
Gale Encyclopedia of Genetic Disorder / Gale Encyclopedia of Genetic Disorders, Two Volume Set - Volume 2 - M-Z - I
.pdf
Demographics
The incidence of all the conditions that cause methylmalonicacidemia was reported in a Massachusetts screening program at approximately one in 48,000 births. About half of the reported patients with methylmalonicacidemia have a deficiency of MCM mut0 or mut-), as opposed to problems with the cofactor. Thus, incidence of specific MCM deficiency-related methylmalonicacidemia and aciduria in the general population may be estimated as one in 96,000. The geographical distribution of methylmalonicacidemia is not uniform and may be higher in certain ethnic groups. One report shows that the disorder is more common in the Middle East, probably occurring in one in 1,000 or 2,000 births. MCM deficiency is seen in equal amounts in males and females.
Signs and symptoms
The symptoms experienced by an infant with MCM deficiency vary with the type of mutation present. Infants born with the mut0 type MCM deficiency will typically show more severe symptoms that manifest in the first 1- 2 weeks of life, while infants with the mut- type MCM deficiency will have slightly milder symptoms that begin later in infancy.
Both sets of infants may show poor feeding, vomiting, lethargy, and low muscle tone, as well as a failure to grow at the normal rate. The disorder may first come to medical attention as it escalates into a full scale overwhelming attack, often triggered by intake of large amounts of dietary protein. If the condition has not yet been diagnosed, treatment is often poor, and patients may experience kidney damage, inflammation of the pancreas, or strokes that result in severe paralysis. More severe attacks can lead to seizures, coma, and eventually, death. As a result, newborns and infants with MCM deficiency may die early, even before a diagnosis can be reached.
If the infant survives the first attack, similar attacks may occur during an infection or following ingestion of a high-protein diet. Between episodes the patient may appear normal, but often, mild to moderate mental retardation will develop. Some infants with this disorder have characteristic facial features with a broad nose bridge, prominent lower eyelid folds, triangular mouth, and high forehead. Other symptoms of the disorder include frequent infections (especially yeast infections of the skin and mouth), enlarged liver, and low amounts of red blood cells. Often a family history is present for affected siblings or siblings that died very early in life for unclear reasons.
K E Y T E R M S
Amino acid—Organic compounds that form the building blocks of protein. There are 20 types of amino acids (eight are “essential amino acids” which the body cannot make and must therefore be obtained from food).
Antibiotics—A group of medications that kill or slow the growth of bacteria.
Autosomal recessive—A pattern of genetic inheritance where two abnormal genes are needed to display the trait or disease.
Carrier—A person who possesses a gene for an abnormal trait without showing signs of the disorder. The person may pass the abnormal gene on to offspring.
Cofactor—A substance that is required by an enzyme to perform its function.
Enzyme—A protein that catalyzes a biochemical reaction or change without changing its own structure or function.
Methylmalonic acid—An intermediate product formed when certain substances are broken down in order to create usable energy for the body.
Methylmalonic CoA mutase (MCM)—The enzyme responsible for converting methylmalonic acid to succinic acid, in the pathway to convert certain substances to usable energy.
Methylmalonicacidemia—The buildup of high levels of methylmalonic acid in the bloodstream due to an inborn defect in an enzyme.
Methylmalonicaciduria—The buildup of high levels of methylmalonic acid in the urine due to an inborn defect in an enzyme.
Mutation—A permanent change in the genetic material that may alter a trait or characteristic of an individual, or manifest as disease, and can be transmitted to offspring.
Protein—Important building blocks of the body, composed of amino acids, involved in the formation of body structures and controlling the basic functions of the human body.
A small percentage of people with the MCM deficiency apparently experience no symptoms or complications of the disease. For reasons not yet understood, these patients can tolerate a normal protein intake and accumulate high levels of methylmalonic acid in their body fluids without consequence.
deficiency mutase CoA methylmalonic to due Methylmalonicaciduria
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
739 |
Methylmalonicaciduria due to methylmalonic CoA mutase deficiency
Diagnosis
When symptoms such as those described above are encountered in a young infant or newborn, a diagnostic search for MCM deficiency should be considered. A routine blood test performed on almost all people who come to the hospital with severe illness will show high levels of acid in the bloodstream. Other clues to possible MCM deficiency include high levels of other substances in the bloodstream that appear with methylmalonicacidemia such as ketones and ammonia, or the presence of abnormally low amounts of glucose or red blood cells.
After high levels of acid in the bloodstream are noted, and if methylmalonicacidemia is suspected, samples of the urine and the blood will be taken and tested for the amount of methylmalonic acid. Abnormally high levels of methylmalonic acid suggest that MCM deficiency may be present. Genetic studies can then be performed to determine if any mutation in the MCM gene is present.
