
новая папка / 80
.pdf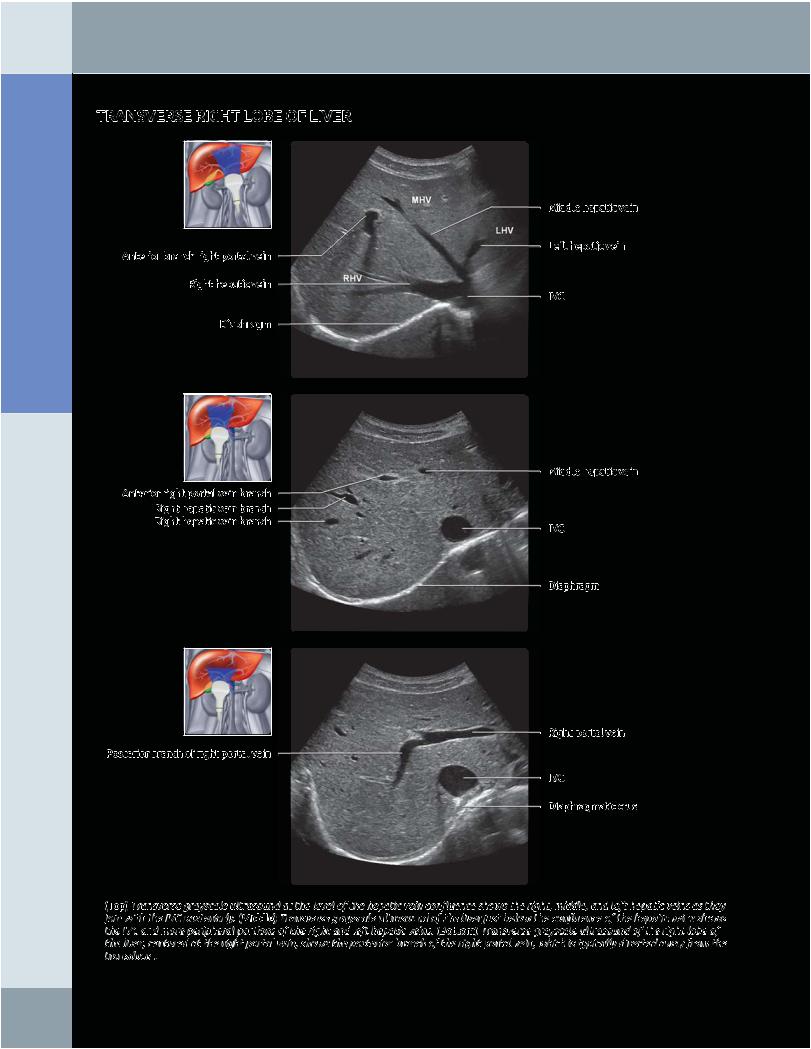
Anatomy: Abdomen
Liver
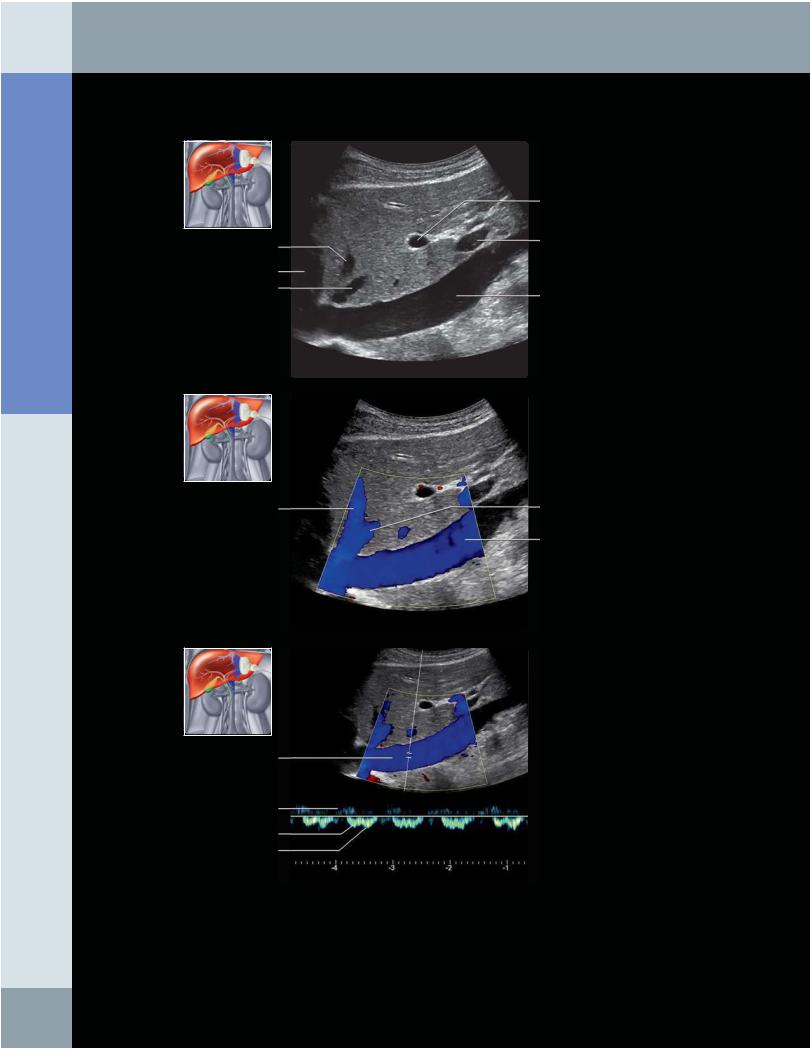
TRANSVERSE RIGHT LOBE OF LIVER
Anterior branch right portal vein
Right hepatic vein
Diaphragm
Anterior right portal vein branch
Right hepatic vein branch
Right hepatic vein branch
Posterior branch of right portal vein
Middle hepatic vein
Left hepatic vein
IVC
Middle hepatic vein
IVC
Diaphragm
Right portal vein
IVC
Diaphragmatic crus
(Top) Transverse grayscale ultrasound at the level of the hepatic vein confluence shows the right, middle, and left hepatic veins as they join with the IVC posteriorly. (Middle) Transverse