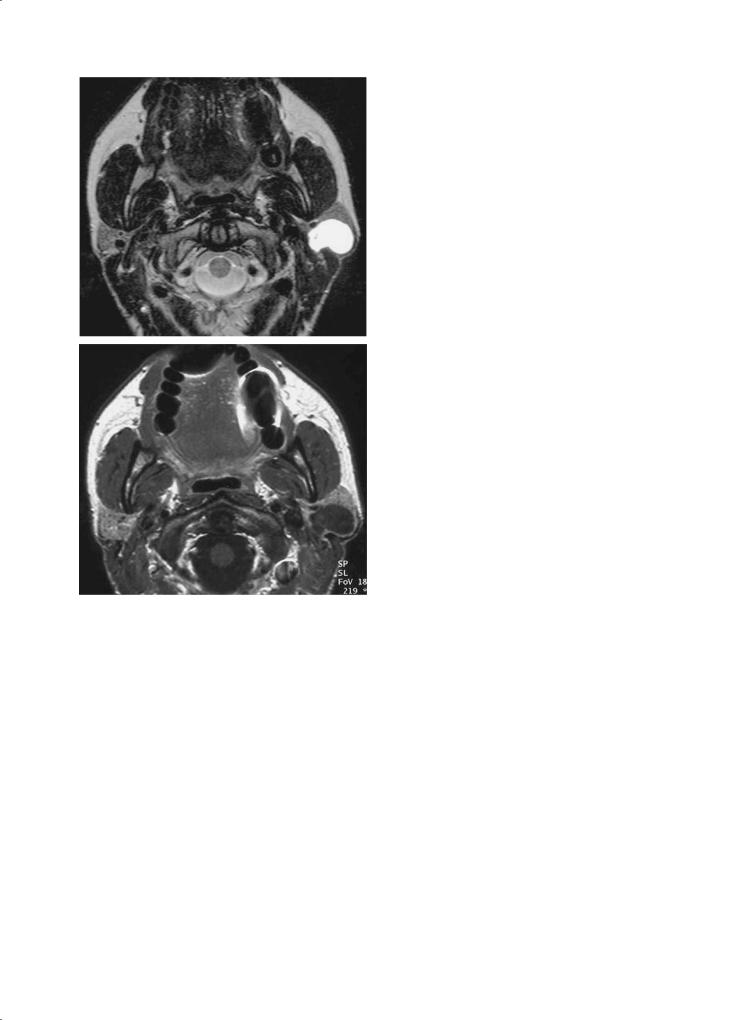
a |
b |
Fig. 12.15a,b. Lipoma of the left parotid gland extending to the deep lobe and the anterior parapharyngeal space, showing a spontaneous high T1-weighted signal intensity (a) and a high T2-weighted signal intensity (b)
about 10 months, then stabilization and finally regression with sometimes an incomplete involution with residual calcifications.
Imaging findings are a large solid mass which shows intermediate T1-weighted, high T2-weighted signal intensities, and intense and fast enhancement with multiple enlarged vascular signal voids (Fig. 12.17).
Fig. 12.16. Cystic lymphangioma of the inferior pole of the left parotid gland. Typical aspect of a lobulated, septated, cystic mass showing a high T2-weighted signal intensity
Fig. 12.17. Infantile capillary hemangioma: a large solid mass of the left parotid space showing intense enhancement and containing multiple enlarged vascular signal voids
12.4.5
Cystic Tumors
12.4.5.1
Solitary Cystic Lesion
A solitary cystic lesion of the parotid gland is rare (Som et al. 1995). The cystic nature of the lesion has to be confirmed on imaging using specific sequences. Actually, most parotid gland tumors have a high T2-weighted
230 |
F. Dubrulle and R. Souillard |
a
b
Fig. 12.18a,b. Solitary simple cystic lesion of the left parotid gland with a high T2-weighted (a) and a low T1-weighted signal intensity without any contrast enhancement (b)
signal intensity, so this finding does not systematically correspond to a cystic lesion.A cystic formation shows a low T1-weighted signal intensity without any enhancement on contrast-enhanced T1-weighted sequence. It has a high T2-weighted signal intensity including T2weighted sequence with long echo time (Fig. 12.18). Cystic lesion appears hypointense on diffusion-weighted sequence at b factor of 800 or 1000 s/mm².
A cystic lesion of the parotid gland is suggestive of first branchial cleft abnormality, and a fistulous connection in or around the external auditory canal must be looked for (Van der Goten et al. 1997). If the cyst appears to be unilocular and non-commu- nicating, the differential diagnosis is between a non-
communicating branchial cleft cyst and a simple cyst of the parotid gland.
