
- •Contents
- •1. Fundamentals of Pathology
- •4. Tissue Repair
- •5. Circulatory Pathology
- •8. Amyloidosis
- •13. Vascular Pathology
- •16. Renal Pathology
- •17. Gastrointestinal Tract Pathology
- •18. Pancreatic Pathology
- •21. Central Nervous System Pathology
- •23. Female Genital Pathology
- •24. Breast Pathology
- •25. Male Pathology
- •26. Endocrine Pathology
- •27. Bone Pathology
- •28. Joint Pathology
Male Pathology 25
PENIS
1.Malformations ofthepenis. Epispadias refers to a urethral opening on the dorsal surface of the penis, while hypospadias refers to a urethral opening on the ventral surface. Both malformations may be associated with unde scended testes, and both have an increased risk of urinary tract infections (UTis) and infertility.
2.Balanitis/balanoposthitis is the term used for inflammation of the glans penis. Causes include poor hygiene and lack of circumcision.
3.Peyronie disease is penile fibromatosis resulting in curvature of the penis.
4.Condyloma acuminatum causes warty, cauliflower-like growth, with the causative agents most frequently being Human papilloma virus (HPV) serotypes 6 and 11.
5. Squamous cell carcinoma (SCC) is uncommon in the United States, and is often related to infection with Human papilloma virus (HPV) serotypes 16 and 18. There is an increased risk in uncircumcised males. Precursor lesions include Bowen disease, bowenoid papulosis, and erythroplasia of Queyrat (may be regarded as synonymous with penile Bowen disease or as representative of one end of a spectrum of in situ penile carcinoma).
6.Priapismis a persistent painful erection that can be caused by sickle cell ane mia (causes blood sludging in penis), trauma, and drugs (e.g., trazodone).
7.Erectile dysfunction. Causes of impotence include psychological factors, decreased testosterone, vascular insufficiency (most common cause over age 50), neurologic disease (multiple sclerosis, diabetic neuropathy, radical prostatectomy), some medications (leuprolide, methyldopa, psychotropic medications), hypothyroidism, prolactinoma, and penile disorders.