grayscale ultrasound of the liver just below the confluence of the hepatic veins shows the IVC and more peripheral portions of the right and left hepatic veins. (Bottom) Transverse grayscale ultrasound of the right lobe of the liver, centered at the right portal vein, shows the posterior branch of the right portal vein, which is typically directed away from the transducer.
14
Liver
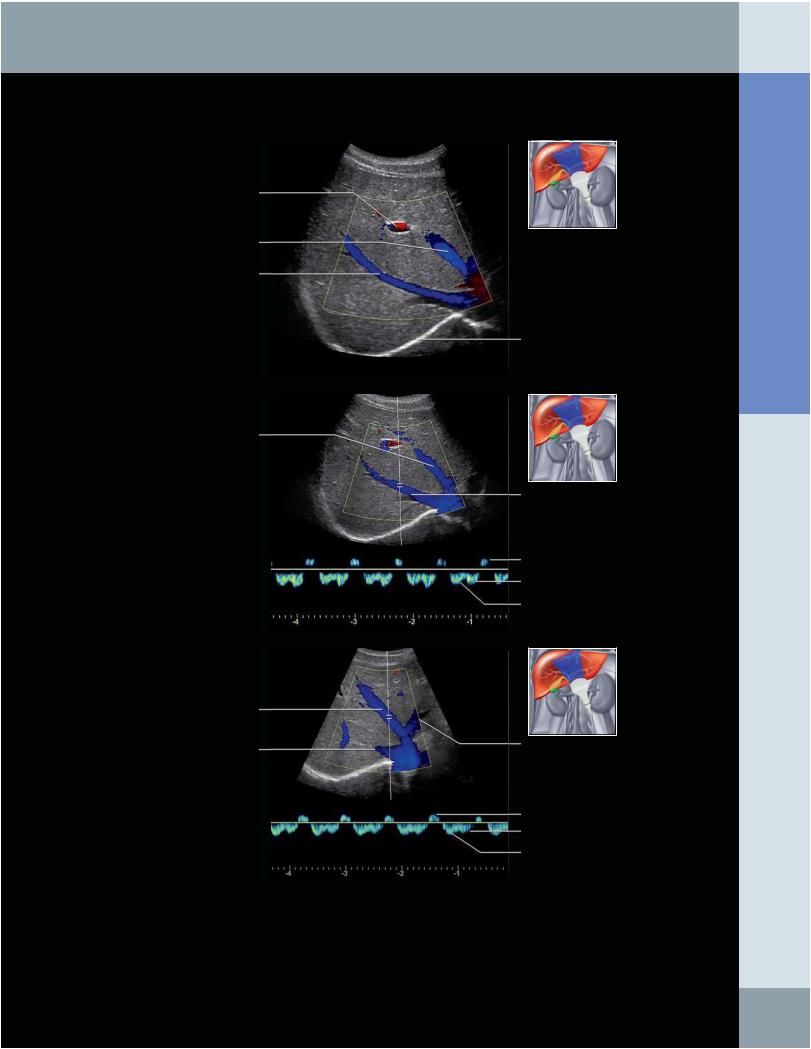
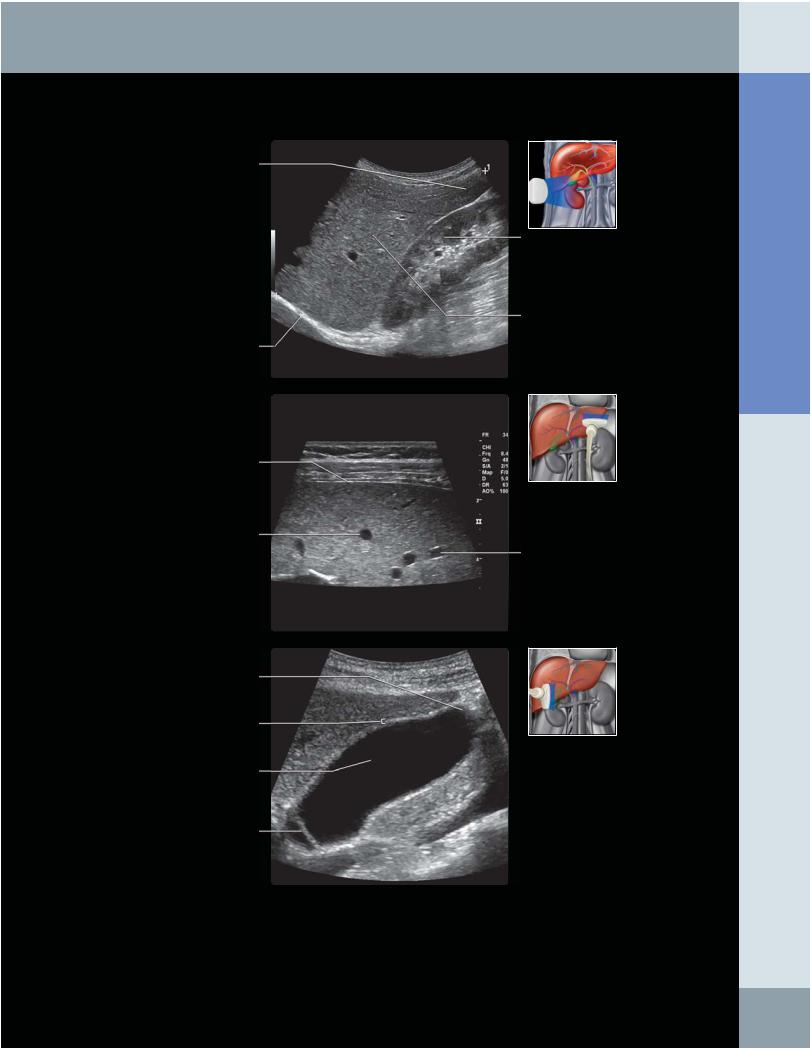
RIGHT LOBE OF LIVER: RIGHT HEPATIC VEIN
Anterior right portal vein
Middle hepatic vein
Right hepatic vein
Middle hepatic vein
Middle hepatic vein
Right hepatic vein
Diaphragm
Right hepatic vein
A wave
D wave
S wave
Left hepatic vein
A wave
D wave
S wave
(Top) Transverse color Doppler ultrasound of the right lobe of the liver shows that the right and middle hepatic vein are directed away from the transducer and flowing toward the IVC. (Middle) Spectral tracing of the right hepatic vein shows a typical triphasic waveform with A, S, and D waves representing reflection of cardiac motion in the hepatic veins. (Bottom) Spectral tracing of the middle hepatic vein shows a typical triphasic waveform with A, S, and D waves representing reflection of cardiac motion in the hepatic veins.