When the disease is diagnosed in a child, research laboratories can test unaffected siblings to determine if they are carriers of the mutant MCM gene. The same technology can be used to diagnose MCM deficiency before the birth of a child, by analyzing fluid or tissue from the sac surrounding the unborn fetus.
Treatment and management
Current research into a cure for MCM deficiency is focusing on the ability of liver transplantation or gene therapy to correct the abnormal MCM gene, however there is no cure for MCM deficiency at this time. The methods of treatment focus on three areas: diet/lifestyle modification, treatment with medications, and support during severe attacks of the disease.
Dietary changes include restriction of the amino acids that are converted to methylmalonic acid: methionine, threonine, valine, and isoleucine. As a result, people with MCM deficiency are limited to a low protein diet that provides the minimum natural protein needed for growth. Calcium and multivitamin supplements should also be taken to correct any nutritional deficiencies that result from avoiding high-protein foods. Activity in children with MCM deficiency need not be restricted.
People with MCM deficiency may benefit from several medications when taken daily. The antibiotic, metronidazole, kills bacteria that live in the intestine and produce substances that are converted to methylmalonic acid. The supplement, L-carnitine, is often used to reduce some of the toxic effects of high levels of methylmalonic acid. Although most reports state that there is no benefit from vitamin B12 supplementation, a few reports suggest
that a trial of vitamin B12 may be reasonable to determine if it will result in improved MCM function. Finally, bicarbonate can be used to counteract low levels of acid that persist in the bloodstream.
All of the above medications can be used to aid in treatment of a severe attack of methylmalonicacidemia. In addition, a patient in crisis should be given excessive amounts of intravenous fluids, to help clear methylmalonic acid from the circulation. Special blood filtering machines can be used when levels of methylmalonic acid or ammonia become dangerously high. Stressful situations that may trigger attacks (such as infection) should be treated promptly.
Patients with MCM deficiency should be seen regularly by a team of health care specialists including a primary care provider, a dietician, and a biochemical geneticist who is familiar with the management of the disease. Parents should be educated in the signs and symptoms of impending attacks and how to respond appropriately. Close monitoring of amino acid levels, urinary content of methylmalonic acid, and growth progress is necessary to ensure proper balance in the diet and the success of therapy.
Prognosis
Prognosis depends on early and accurate diagnosis of the disease and the prompt initiation of diet modification and medications. In those infants who escape early diagnosis, the prognosis is poor as severe attacks will lead to complications as extreme as sudden death. In those infants that do survive initial attacks, damage to the developing brain and kidneys may result that leave the child severely incapacitated.
The addition of the medications, L-carnitine and metronidazole, to the management of this disorder has changed the prognosis. Scientists point out that although most patients before 1985 died, those after 1985, when these drugs were introduced, survived with improved general health. Thus, if detected early and treated appropriately, the lifestyle of a well-managed patient with MCM deficiency can be relatively normal, without mental retardation or growth delay.
Resources
BOOKS
Behrman, R.E., ed. Nelson Textbook of Pediatrics. Philadelphia: W.B. Saunders, 2000.
Fauci, A.S., ed. Harrison’s Principles of Internal Medicine.
New York: McGraw-Hill, 1998.
740 |
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
PERIODICALS
Ledley, F.D. “Mutations in mut methylmalonic acidemia: clinical and enzymatic correlations.” Human Mutation 9 (1997): 1–6.
ORGANIZATIONS
Support Groups For MMA Organic Acidemia Association. 13210 35th Avenue Plymouth, MN 55441. (763) 5591797. http://www.oaanews .
WEBSITES
“Methylmalonicaciduria due to MCM Deficiency.” Online Mendelian Inheritance in Man. http://www3.ncbi.nlm
.nih.gov/htbin-post/Omim/dispmim?251000 .
Oren Traub, MD, PhD
Microcephaly with spastic diplegia selmanona syndrome I see Paine syndrome
Microcephaly-mental retardationtracheoesophageal fistual syndrome see
Oculo-digito-esophago-duodenal syndrome
Microcephaly-mesobrachyphalangy- tracheo-esophagael fistula syndrome (MMT) see Oculo-digito-esophago- duodenal syndrome
I Microphthalmia with linear skin defects (MLS)
Definition
Microphthalmia with linear skin defects (MLS) is a rare genetic disorder that causes abnormalities of the eyes and skin. This disorder was first recognized as a distinct genetic condition in 1990.