TESTES
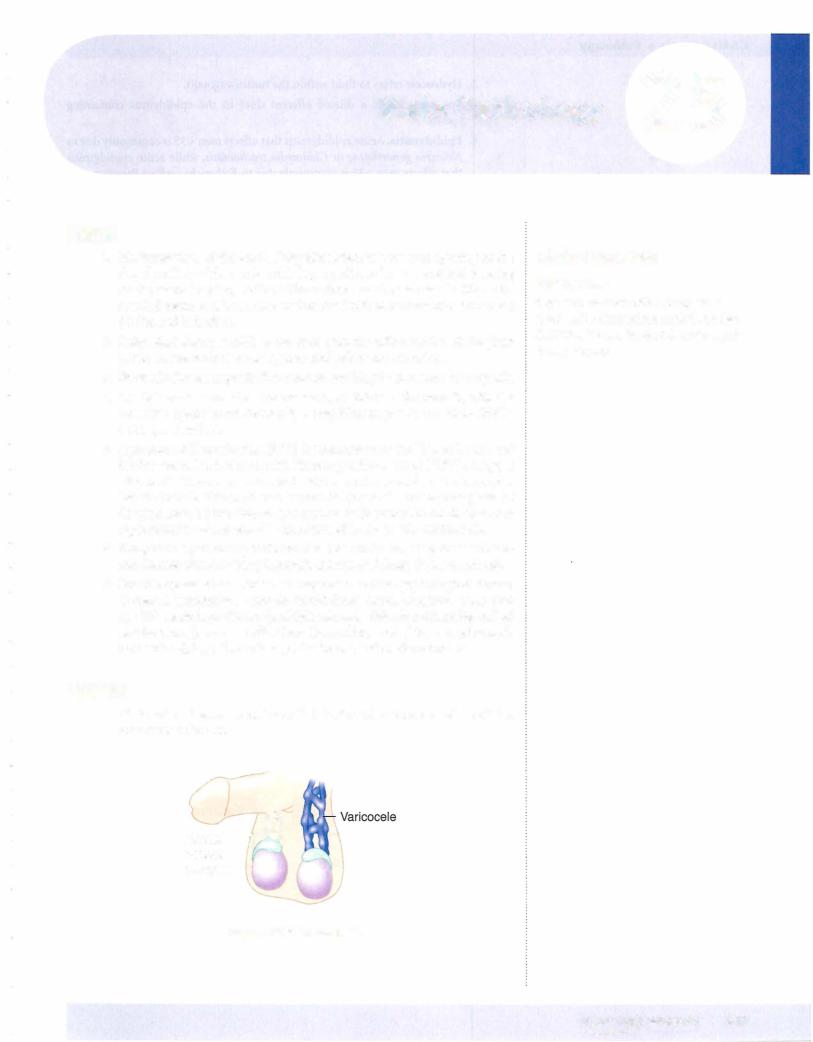
1. Varicocele is the term used for a dilated vein within the spermatic cord that may cause infertility.
Normal - venous
complex
Clinical Correlate
Hypospadias
Boys who are born with hypospadias must not be circumcised at birth, so that their foreskin can be used later for repair during surgery.
Figure 25-1 . Varicocele
MEDICAL 247
Chapter 25 • Male Pathology
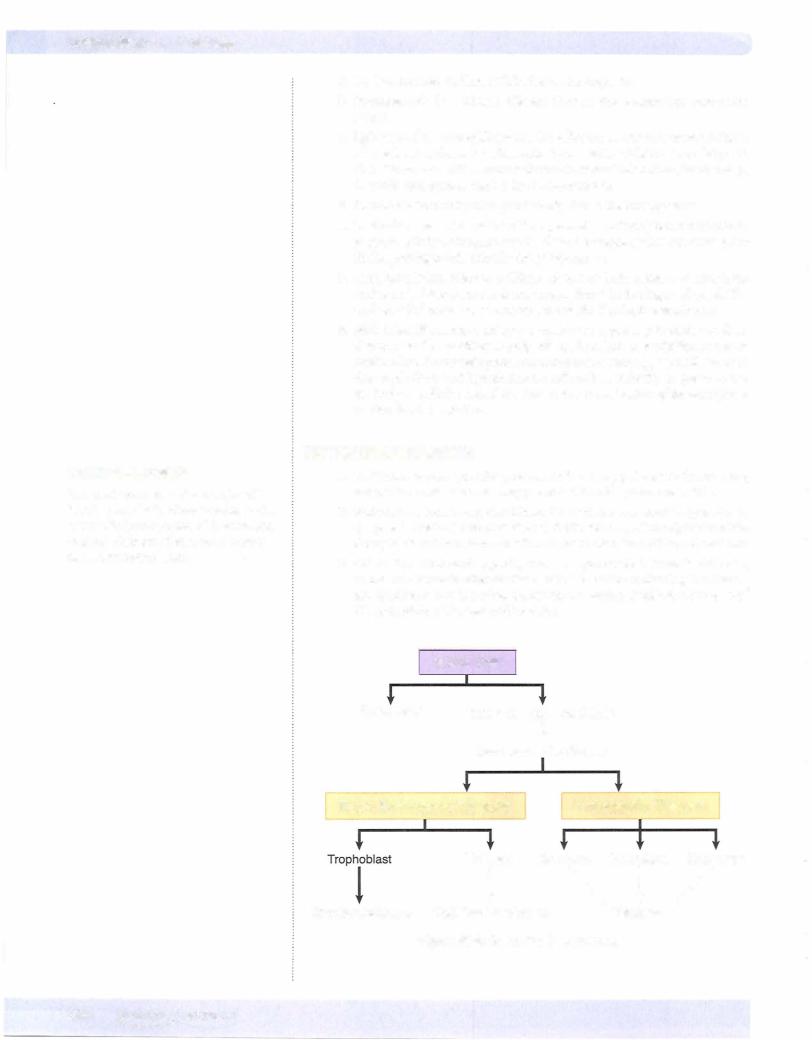
Table 25-1. SeminomasVersus Nonseminomatous Germ-CellTumors
Seminomas |
Nonseminomatous Germ-Cell Tumors |
Seminoma |
Embryonal, yolksac, choriocarcinoma, teratoma |
Radiosensitive |
Not radiosensitive |
Chemosensitive |
Chemosensitive |
Late metastasis |
Early metastases to retroperitoneal lymph nodes |
Excellent prognosis |
More aggressive |
4. Germ-cell tumors
a. Seminoma is the most common germ-cell tumor in adults ages 15-35. It is characteristically sensitive to both chemotherapy and radiation, and has an excellent prognosis, with early stage seminoma having a 95% cure rate. A variant is spermatocytic seminoma, a disease of older men, also with an excellent prognosis.