Abdomen Anatomy:
15
Anatomy: Abdomen
Liver
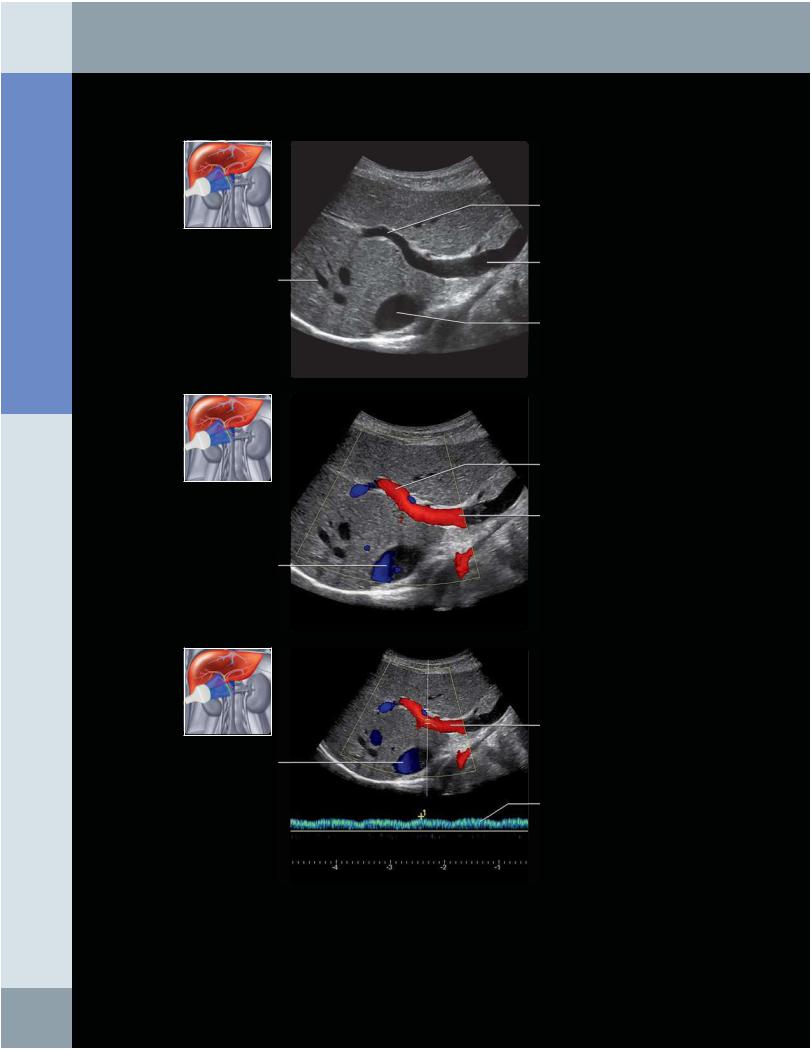
MAIN PORTAL VEIN
Right portal vein
Main portal vein
Hepatic vein branch
IVC
Right portal vein
Main portal vein
IVC
Main portal vein
IVC
Main portal vein spectral tracing
(Top) Longitudinal oblique grayscale ultrasound is shown, centered at the level of the main portal and right portal vein. (Middle) Longitudinal oblique color Doppler ultrasound, centered at the level of the main portal and right portal vein, shows that flow in the portal vein is directed toward the liver (hepatopetal). (Bottom) Longitudinal oblique spectral Doppler ultrasound of the main portal vein shows that the flow is hepatopetal, with gentle undulation reflecting the cardiac and respiratory cycle.