Description
MLS is a rare disorder that is observed only in females because males with the disease do not survive to birth. This disorder is also called MIDAS (Microphthalmia, dermal aplasia, and sclerocornea) syndrome. People affected by MLS have:
•small sunken eyes (microphthalmia),
•irregular red streaks of skin on the head and neck (skin erythema),
K E Y T E R M S
Cornea—The transparent structure of the eye over the lens that is continous with the sclera in forming the outermost, protective, layer of the eye.
de novo mutation—Genetic mutations that are seen for the first time in the affected person, not inherited from the parents.
Microphthalmia—Small or underdeveloped eyes.
Orbital cysts—Small fluid-filled sacs that abnormally develop inside the bony cavity of the skull that holds the eyeball.
Sclera—The tough white membrane that forms the outer layer of the eyeball.
Septum pellucidum—A membrane between two of the normal cavities of the brain that prevents electrical signals from passing between different portions of the brain.
Skin erythema—Irregular red streaks of skin.
Terminal deletion—The abnormal early termination of a chromosome caused by the deletion of one of its ends.
•and abnormal development of the sclera and cornea of the eye.
The eye is composed of three layers: the sclera, the choroid, and the retina. The sclera is the tough white outer coat of the eyeball. As this coat passes over the lens, it normally becomes clear. This clear portion of the sclera is the cornea. Both the sclera and the cornea are affected by MLS.
The choroid is the middle layer of the eye. It serves to nourish the retina and absorb scattered light. The retina is the inner, light-sensitive, layer of the eye. The retina receives the image transmitted by the lens and it contains the rods and cones that are responsible for color vision and vision in dim light. Both the choroid and the retina are unaffected by MLS.
Genetic profile
The gene responsible for MLS has been localized to a portion of the short arm (p) of the X chromosome (Xp22.3). The specific symptoms of MLS are believed to result from the premature cutoff (terminal deletion) of the X chromosome at this point. People with MLS do not have the portion of the short arm of the X chromosome beyond the Xp22.2 location.
(MLS) defects skin linear with Microphthalmia
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
741 |
Microphthalmia with linear skin defects (MLS)
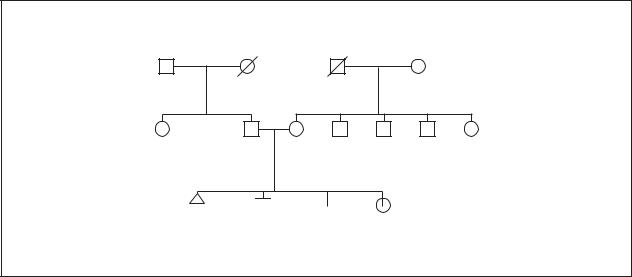
Microphthalmia with Linear Skin Defects
2 


 Early miscarriages Small, sunken eyes
Early miscarriages Small, sunken eyes
Red streaking on skin Diaphragmatic hernia Breathing problems
(Gale Group)
Nearly all of the cases of MLS are believed to result from de novo mutations since parents of affected individuals do not carry the MLS mutation in their chromosomes. A de novo mutation is caused by a problem with the chromosomes of the parental egg or sperm cells. The remainder of the chromosomes in the parents are not affected. As the sex cells of one of the parents reproduce, an error occurs. This leads to the transmission of a new mutation from that parent to his or her child. This mutation is expressed for the first time in the child of that parent.
A typical female has two X chromosomes. A typical male has one X chromosome and one Y chromosome. Because no XY male has ever been diagnosed with MLS, it is assumed that MLS is dominant and X-linked with 100% fetal mortality in males. This type of genetic disorder is also called an X-linked male-lethal trait.
There have been a few reported cases of males affected with MLS. These individuals presumably survived because they were XXY males (genetically female with ambiguous or male sex organs), rather than the typical male with XY chromosomes. This condition (XXY) is called Klinefelter syndrome.
Demographics
Approximately 300 individuals, all without a Y chromosome, have been diagnosed with MLS worldwide. MLS is not associated with any particular sub-popula- tions. It appears with equal frequency in all races and across all geographies. Because it is an X-linked male-
lethal trait, it is observed exclusively in females or, in a few cases, in XXY males.
Signs and symptoms
MLS is characterized by:
•small, sunken, eyes (microphthalmia);
•defects of the sclera and cornea portions of the eye
•linear red streaking of the skin on the upper body, primarily the head and neck;
•abnormal protrusion of the abdominal contents upward through an opening in the diaphragm (diaphragmatic hernia), which causes difficulty with breathing (respiratory distress);
•a lack of the transparent membrane (septum pellucidum) in the brain that forms a wall between two of the normal cavities (the lateral ventricles) of the brain;
•and, a condition in which the heart is located on the right side, rather than the left side, of the chest (dextrocardia).