12.4.5.2 Dermoid Cysts
Dermoid cysts may occur in the parotid space. Their heterogeneous structure (fat, bone, skin adnexa) is highly suggestive of this diagnosis.
12.4.5.3 Epidermoid Cysts
Rarely epidermoid cysts occur in the parotid gland. They show typical signal intensities on MRI: a low T1weighted, a high T2-weighted signal intensity and no enhancement on contrast-enhanced T1-weighted images. A diffusion-weighted sequence is very helpful because epidermoid cysts show high signal intensity at b factor of 800 or 1000 s/mm2, with a very small apparent diffusion coefficient (ADC) value (around 0.5u10-3 mm2/s).
These are slow-growing tumors and a single fol- low-up imaging study can be proposed.
12.4.5.4
Multiple Intraparotid Cystic Lesions
Multiple intraparotid cystic lesions must evoke the possibility of benign lymphoepithelial lesions, as may be seen in HIV positive patients (Holliday et al. 1998).
The etiology remains unknown; they are probably of inflammatory nature.
Imaging findings are multiple, bilateral cystic and solid masses, enlarging both parotid glands, associated with tonsillar hyperplasia and bilateral cervical adenopathy.
These lesions are well-circumscribed, sometimes heterogeneous, with low T1-weighted and high T2weighted signal intensities (Fig. 12.19).
The clinical profile should help in the diagnosis.
12.5
Malignant Parotid Tumors
Malignant tumors represent 15% of all parotid tumors. Clinical symptoms suggestive for malignancy are: facial nerve paralysis, pain, skin infiltration, a rapidly-enlarging lesion and cervical adenopathy. Prognosis depends on histologic grade.
Parotid Gland and Other Salivary Gland Tumors |
231 |
Fig. 12.19. Multiple bilateral cystic lesions in a HIV-positive patient, corresponding to benign lymphoepithelial lesions
associated to a systemic lymphoma with cervical lymphadenopathy and other lymphoma localizations. Patients suffering Sjögren’s syndrome have an increased risk of developing parotid lymphoma.
x Intraparotid metastases. The vast majority of parotid metastases of known primary tumors originate from the skin in the head and neck region.
x Liposarcoma and rhabdomyosarcoma. These are rare parotid neoplasms.
12.5.2
Imaging Findings
12.5.2.1 Parotid Cancer
12.5.1
Histologic Classification
x Adenocarcinoma, squamous cell carcinoma and undifferentiated carcinoma. These malignant tumors have a predilection for men and most cases occur over the age of 60 years. They are most frequently rapidly-growing tumors, presenting with facial nerve paralysis and early infiltration of the infratemporal fossa. The prognosis of these cancers is very bad.
x Adenoid cystic carcinoma. This malignant tumor occurs more commonly in the submandibular gland and the minor salivary glands. Adenoid cystic carcinoma is a slow-growing, widely infiltrative tumor with a tendency for perineural spread along the facial nerve and trigeminal nerve (auriculotemporal nerve and mandibular nerve). A significant number of patients develop late intracranial recurrence due to perineural infiltration. Distant metastases develop in 40%– 50%.
x Mucoepidermoid carcinoma. This has a female predominance and is most frequently seen in the 40to 60-year age group. Prognosis depends on the histologic grade. Low-grade mucoepidermoid carcinoma may have a clinical and radiological presentation of a benign tumor. High grade tumors have a high risk of local recurrence and distant metastases.
x Non-Hodgkin lymphoma. This develops from intraparotid lymph nodes and is frequently
The aim of imaging is to identify the malignant features of a tumor in order to initiate the best therapy as soon as possible. Subtle signs of malignancy (Figs. 12.20–12.23) (Freling et al. 1992) that have to be scrutinized include the following:
x Poorly-defined margins, indicating an invasive mass, including infiltration of the adjacent fat tissue, which can be an early and only sign suggesting malignancy, best depicted on precontrast T1-weighted images.
x Cervical lymphadenopathy.
x Extension to the adjacent deep facial spaces (Fig. 12.24) such as the masticator and parapharyngeal space.
x Perineural spread along the facial nerve or trigeminal nerve, better depicted on contrast-enhanced images with fat saturation, is typically seen in adenoid cystic carcinoma (Fig. 12.25) (Harnsberger 2004; Som and Brandwein 1996).
x Low T2-weighted signal intensity may indicate malignancy (Som and Biller 1989), but may also be seen in some benign tumors.
