
SAOphthalmicAtlas&Guide
.pdf
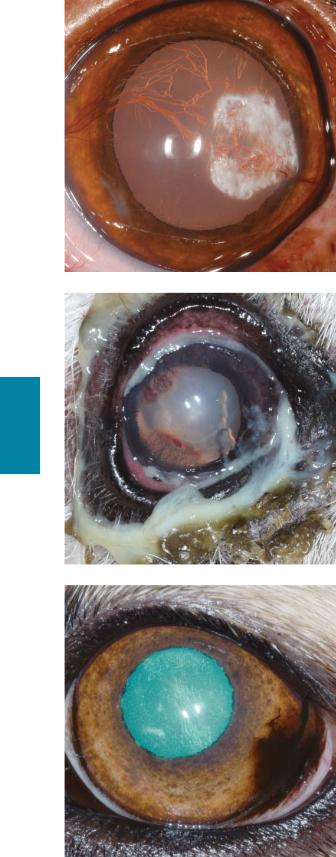
Figure 5.3 Right conjunctival hyperemia, superficial corneal vascularization, and corneal fibrosis (chronic, superficial, nonulcerative keratoconjunctivitis). Fluorescein has been applied but is not retained by the cornea. The extensive branching of the corneal vessels indicates their location in the superficial corneal stroma. The fibrosis affects the dorsal and lateral portions (approximately two-thirds) of the visible cornea. Because the fibrosis is causing mild corneal opacification, the pupillary margin immediately behind the fibrosis is less distinct than medially, where the cornea is unaffected. An eyelid mass is also present on the medial aspect of the lower eyelid. Superficial corneal vascularization is discussed on page 98, and keratitis is discussed on pages 100 to 101, and 111 to 112.
Figure 5.4 Chronic, stromal keratoconjunctivitis. Abnormalities include episcleral congestion, deep corneal vascularization, and diffuse corneal edema. The yellow tinge to the cornea is suggestive of white cell infiltrate in addition to edema. The dense grouping of the vessels and lack of branching are characteristic for vessels in the deep corneal stroma. Deep corneal vascularization and its significance is discussed on page 98.
Figure 5.5 Classic appearance of corneal edema. Note the bluish-white discoloration of the cornea. A regular pattern, often referred to as a “chicken wire” or “cobblestone” pattern, can be seen within the cornea and is also considered a characteristic finding of corneal edema. The white, amorphous shape adjacent to the limbus from 3 to
6 o’clock is a reflection and not a true corneal change. Corneal edema is discussed on page 99.
Chapter 5 Cornea 21
Chapter 5

22 Section I Atlas
Figure 5.6 Absence of fluorescein retention, superficial corneal vascularization, and corneal melanosis (chronic, superficial, nonulcerative keratitis) in a dog with chronic KCS. The STT was 13 mm/min with medical therapy. See pages 100 to 101, and 111 to 112 for discussion of keratitis and pages 101 to 103 for discussion of KCS.
Figure 5.7 Right eye of a 5-year-old, castrated male pug. Note the corneal melanosis in the medial corneal quadrant. Melanosis results from chronic corneal irritation, which is caused in this case by ventromedial entropion, corneal contact with the nasal fold, lagophthalmos, macroblepharon, and exophthalmos. The lesions are bilateral and symmetrical. Pigmentary keratitis and brachycephalic ocular syndrome are discussed on pages 103 to 104 and 62 to 63, respectively.
Chapter 5
Figure 5.8 Conjunctival hyperemia, superficial corneal vascularization, and corneal fibrosis (chronic, superficial keratoconjunctivitis) resulting from previous corneal ulceration. The corneal fibrosis is dense, white, and linear in this photograph. It is associated with irregularities of the corneal surface (as evidenced by the indistinct borders of the camera flash in the central cornea). Keratitis is discussed on pages 100 to 101, and 111 to 112.