1. Pathology. On gross examination, the tumor forms large, grey-tan, bulky masses. Microscopic examination shows polygonal germ cells with clear cytoplasm and round nuclei that are arranged in lobules separated by fibrous septae. Lymphocytes, granulomas, and giant cells may be seen. The tumor marker for seminoma is placental alka line phosphatase (PLAP).
b. Embryonal carcinoma is more aggressive than seminoma and affects adults ages 20-40. The tumor causes bulkymasses with hemorrhage and necrosis that microscopically show large primitive cells. Tumor markers for embryonal carcinoma are nonspecific, but there may be elevation of alpha-fetoprotein (AFP) and/or beta human chorionic gonadotropin ( -hCG).
c. Choriocarcinoma is a highly malignant tumor that often has wide spread metastasis at the time of diagnosis; hematogenous spread to lungs and liver is particularly common. The tumor often has small pri maries with extensive hemorrhage and necrosis, which microscopically shows proliferation of syncytiotrophoblasts and cytotrophoblasts. The tumor marker is -hCG.
d. Yolksactumor (endodermal sinus tumor) is the most common germ cell tumor in children. In those cases, the prognosis is good. In adults, the tumor is often mixed with other components so the prognosis may depend on what the other components are.
i. Microscopically,yolk sac tumor shows scattered Schiller-Duval bod ies, which have a mesodermal core with a central capillary, all lined by flattened layers of both visceral and parietal cells resembling a glomerulus-like structure. The tumor marker is alpha-fetoprotein
(AFP).
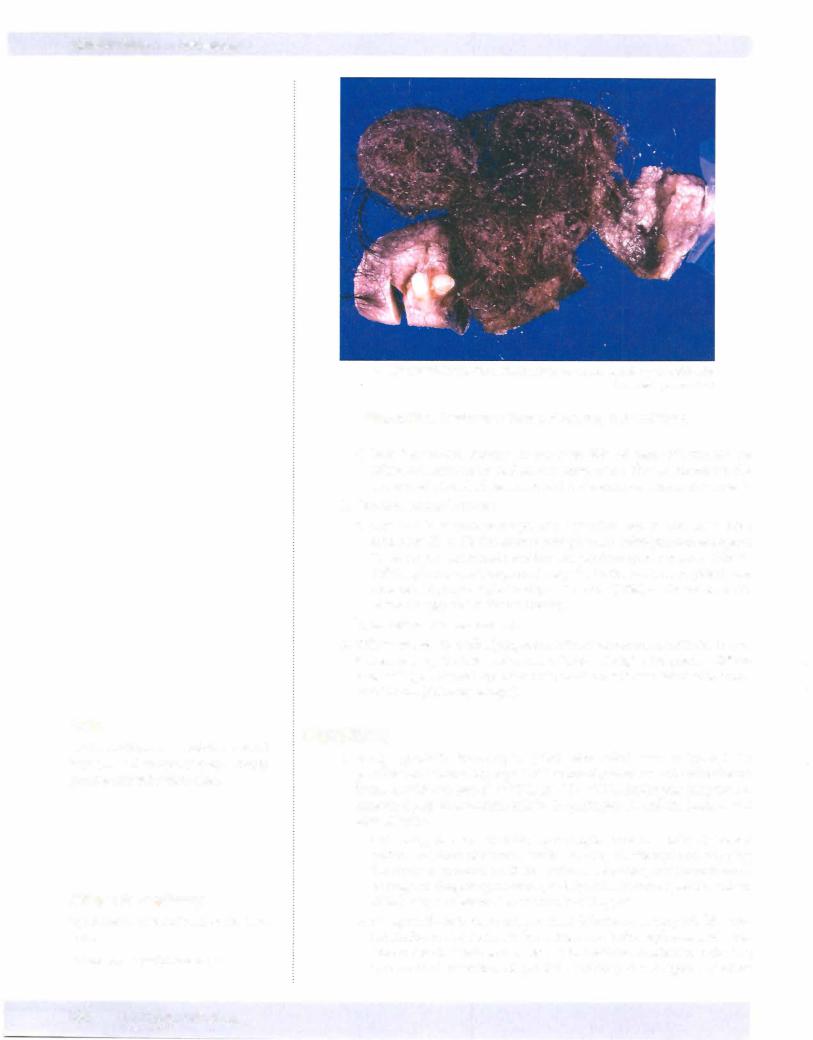
e. Teratoma often causes cystic masses that may contain cartilage and bone. The majority (99%) of these tumors, when located in testes, are malignant. Microscopically, teratoma contains ectodermal, endodermal, and mesodermal tissue in a haphazard arrangement. Immature elements and malignant transformation are often seen.