In individuals affected with MLS, the bony cavity that contains the eyeball (orbit) often contains small fluid-filled sacs (orbital cysts). The sclera is often not fully or properly formed, and the cornea generally has areas that are opaque rather than transparent. This corneal opacity causes blurring of vision and may result in blindness. Corneal opacities should not be confused with cataracts, which are opacities of the lens of the eye, not of the cornea.
742 |
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
Difficulty in breathing (respiratory distress) is seen at birth in some patients with MLS. This is caused by a hole in the muscle beneath the lungs (diaphragm) that is responsible for the flow of air into and out of the lungs. This condition will rapidly lead to death if it is not surgically repaired.
Seizures and mental retardation have been observed in some MLS patients. It is believed that these individuals do not have a septum pellucidum. The absence of this membrane may allow electrical transmissions between parts of the brain that are usually isolated from each other. These inadvertent electrical signals may cause the seizures and the mental retardation that is sometimes seen in MLS patients.
Diagnosis
MLS is generally diagnosed by the presence of the characteristic red striping of the skin on the head and neck accompanied by small eyes (microphthalmia) and opaque patches on the corneas.
MLS is differentiated from Goltz syndrome, which has a similar gene locus, in that the patient with MLS has skin irregularities only on the upper half of the body, most typically only on the head and neck. Goltz syndrome tends to result in skin irregularities across their entire bodies. Also, patients with MLS do not have the abnormal fatty tissue deposits seen under the skin of Goltz syndrome patients. Finally, MLS does not have the clefting of the hands or feet (syndactyly) or incomplete formation of certain structures of the eyes (coloboma) seen in Goltz syndrome.
In early 2001, prenatal diagnosis for MLS syndrome was not yet available, but identification of the gene responsible for MLS makes genetic testing for this dominant trait potentially possible.
Treatment and management
The treatment and management of MLS is directed toward the symptoms seen in each patient. All those affected with MLS will need eye care including surgeries to potentially repair damaged areas of the cornea and sclera. Some individuals may require skin care treatments depending on the severity of the skin abnormalities.
In cases of patients with a diaphragmatic hernia, emergency surgery shortly after birth may be necessary to attempt to repair the damaged area. Unfortunately, most cases of this type of hernia cannot be surgically corrected and the patient will die.
In cases of patients with a lack of the septum pellucidum in the brain, anti-seizure medication may be necessary to control the seizures.
Prognosis
MLS is lethal in males prior to birth. In females, a full life expectancy is possible if the complications are not severe and if medical treatment is followed.
Most problems of the cornea and sclera of the eye associated with MLS can be treated with corrective lenses or potentially surgically repaired with corneal implants or laser surgery.
Seizures, if present, can generally be controlled by anti-seizure medications.
Developmental delays in growth, motor ability, speech, and intellect occur in some, but not all, cases of MLS. The amount of delay that is observed is directly related to the severity of seizure activity in the brain caused by the malformation, or lack, of the septum pellucidum.
Resources
PERIODICALS
Kuno, T., T. Migita. “Another observation of microphthalmia in an XX male: microphthalmia with linear skin defects syndrome without linear skin lesions.” Journal of Human Genetics (1999): 63-8.
ORGANIZATIONS
National Foundation for the Blind. 1800 Johnson St., Baltimore, MD 21230. (410) 659-9314. http://www.nfb
.org .
National Organization for Rare Disorders (NORD). PO Box 8923, New Fairfield, CT 06812-8923. (203) 746-6518 or (800) 999-6673. Fax: (203) 746-6481. http://www
.rarediseases.org .
WEBSITES
“Multiple Congenital Anomaly/Mental Retardation (MCA/ MR) Syndromes.” United States National Library of Medicine. http://www.nlm.nih.gov/mesh/jablonski/syndromes/ syndrome453.html . (February 9, 2001).
“Entry 309801: Micropthalmia with linear skin defects; MLS.” OMIM—Online Mendelian Inheritance in Man.
http://www.ncbi.nlm.nih.gov/htbin-post/Omim/ dispmim?309801 . (February 9, 2001).
Paul A. Johnson
MIDAS syndrome see Microphthalmia with linear skin defects
Mild hypophosphatasin see
Hypophosphatasia
(MLS) defects skin linear with Microphthalmia
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
743 |

Miller-Dieker syndrome
I Miller-Dieker syndrome
Definition
Miller-Dieker syndrome (MDS) is a rare genetic disorder. Its signs and symptoms include severe abnormalities in brain development as well as characteristic facial features. Additional birth defects may also be present.