Figure 5.9 Left conjunctival hyperemia, deep corneal vascularization, corneal edema, and corneal white cell infiltrate (chronic stromal keratitis) following left ocular proptosis and corneal ulceration. Unlike superficial corneal vessels, deep vessels rarely branch. The corneal edema is responsible for the blue change in the lateral cornea, and the white cell infiltrate is responsible for the yellow discoloration of the medial cornea. Keratitis and white cell infiltrates are discussed on pages 100 to 101 and 111 to 112, and 99, respectively.
Figure 5.10 Corneal dystrophy in a Siberian husky. White, refractile deposits without any associated keratitis are characteristic. Also characteristic are the overall oval shape and the central location. This condition is bilateral and symmetrical and is not associated with visual compromise or other ocular pathology. Corneal dystrophy is discussed on pages 99 and 100.
Figure 5.11 White, crystalline opacities in the central cornea. This is present in both eyes. The oval shape, crystalline white color, central location, symmetry between eyes, and lack of concurrent ocular pathology are supportive of corneal dystrophy. This dog did not show any signs of ocular discomfort or visual compromise. Corneal dystrophy is discussed on pages 99 and 100.
Chapter 5 Cornea 23
Chapter 5
24 Section I Atlas
Figure 5.12 Chronic, superficial keratitis. Dense, refractile, white deposits are associated with superficial corneal vascularization. Although the deposits were present bilaterally, they were not symmetrical between eyes. Because of the asymmetry and the associated keratitis, this was not consistent with corneal dystrophy. A diagnosis of corneal degeneration is more appropriate. See pages 99 to 100.
Figure 5.13 Chronic, superficial nonulcerative keratitis due to KCS. The copious and tenacious mucoid discharge is characteristic of KCS. Superficial corneal vascularization is another characteristic of KCS. The STT in this eye was 8 mm/min. KCS is discussed on pages 101 to 103.
Chapter 5
Figure 5.14 Typical appearance of pannus, or chronic superficial keratitis, in the left eye of a German shepherd. Corneal melanosis affects the ventrolateral peripheral cornea. In pannus, this is the typical location for melanosis to arise from (in contrast to pigmentary keratitis). Pannus is discussed on pages 104 and 105.
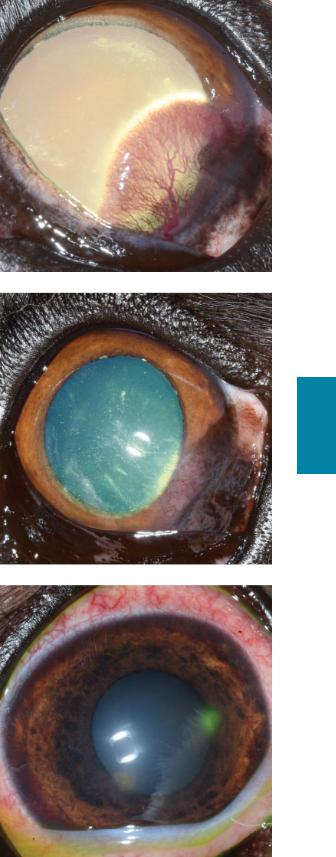
Figure 5.15 Pannus with a more fibrovascular component than in the previous figure. Corneal melanosis is present in the ventrolateral cornea. However, the predominant feature in this case is superficial corneal vascularization, also located ventrolaterally. The leading edge of the third eyelid is mildly depigmented. Pannus is discussed on pages 104 and 105.
Figure 5.16 Pannus in the left eye of a German shepherd. Corneal melanosis and superficial vascularization affect the ventrolateral corneal quadrant. Linear, white wisps are visible in the ventral corneal quadrant; these are likely lymphocytes infiltrating the cornea (Williams, 1999).
Figure 5.17 Right eye of a shih tzu presenting with a 1-day history of a red eye and excessive tearing. There is moderate conjunctival hyperemia and superficial corneal fluorescein retention. This ulcer is considered simple because it is acute, superficial, and there are no signs of white cell infiltrate or melting. The white opacity extending from the ulcer to the 6 o’clock limbus is a reflection. Simple corneal ulcers are discussed on pages 105 and 106.
Chapter 5 Cornea 25
Chapter 5

26 Section I Atlas
Figure 5.18 Indolent corneal ulcer of the right eye of a 9-year-old, spayed female boxer. Red arrowheads indicate the edges of the epithelial defect. However, because the epithelium is not adhering to the underlying stroma, fluorescein has been taken up by stroma beyond the epithelial edge (underneath epithelium) up to the area indicated by the black arrowheads. Mild corneal edema and superficial corneal vascularization obscure the ventrolateral iris. Also note the indistinct edges of the camera flash, indicating a roughened corneal surface. Indolent corneal ulcers are discussed on pages 106 to 108.
Figure 5.19a Indolent corneal ulcer with nonadherent epithelium. The red arrowhead indicates the edge of the epithelial defect. The epithelium is present but nonadherent to the underlying stroma between the red and the black arrowheads. Similar changes can be seen around the entire circumference of the ulcer. The disrupted reflection of the camera flash indicates that the central cornea, near the edge of the defect, is uneven. Indolent corneal ulcers are discussed on pages 106 to 108.
Chapter 5
Figure 5.19b The same ulcer as in the previous figure (with similar arrowhead placement) after application of fluorescein stain. This photograph shows fluorescein retention by stroma that has overlying but nonadherent epithelium (between the red and the black arrowheads). Similar patterns of fluorescein retention are visible around the circumference of the ulcer. Indolent corneal ulcers are discussed on pages 106 to 108.