MEDICAL 249
USMLE Step 1 • Pathology
Note
The H in BPH more accurately represents hyperplasia than hypertrophy, although you may see eitherterm used.
Bridge to Anatomy
Hyperplasia --7 transitional/periurethral zones
Carcinoma --7 peripheral zone
250 MEDICAL
@ Katsumi M. Miyai, M.D., Ph.D.; Regents ofthe University ofCalifornia. Used with permission.
Figure 25-3. Teratoma of Testes, Producing Hair and Teeth
f.Mixed germ-cell tumors. As many as 60% of germ-cell tumors are mixed and contain more than one component. Teratocarcinoma is the name used when both teratoma and embryonal carcinoma are present.
5.Sex cord-stromal tumors
a.Leydig cell tumors cause painless testicular masses, and may affect adults age 20 to 60. The tumors may produce androgens and estrogens; in adults, the hormonal secretion can produce gynecomastia, while in children, it mayproduce precocious puberty. Benign tumors (90%) have an excellent prognosis, but malignant tumors (10%) can be refractory to chemotherapy and radiation therapy.
b.Sertoli cell tumors are rare.
6.Othertumors. Testicular lymphoma is the most common testicular tumor in men over age 50. It is most commonlynon-Hodgkin lymphoma, diffuse large-cell type. Scrotal squamous cell carcinoma is associated with expo sure to soot (chimney sweeps).
PROSTATE
1. Benign prostatic hypertrophy (BPH, also called nodular hyperplasia; glandularand stromal hyperplasia)= isextremely= common and the incidence increases with age (age 60 70%, age 70 80%). Androgens (dihydrotes tosterone) play an important role in the pathogenesis, and the lesion is not premalignant.
a.Clinically, benign prostatic hypertrophy presents with decreased caliber and force ofstream; trouble starting (hesitancy) and stopping the stream; postvoid dribbling, urinary retention, and incontinence; or urgency, frequency, nocturia, and dysuria. Prostate specific antigen (PSA) maybe elevated but is usually <10 ng/ml.
b.Complications include urinary tract infections, urinary bladder tra beculation and diverticula formation, and hydronephrosis and renal failure (rare). Treatment varies, with available modalities including transurethral resection of prostate (TURP); the 5-alpha reductase
Chapter 25 • Male Pathology
inhibitor, finasteride (Proscar), and the selective alpaha- 1 receptor blockers, terazosin and prazosin.
c. Pathology. Grossly, benign prostatic hypertrophy causes an enlarged prostate with well-demarcated nodules in the transition and central (periurethral zones), which often results in slitlike compression of the prostatic urethra. Microscopically, the lesion shows glandular and stro mal hyperplasia resulting in the characteristic prostate enlargement.
is the most common cancer in men in the United States and is the second most common cause of cancer death in men. The incidence increases with age, and the highest rate is in African Americans.