Description
MDS was named for the two physicians, J. Miller and H. Dieker who independently described the condition in the 1960s. The hallmark of MDS is lissencephaly (smooth brain), a condition in which the outer layer of the brain, the cerebral cortex, is abnormally thick and lacks the normal convolutions (gyri). In some areas of the brain, gyri are fewer in number but wider than normal (pachygyri). Other areas lack gyri entirely (agyri). Normally, during the third and fourth months of pregnancy, the brain cells in the baby multiply and move to the surface of the brain to form the cortex. Lissencephaly is caused by a failure of this nerve cell migration. MDS is often called Miller-Dieker lissencephaly syndrome.
Genetic profile
When MDS was first described, geneticists thought it followed an autosomal recessive pattern of inheritance. However, in the early 1990s, several patients with MDS were found to be missing a small portion of the short arm of chromosome 17 (17p13.3). This is called a partial deletion of chromosome 17. MDS is now classified as a “micro-deletion syndrome” because it is the result of the absence of genes that are normally located in this region of chromosome 17. In 1993, research scientists identified one of the genes in this region. They named it LIS1 for “first lissencephaly gene” because it appeared to be important in normal brain formation. The main evidence for this was that the LIS1 gene was missing in a number of individuals with isolated lissencephaly; that is, lissencephaly without the additional characteristics found in MDS. Researchers then studied a number of patients with MDS and found over 90% of them were missing the LIS1 gene as well as other, as yet unidentified genes, on the short arm of chromosome 17. Geneticists now think that the characteristic facial appearance and other abnormalities seen in MDS are due to the deletion of these other genes. For this reason, MDS has also been described as a “contiguous gene syndrome”.
Most genes, including all genes on the autosomes (non-sex chromosomes), are normally present in pairs. Individuals with MDS who have a micro-deletion of a small region of the short arm of one copy of their chro-
mosome 17 still have one normal copy of this chromosome region on their other chromosome 17. For this reason, MDS is said to be due to “haploinsufficiency,” the term for a genetic condition caused by the lack of function of only one of the two copies of a gene. As with other haploinsufficiency syndromes, MDS has also been described as having an autosomal dominant pattern of inheritance.
Individuals with MDS usually die in infancy. Because they do not live to the age where they can reproduce, they cannot transmit MDS to their offspring. Eighty percent of individuals with MDS have it as the result of a new (de novo) deletion of a small part of the short arm of one chromosome 17 in just the one egg or sperm that formed that individual. The parents of these affected individuals have normal chromosomes without deletions. This means that their risk of having another child with MDS is very low (probably less than 1%). However, the other 20% of those with MDS have the syndrome because one of their parents carries a rearrangement of one copy of their own chromosome 17. The rearrangement can be an inversion or a balanced translocation between chromosome 17 and one of the other chromosomes. Since the rearrangement is balanced; that is, all the chromosome material is present but in a rearranged form, the parent is normal. However, when that parent produces an egg or a sperm, the balanced chromosome rearrangement can go through a further rearrangement. This results in a portion of the short arm of chromosome 17 being deleted. The individual who develops from that egg or sperm will have MDS.
Demographics
MDS is present in fewer than one in 100,000 births. There is no information to suggest that the syndrome is more common in any particular ethnic or racial group.
Signs and symptoms
Infants with MDS are usually small at birth. Characteristic facial features may include a high forehead with furrows and vertical ridges, indentation of the temples, a small, upturned nose, up-slanting eyes, a small mouth, a thick, broad upper lip with a thin border, low-set ears, and occasionally, a cleft palate. Some infants with MDS also have birth defects involving the heart and kidneys. Signs and symptoms can vary among MDS patients. This may relate to the actual size or exact location of the chromosome 17 deletion in that individual.
MDS infants have a very limited capacity for development due to the lissencephaly and associated brain abnormalities. Mental retardation is severe to profound.
744 |
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |

K E Y T E R M S
Amniocentesis—A procedure performed at 16-18 weeks of pregnancy in which a needle is inserted through a woman’s abdomen into her uterus to draw out a small sample of the amniotic fluid from around the baby. Either the fluid itself or cells from the fluid can be used for a variety of tests to obtain information about genetic disorders and other medical conditions in the fetus.
Autosomal dominant—A pattern of genetic inheritance where only one abnormal gene is needed to display the trait or disease.
Autosomal recessive—A pattern of genetic inheritance where two abnormal genes are needed to display the trait or disease.
CAT (CT) scan—Computerized (axial) tomography. A special x ray technique used to examine various tissues, particularly the brain, in great detail.
Cerebral cortex—The outer surface of the cerebrum made up of gray matter and involved in higher thought processes.
Chorionic villus biopsy—A procedure used for prenatal diagnosis at 10-12 weeks gestation. Under ultrasound guidance a needle is inserted either through the mother’s vagina or abdominal wall and a sample of cells is collected from around the fetus. These cells are then tested for chromosome abnormalities or other genetic diseases.