Figure 5.20 Chronic, deep ulcerative keratitis. In addition to the deep ulcer, KCS was diagnosed because the STT was 0 mm/min. The visible crater in the cornea indicates stromal loss; the cornea within the defect is clearer than the surrounding cornea because it is much thinner. This defect retained fluorescein stain when it was applied. The surrounding cornea is edematous, with deep vascular ingrowth. Chemosis and conjunctival hyperemia are also present. The copious amount of mucoid ocular discharge is a common finding with low tear production. Deep corneal ulcers are discussed on pages 108 to 110. KCS is discussed on pages 101 to 103.
Figure 5.21a Descemetocele. Note the deep, central corneal defect. Fluorescein stain is retained by corneal stroma exposed at the periphery of this defect. However, fluorescein is not retained in the center of the defect, which appears black. This indicates loss of the entire corneal stroma centrally, with only hydrophobic Descemet’s membrane and corneal endothelium intact. Deep corneal ulcers are discussed on pages 108 to 110.
Figure 5.21b The same eye as in the previous figure. This photo was taken using the cobalt blue filter to highlight the pattern of fluorescein uptake.
Chapter 5 Cornea 27
Chapter 5

28 Section I Atlas
Figure 5.22 Perforated left cornea. The brown, central lesion is iris plugging a full-thickness corneal defect. Immediately surrounding the perforation, there is corneal stromal loss. The remainder of the cornea is edematous (most pronounced around the area of stromal loss). Superficial and deep corneal vessels, indicating chronicity, can be seen entering the cornea. Corneal melanosis is visible medial to the perforation. This patient was treated with a conjunctival graft. Deep and perforating corneal ulcers are discussed on pages 108 to 110.
Figure 5.23 Corneal perforation. The iris is the red object in the central cornea. The surrounding cornea is edematous. Deep corneal vessels (indicating chronicity) are visible at the limbus dorsally and laterally; the remainder of the red discoloration is hyphema viewed through the cornea. Deep and perforating corneal ulcers are discussed on pages 108 to 110.
Chapter 5
Figure 5.24 The large brown and pink structure protruding from the central cornea is the iris. Surrounding cornea is edematous with ingrowth of deep corneal vessels. Due to the severity of this injury, the globe was enucleated. Deep and perforating corneal ulcers are discussed on pages 108 to 110.

Figure 5.25 Melting corneal ulcer. There is diffuse corneal edema, and deep corneal vessels are present near the limbus. The central, white lesion is protruding from the corneal surface and appears soft. This is the area of corneal melting. It is raised from the corneal surface because as the malacic cornea loses it normal solid form, it deforms. A second white lesion ventral to this is hypopyon. Melting corneal ulcers are discussed on pages 110 and 111.
Figure 5.26 Perforated melting corneal ulcer. The central, red lesion is iris that has protruded through a corneal perforation. Malacic cornea is visible around the iris and exuding over the surface of the iris. Episcleral hyperemia and deep corneal vascularization are also visible in this photograph. Due to the severity of ocular disease and grave prognosis, the eye was enucleated. Melting corneal ulcers are discussed on pages 110 and 111.
Figure 5.27 Dendritic refers to the linear branching nature of the superficial corneal ulcers shown here. These are pathognomonic for FHV-1 infection. The cobalt blue filter of the direct ophthalmoscope enhances visualization of fluorescein. See pages 111 and 112 for discussion of feline corneal ulcers.
Chapter 5 Cornea 29
Chapter 5

30 Section I Atlas
Figure 5.28 Chronic, superficial keratoconjunctivitis (chemosis, conjunctival hyperemia, superficial corneal vascularization, and corneal edema) due to eosinophilic keratoconjunctivitis. The raised, round, white structures on the cornea and conjunctiva near the dorsolateral limbus are white cell plaques. Eosinophilic keratoconjunctivitis is discussed on pages 112 and 113.
Figure 5.29 Eyelid depigmentation, chemosis, conjunctival hyperemia, superficial corneal vascularization, and corneal plaques due to eosinophilic keratoconjunctivitis. The plaques in this photo differ from those in the previous photo because they are more diffuse. However, regardless of plaque appearance, the association of white cell plaques with chronic superficial keratoconjunctivitis in cats should raise clinical suspicion for eosinophilic keratoconjunctivitis. Eosinophilic keratoconjunctivitis is discussed on pages 112 and 113.
Chapter 5
Figure 5.30 Chronic, superficial keratitis, diagnosed via corneal cytology as eosinophilic keratoconjunctivitis. In contrast to the previous two figures, the white cell infiltrate has not formed discrete, raised plaques on the cornea. This underscores the importance of cytology for obtaining a diagnosis (see page 112). Eosinophilic keratoconjunctivitis is discussed on pages 112 and 113.