Histologic diagnosis is not possible on imaging.
If a malignant tumor is suspected on imaging, a fine needle aspiration may be performed. This allows differential diagnosis with a benign tumor in 85%– 90% of cases (Zbaren et al. 2001).
The typical treatment of these malignant tumors is wide surgical resection, lymph node dissection and radiation therapy.
232 |
F. Dubrulle and R. Souillard |
a |
b |
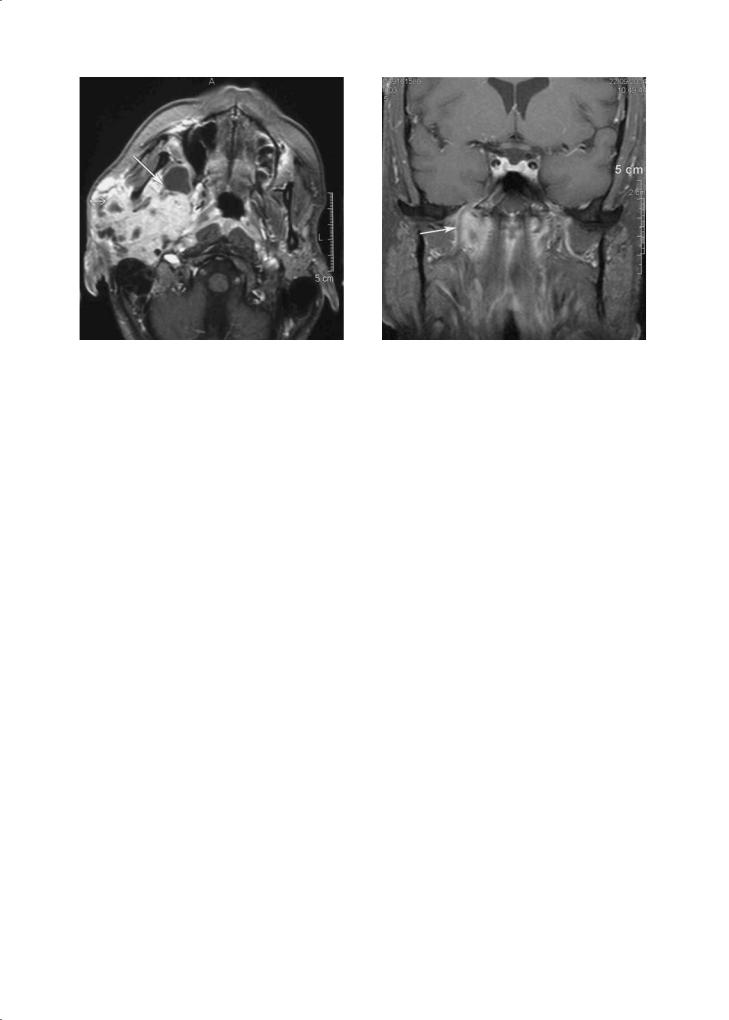
Fig. 12.20a,b. Malignant tumor of the left parotid gland, with ill-defined margins, infiltrating the adjacent subcutaneous fat tissue (arrow), well appreciated on pre-contrast T1-weighted images (a, b). Adenocarcinoma
a |
b |
|
Fig. 12.21a–c. Malignant tumor of the right parotid gland, with |
|
poorly-defined margins and infiltrating the subcutaneous adjacent |
|
fat tissue (arrow) showing a low T1-weighted signal intensity (a), |
|
a low T2-weighted signal intensity (arrow, b) and mild enhance- |
|
ment on the contrast-enhanced T1-weighted image (arrow, c). |
c |
Mucoepidermoid carcinoma |
Parotid Gland and Other Salivary Gland Tumors |
233 |
a |
b |
Fig. 12.22a,b. Small malignant tumor of the inferior pole of the left parotid gland (a). The ill-defined margins, low T2-weighted signal intensity (b), and infiltration of the adjacent fat tissue suggest malignancy (arrow). Mucoepidermoid carcinoma
Fig. 12.23a–c. Malignant tumor in the superficial lobe of the left parotid gland, with a low T2-weighted signal intensity (arrow, a). The infiltration of the adjacent fat tissue is well identified on pre-contrast T1-weighted image (arrow, b), as well as on the con- trast-enhanced T1-weighted images with fat saturation (arrow, c). Adenocarcinoma
a
b |
c |
234
Fig. 12.24. Adenoid cystic carcinoma of the right parotid gland extending to the parapharyngeal space and the infratemporal fossa (arrow)
F. Dubrulle and R. Souillard
Fig. 12.25. Adenoid cystic carcinoma of the deep lobe of the right parotid gland, showing perineural spread along the mandibular branch of the trigeminal nerve (arrow) towards the foramen ovale
12.5.2.2
Non-Hodgkin Lymphoma
Non-Hodgkin lymphoma often has more specific imaging features: multiple homogeneous nodal lesions with intermediate T1-weighted and T2-weighted signal intensities and moderate enhancement, rarely necrotic. Usually, there is also cervical lymphadenopathy showing the same signal intensity on all MR sequences (Fig. 12.26). The submandibular gland as well as the lacrimal glands may also be involved. Fine needle aspiration may confirm the diagnosis. However, the histologic diagnosis has to be confirmed by a larger tissue sample (such as an adenopathy). The treatment consists of chemotherapy, possibly associated with radiotherapy.