Contiguous gene syndrome—A genetic syndrome caused by the deletion of two or more genes located next to eachother.
FISH (fluorescence in situ hybridization)—
Technique used to detect small deletions or rearrangements in chromosomes by attempting to attach a fluorescent (glowing) piece of a chromosome to a sample of cells obtained from a patient.
Gastrostomy—The construction of an artificial opening from the stomach through the abdominal wall to permit the intake of food.
Haploinsufficiency—The lack of one of the two normal copies of a gene. Haploinsufficiency can result in a genetic disorder if normal function
requires both copies of the gene. Haploinsufficiency is one explanation for a dominant pattern of inheritance.
Hypotonia—Reduced or diminished muscle tone.
Inversion—A type of chromosomal defect in which a broken segment of a chromosome attaches to the same chromosome, but in reverse position.
Lissencephaly—A condition in which the brain has a smooth appearance because the normal convolutions (gyri) failed to develop.
Magnetic resonance imaging (MRI)—A technique that employs magnetic fields and radio waves to create detailed images of internal body structures and organs, including the brain.
Micro-deletion syndrome—A collection of signs and symptoms caused by a deletion of a gene or genes that is too small to be seen through the microscope.
Microcephaly—An abnormally small head.
Opisthotonos—An arched position of the body in which only the head and feet touch the floor or bed when the patient is lying on their back.
Prenatal diagnosis—The determination of whether a fetus possesses a disease or disorder while it is still in the womb.
Syndrome—A group of signs and symptoms that collectively characterize a disease or disorder.
Translocation—The transfer of one part of a chromosome to another chromosome during cell division. A balanced translocation occurs when pieces from two different chromosomes exchange places without loss or gain of any chromosome material. An unbalanced translocation involves the unequal loss or gain of genetic information between two chromosomes.
X-linked—Located on the X chromosome, one of the sex chromosomes. X-linked genes follow a characteristic pattern of inheritance from one generation to the next.
Infants with MDS may be able to do little more than roll |
and increases the risk of pneumonia because the infants |
over. Convulsions (seizures) develop within a few weeks |
can accidentally inhale baby formula into their lungs. |
of birth and can be severe. Most newborns with MDS |
Head size is usually in the normal range at birth, but poor |
have low muscle tone (hypotonia), but later develop stiff- |
brain growth means that, by the age of one year, the chil- |
ness (spasticity) and an arching of the body |
dren have a smaller-than-normal head size (micro- |
(opisthotonos). Poor feeding leads to a failure to thrive |
cephaly). |
syndrome Dieker-Miller
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
745 |
Miller-Dieker syndrome
Diagnosis
MDS is not the only disorder associated with lissencephaly. Autosomal dominant, autosomal recessive, and X-linked patterns of inheritance have been described among the more than two dozen genetic syndromes featuring this brain abnormality. Less commonly, lissencephaly can also be the result of fetal infections such as prenatal cytolomegalovirus (CMV). An accurate diagnosis of MDS is important not only because it can provide a prognosis for the affected child, but because it can give parents an estimate of their risk for having another child with MDS.
MDS may be suspected in the newborn period if an infant has the characteristic facial features along with low muscle tone. Studies of the infant’s brain by CAT scan or MRI will show the smooth brain surface. After the diagnosis of MDS is made on the basis of these signs and symptoms, it is very important to study the infant’s chromosomes to check for the characteristic chromosome 17 deletion. This is done by sending a small sample of the infant’s blood to a cytogenetics laboratory. Trained laboratory personnel (cytogeneticists) first examine the infant’s chromosomes through the microscope using traditional techniques. If no deletion or other chromosome rearrangement is detected in this step, newer methods can be used to search for deletions that are too small to see by ordinary means (micro-deletions). A special technique called FISH (fluorescent in situ hybridization) can detect chromosome regions where very small pieces of DNA are missing. This test is usually done on the same blood sample.
Carrier detection
When a chromosome deletion is found in an infant, both parents’ chromosomes should also be studied to determine if one of them carries a chromosome rearrangement such as a balanced translocation. Although most parents of infants with MDS have normal chromosomes, in approximately 20% of children, one parent will have a chromosome rearrangement, which can increase the risk for having another child with MDS. Other family members should also be offered chromosome studies because these balanced chromosome rearrangements can be passed down through a family undetected, and, thus, other family members may be carriers. The first step in studying other family members is for a geneticist or genetic counselor to obtain a detailed family history and construct a pedigree (family tree) to determine which family members should be offered testing.