a. Clinical features. Prostate adenocarcinoma is often clinically silent, but may present with lower back pain secondary to metastasis. Advanced localized disease may present with urinary tract obstruction or UTis (uncommon) . The tumor can be detected with digital rectal exam (induration), serum prostatic specific antigen (PSA) levels, and tran srectal ultrasound and biopsy.
i. Metastases most commonly involve the obturator and pelvic lymph nodes. Osteoblastic bone metastasis to the lumbar spine can occur, and be associated with elevated alkaline phosphatase. Treatment of local disease is with prostatectomy and/or external beam radiation. Metastatic disease is treated with orchiectomy, estrogens, or andro gen receptor blockade (flutamide or leuprolide). The disease course can be monitored with PSA levels.
b. Pathology. Prostate adenocarcinoma causes an ill-defined, firm, yellow mass that commonly arises in the posterior aspect of the peripheral zone. Microscopically, adenocarcinoma is seen, which is graded with the Gleason system.
3.Prostatitis.Acute prostatitis is usually due to intraprostatic reflux of urine
containing Escherichia, Pseudomonas, or Klebsiella pathogens. Chronic
prostatitis may develop following recurrent acute prostatitis, and bacte rial pathogens may not be detectable. Clinical findings can include fever (acute prostatitis), pain (lower back, perineal, or suprapubic), painful prostate on rectal exam, and dysuria (sometimes with hematuria) .
Clinical Correlate
An elderly man with osteoblastic metastasis visible on x-ray should be considered as having prostate carcinoma until proven otherwise.
MEDICAL 251
USMLE Step 1 • Pathology
Chapter Summary
•Malformations of the penis related to aberrant opening of the urethra include epispadias (opening on dorsal surface) and hypospadias (opening on ventral surface). Balanitis is inflammation ofthe glans penis, often related to poor hygiene and lack of circumcision. Peyronie disease is penile fibromatosis resulting in curvature ofthe penis. Condyloma acuminatum is a warty growth related to HPV infection. Squamous cell carcinoma of the penis is uncommon in the United States butcan be related to HPV infection. Priapism is a persistent painful erection. Erectile dysfunction has many causes.
•Varicocele is a dilated vein within the spermatic cord. Hydrocele is fluid within the tunica vaginalis. Spermatocele is a dilated efferent duct in the epididymis containing sperm.
•Acute epididymitis is usually caused by Neisseria gonorrhoeae and/or Chlamydia trachomatis. Chronic epididymitis is usually caused by tuberculosis. Orchitis or testicular inflammation can be caused by mumps.
•Testicular torsion is a twisting ofthe spermatic cord that maycause painful hemorrhagic infarction leadingto gangrene.
•Testicular cancers tend to cause firm, painless masses, and occur in a wide variety of subtypes. Seminoma is a chemotherapyand radiation therapy sensitive cancer ofyoung adult men that causes bulkytesticular masses.
Spermatocytic seminoma is a variant affecting older men. Cryptorchidism is a failure of descent of one or both testes, and is associated with an increased risk of developing seminoma. Male infertility has many causes.
•Embryonal carcinoma also affects young men and behaves more aggressively than seminoma. Choriocarcinoma is a highly malignant testicular carcinoma. Yolk sac tumor is the most common germ-cell tumor in children, in whom it has a better prognosis than in adults. Teratoma in testes (as opposed to in ovaries) is almost always malignant and aggressive. Mixed germ-cell tumors are common and usually behave aggressively.
•Most sex cord tumors ofthe testes are Leydig cell tumors, ofwhich 10% are malignant. Testicular lymphoma is the most common testicular tumor in men over age 50 years.
•Benign prostatic hypertrophy (nodular hyperplasia) is an extremely common condition ofolder men that may alterthe function ofthe urinary tract by compressing the urethra.
•Prostate cancer is the most common cancer in men in the United States and commonly arises in the posterior aspect ofthe peripheral zone ofthe prostate. It is often clinically silent, but may be detected by digital rectal exam, serum PSA levels, and transrectal ultrasound and biopsy.
•Prostatitis can be acute or chronic, and causes tenderness of the prostate on rectal examination.
252 MEDICAL