12.6
Di cult Cases
x Really difficult cases in imaging parotid gland tumors are rare and represent less than 10% of all cases. However, it can be impossible to differentiate an atypical parotid benign tumor, such as atypical pleomorphic adenoma, from a malignant tumor showing few typical malignant characteristics. Diffusion-weighted sequences are helpful in such situations. The lesion’s signal intensity at b factor of 1000 s/mm² and 0 s/mm², and the ADC
value need to be evaluated. Pleomorphic adenoma appears hypointense on diffusion-weighted sequence at b factor of 1000 s/mm², with an ADC value > 1.2 (Fig. 12.27). On the other hand, malignant tumors, including lymphoma, show a much lower ADC value, < 1.2. If the ADC value is > 1.2, suggestive of a pleomorphic adenoma, surgery of the lesion can be proposed. If the ADC value is < 1.2, fine needle aspiration can be done in order to first exclude malignancy. However, there is no consensus whether to perform fine needle aspiration or not. As already mentioned, this procedure allows differentiation of benign tumors from malignant tumors in 85%–90% of all cases (Zbaren et al. 2001; Lim et al. 2003). On the contrary, a specific histologic diagnosis for benign tumors is possible only in 40% of cases (Hamilton et al. 2003), except for cystadenolymphoma for which a diagnosis is possible in 74% of cases (Parwani and Ali 2003).