Prenatal diagnosis
If a couple has had one child with MDS, they can be offered prenatal diagnosis in future pregnancies. This
option is particularly important for the 20% of MDS families where one parent carries a balanced chromosome rearrangement. The risk for these couples to have another affected child depends on the exact type of chromosome rearrangement present and may be as high as 25-33%. For families in which both parents’ chromosomes are normal, the risk of having another child with MDS is low (1% or less). Either chorionic villus sampling (CVS) or amniocentesis can be used early in a pregnancy to obtain a small sample of cells from the developing embryo for chromosome studies. Early prenatal diagnosis by ultrasound is not reliable because the brain is normally smooth until later in pregnancy. Couples who are considering prenatal diagnosis should discuss the risks and benefits of this type of testing with a geneticist or genetic counselor.
Treatment and management
There is no cure for MDS and treatment is usually directed toward comfort measures. Because of the feeding problems and risk of pneumonia, surgeons often place a tube between the stomach and the outside of the abdomen (gastrostomy tube). Feedings can be made through the tube. Seizures are often difficult to control even with medication.
Prognosis
Death often occurs in the first three months of life and most infants with MDS die by two years of age, although there have been reports of individuals living for several years.
Resources
BOOKS
Jones, Kenneth Lyons. Smith’s Recognizable Patterns of
Human Malformations, 5th ed. Philadelphia, W. B.
Saunders, 1997.
ORGANIZATIONS
Lissencephaly Network, Inc. 716 Autumn Ridge Lane, Fort Wayne, IN 46804-6402. (219) 432-4310. Fax: (219) 4324310. lissennet@lissencephaly.org. http://www
.lissencephaly.org .
WEBSITES
“Entry 247200: Miller-Dieker Lissencephaly Syndrome.”
OMIM—Online Mendelian Inheritance in Man.
http://www.ncbi.nlm.nih.gov/htbin-post/Omim . Dobyns, W. B. “Lissencephaly and subcortical band heterotopia
(Agyria-pachygyria-band spectrum) Overview.” (updated October 4, 1999). GeneClinics: Clinical genetic information resource. University of Washington, Seattle.http://www.geneclinics.org .
”Lissencephaly, Information for Parents.”http://www.lissencephaly.org/about/lissen.htm .
746 |
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
The Lissencephaly Network, Inc.
http://www.kumc.edu/gec/support/lissence.html .
Sallie Boineau Freeman, PhD
Mirhosseini-Holmes-Walton syndrome see
Cohen syndrome
MODY—Maturity-onset diabetes of the young see Diabetes mellitus
I Möebius syndrome
Definition
Möebius syndrome is a condition in which the facial nerve is underdeveloped, causing paralysis or weakness of the muscles of the face. Other nerves to the facial structures may also be underdeveloped.
Description
Möebius syndrome has been called “life without a smile” because the paralysis of the facial muscles, the most constant feature, leads to the physical inability to form a smile even when happy feelings are experienced. The facial nerve is one of a group of 12 nerves known as the cranial nerves because they originate in the brain. The facial nerve is also known as the seventh cranial nerve. The sixth cranial nerve, also called the abducens, controls blinking and back-and-forth eye movement and is the second most commonly affected cranial nerve in Möebius syndrome. Additional cranial nerves affected in some patients control other eye movements and other functions such as hearing, balance, speech, and feeding.
Individuals with Möebius syndrome may also have abnormalities of their limbs, chest muscles, and tongue. The chance of mental retardation appears to be increased in people with Möebius syndrome, but most people with the disorder have normal intelligence.
Genetic profile
Most cases of Möebius syndrome are isolated and do not appear to be genetic, but occurrence in multiple individuals within some families indicates that there are multiple genetic forms. One study in 1991 suggested that forms of Möebius syndrome which included abnormalities of the limbs and skeleton were less likely than other types to be genetic. During pregnancy, certain exposures, such as to the drug misoprostol, appear to increase the risk of Möebius syndrome.
K E Y T E R M S
Balanced chromosome translocation—A rearrangement of the chromosomes in which two chromosomes have broken and exchanged pieces without the loss of genetic material.
Cranial nerves—The twelve nerves that originate in the brain, and control functions such as hearing, vision and facial expression.
Chromosomes 13, 3, and 10 appear to contain genes causing forms of Möebius syndrome, now named, respectively, types 1, 2, and 3. The presence of a gene on chromosome 13 was first suggested based on a family in which several members had facial weakness and finger abnormalities along with a chromosome rearrangement called a balanced translocation involving chromosomes 1 and 13. In a balanced translocation, two chromosomes have broken and exchanged pieces. Balanced translocations are usually not associated with physical abnormalities unless (1) material has been lost or gained during the breaks, or (2) a gene is disrupted by one of the breaks. When a child with Möebius syndrome in an unrelated family was found to have a deletion (missing piece) of chromosome 13 in the same area as the break in the first family, this suggested that there might be a gene causing Möebius syndrome on chromosome 13 rather than on 1.
The genes on chromosomes 3 and 10 were localized using a technique called linkage mapping, which involves using molecular genetics and statistical methods to look throughout all of the chromosomes in families with several affected members for areas associated with the disease. As of 2001, the actual genes on chromosomes 3, 10, and 13 have not been identified. These three forms of the disease are inherited in an autosomal dominant manner, which means that only one altered copy of the gene is required to have the disease, and people with the disease have a 50% chance of having an affected child with each pregnancy. However, in the chromosome 3 and 10 families, some individuals who appear to carry a gene do not show signs of Möebius syndrome, suggesting that factors other than genetics, such as uterine environment, are involved even in these highly familial cases.
One family was reported in which two brothers and their male cousin who were the sons of sisters all had Möebius syndrome along with other physical abnormalities and mental retardation. Boys only have one X chromosome and can inherit an X-linked disease from their unaffected mothers, who have two X chromosomes. The
syndrome Möebius
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
747 |

Moyamoya
pattern of affected children in this family is therefore typical of X-linked inheritance, so it is suggested that there may be a gene involved in Möebius syndrome on the X chromosome as well. If this is the case, the son of a woman with an altered Möebius gene on one X-chromo- some would have a 50% chance of inheriting the gene and having the condition. A man with this type of Möebius syndrome would be unlikely to have affected children since his daughters would likely have one normal X chromosome from their mother and his sons would not receive his X chromosome but his Y chromosome. In another family, a brother and sister with unaffected parents had Möebius syndrome, suggesting autosomal recessive inheritance, in which two altered copies of a gene are required to have the disorder. In an autosomal recessive disorder, a couple in which each parents carry one altered copy of the disease gene have a 25% chance of having a child with the condition with each pregnancy.
Demographics
Möebius syndrome is extremely rare and does not seem to affect any particular ethnic group more than others. The families in which genes on chromosomes 3 and 10 were mapped were Dutch.
Signs and symptoms
The first sign of Möebius syndrome in newborns is an inability to suck, sometimes accompanied by excessive drooling and crossed eyes. Also seen at birth in some patients are abnormalities of the limbs, tongue, and jaw. Children also often have low muscle tone, particularly in the upper body. The lack of facial expression and inability to smile become apparent as children get older.
When cranial nerve palsy is associated with limb reduction abnormalities and the absence of the pectoralis muscles, the condition is known as Poland-Möebius or Möebius-Poland syndrome. Common limb abnormalities are missing or webbed fingers and clubfoot.
The prevalence of mental retardation in Möebius syndrome is uncertain. It has been estimated in the past to be between 10% and 50%, but these numbers are thought to be overestimates resulting from the lack of facial expression and drooling seen in people with Möebius syndrome. In one study of familial cases of Möebius syndrome, 3% were reported to be mentally retarded.
Diagnosis
Diagnosis of Möebius syndrome is made on the basis of clinical symptoms, especially the lack of facial
expression. Since exact genes involved in Möebius syndrome have not yet been identified as of 2001, molecular genetic testing is not available at this time.
Treatment and management
The ability to smile has been restored in some cases of Möebius syndrome by surgery which transfers nerve and muscle from the thigh to the face. Other surgeries can be used to treat eye, limb, and jaw problems. In children with feeding problems, special bottles or feeding tubes are used. Physical and speech therapy are used when necessary to improve control over coordination, speech, and eating.
Prognosis
Möebius syndrome does not appear to affect life span, and individuals who are treated for their symptoms can lead normal lives.
Resources
PERIODICALS
Kumar, Dhavendra. “Möebius Syndrome.” Journal of Medical
Genetics 27 (1990): 122–26.
ORGANIZATIONS
Möebius syndrome Foundation (MSF). PO Box 993, Larchmont, NY 10538. (914)834-6008. http://www
.ciaccess.com/moebius .
Toni I. Pollin, MS, CGC
Mohr syndrome see Oral-facial-digital syndrome (OFD)
Morquio syndrome (MPS IV) see
Mucopolysaccharidosis (MPS)
I Moyamoya
Definition
Moyamoya is a progressive syndrome characterized by narrowing of the blood vessels in the brain. Moyamoya is the Japanese term for ‘cloud of smoke drifting in the air.’
Description
The term moyamoya is used to describe how the arteries in the brain look in this syndrome, which was
748 |
G A L E E N C Y C L O P E D I A O F G E N E T I C D I S O R D E R S |