x It can also be very hard to differentiate an atypical pleomorphic adenoma showing a low T2-weighted signal intensity from a Warthin’s tumor. In such situations, MR diffusion-weighted imaging is very helpful: a pleomorphic adenoma appears hypointense on diffusion-weighted sequence at b factor of 1000 s/mm², with a ADC value > 1.2, whereas a Warthin’s tumor presents a high signal intensity at b factor of 1000 s/mm² with a low ADC value, lower than the one observed in case of malignant tumor (Ikeda et al. 2004).
Parotid Gland and Other Salivary Gland Tumors |
235 |
a |
b |
|
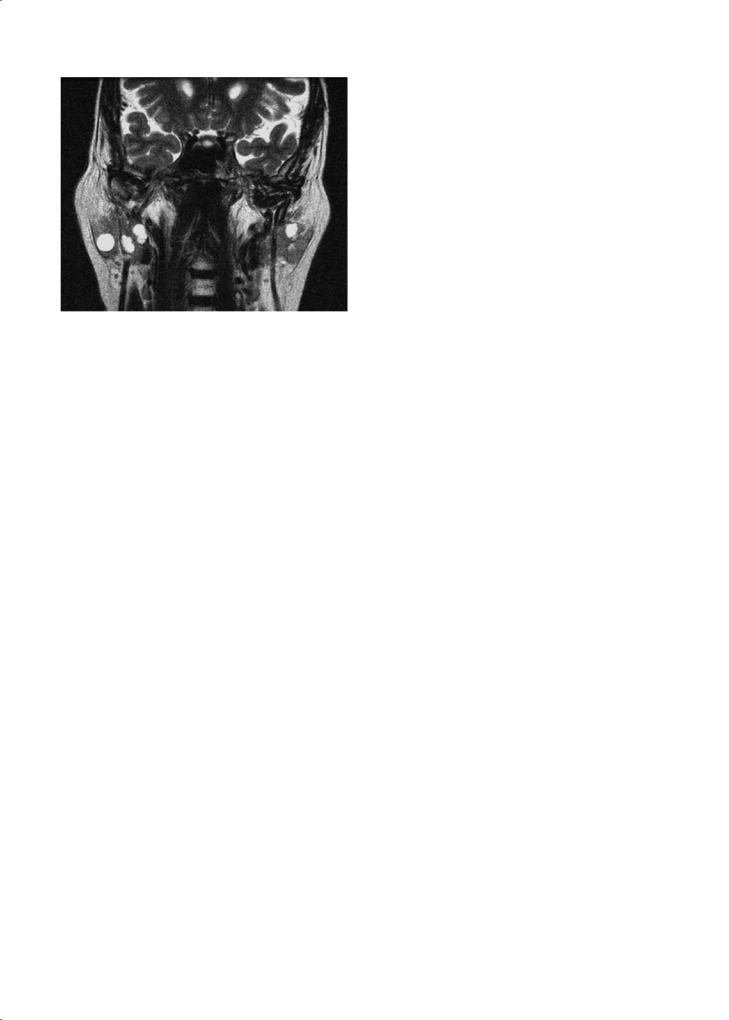
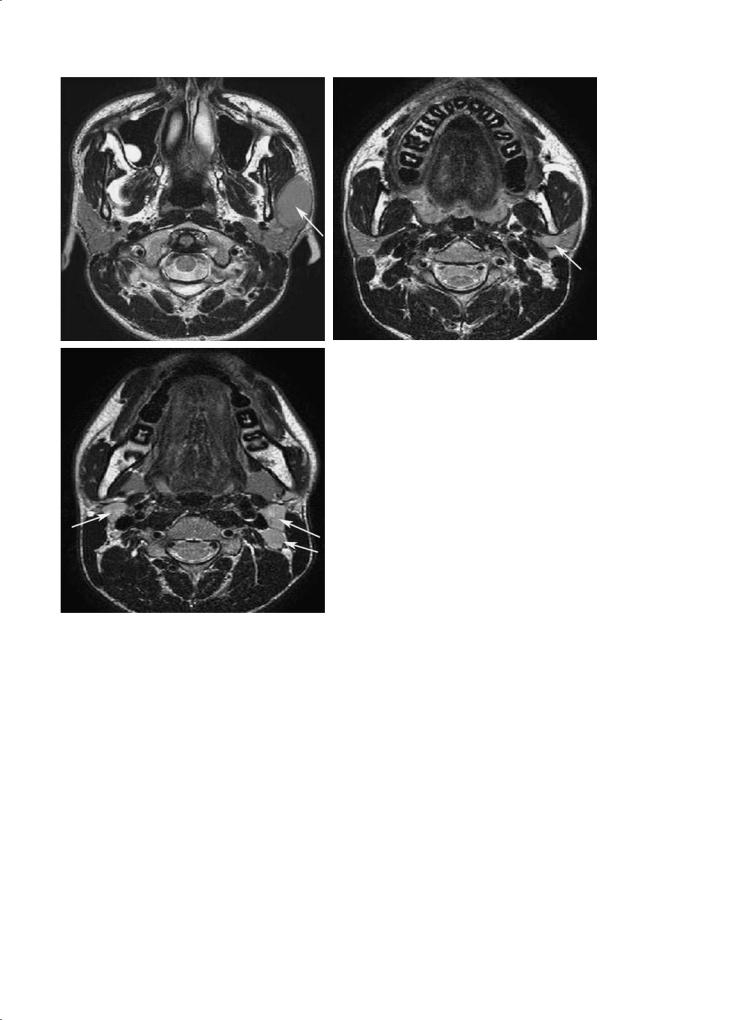
Fig. 12.26a–c. Multiple homogeneous nodular lesions of the left pa- |
|
rotid gland (a,b, arrow), associated with bilateral lymphadenopathy |
|
(c, arrows) showing the same intermediate signal as the parotid |
c |
lesions on all sequences, corresponding to lymphoma |
x Diffusion-weighted imaging also allows making the difference between a simple intraparotid cyst and an epidermoid cyst. An epidermoid cyst shows a high signal on diffusion-weighted images at b factor of 1000 s/mm² with a very small ADC value (around 0.5), favouring this diagnosis (see above).
12.7
Pseudotumors of the Parotid Gland
12.7.1
Sjögren’s Syndrome
This is a chronic systemic autoimmune disease that affects salivary and lacrimal glands.
The best diagnostic clue on imaging is bilateral enlargement of both parotid glands, usually asymmetric, with multiple small cystic and solid lesions; sometimes calcifications are present.
On MR imaging, a miliary pattern of small cysts throughout both parotids is diagnostic of Sjogren’s syndrome. The small collections show low T1-weighted, high T2-weighted signal intensities; the small cysts do not enhance, while the surrounding parenchyma shows mild enhancement. MR sialography suggest the diagnosis of Sjögren’s syndrome by showing multiple cystic lesions while the salivary ducts appear normal (Fig. 12.28) (Ohbayashi et al. 1998; Izumi et al. 1996).
The differential diagnosis includes benign lymphoepithelial cystic lesions in HIV positive
236 |
F. Dubrulle and R. Souillard |
a |
b |
|
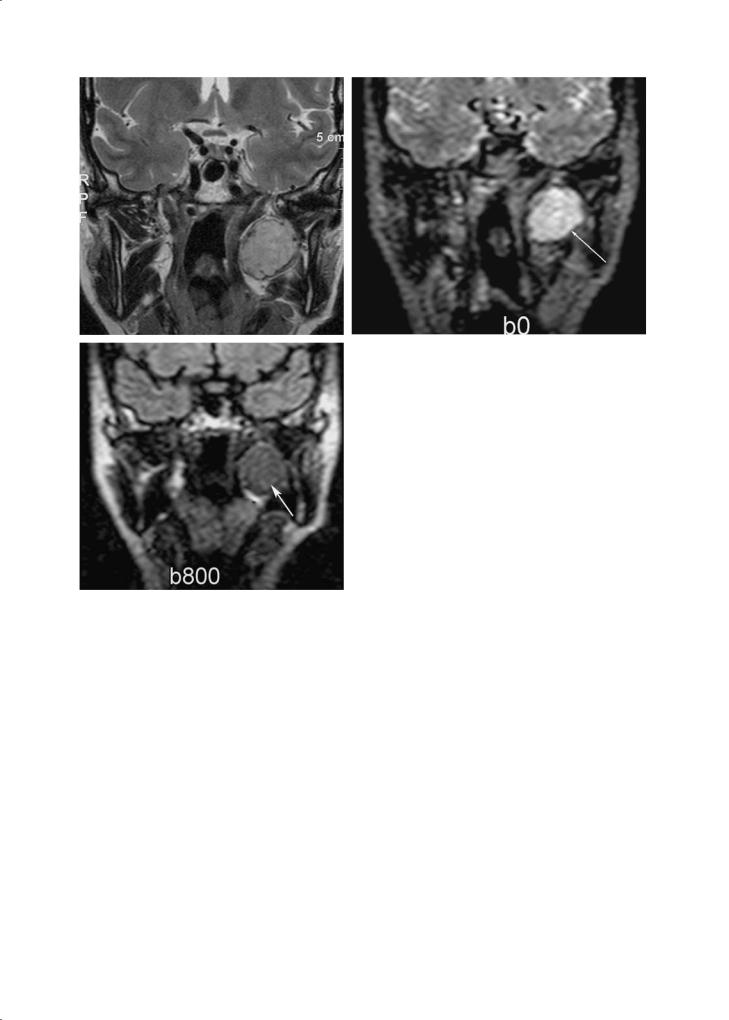
Fig. 12.27a–c. Pleomorphic adenoma of the deep lobe of the right |
|
parotid gland, appearing hyperintense on T2-weighted images (a), |
|
hyperintense on a diffusion-weighted image with b factor of 0 s/mm2 |
|
(arrow, b), and hypointense with b factor of 800 s/mm2 (arrow, c); |
c |
the ADC value is > 1.2 |
patients; cystic areas are usually larger in this pathology.
A solid tumoral mass, developing in the parotid gland in a patient with Sjögren’s syndrome, is suspect for lymphoma.
12.7.2 Sarcoidosis
Sarcoidosis is a systemic disease. The parotid glands are affected in 10%–30% of patients. It can present with solid and cystic lesions involving both parotid glands, often associated with cervical adenopathy.
Differential diagnosis must be made with nonHodgkin lymphoma, in which the imaging pattern commonly consists of bilateral, solid, nodal-appear-
ing intraparotid masses. The clinical presentation is usually suggestive of the diagnosis.
12.8
Tumors of the Other Salivary Glands
The paired submandibular and sublingual glands are referred to as major salivary glands, such as the parotid glands. The minor salivary glands are submucosal clusters of salivary tissue present in the oral cavity, particularly at the junction of hard palate and soft palate, pharynx, upper respiratory tract, as well as in the anterior parapharyngeal space. Whereas parotid tumors are frequently benign, other salivary glands tumors are often malignant.