16
Liver
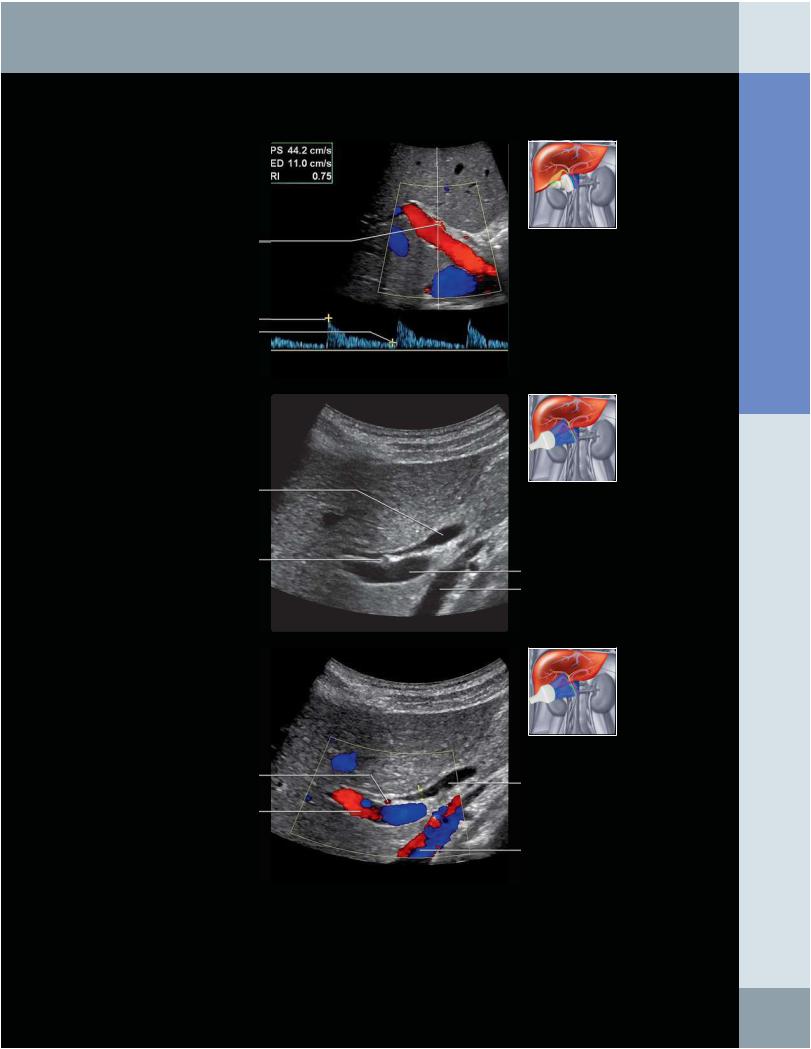
PORTA HEPATIS
Hepatic artery
Systolic peak
End diastole
Common bile duct
Right hepatic artery
Right hepatic artery
Main portal vein
Main portal vein IVC
Common bile duct
IVC
(Top) Longitudinal oblique spectral tracing of the main hepatic artery shows a typical low-resistance waveform, with brisk upstroke and forward diastolic flow. In this case, the hepatic artery velocity is 44 cm/s, which is normal. When measuring velocity, proper angle correction is the key to obtaining accurate velocities. (Middle) Oblique grayscale ultrasound of the liver, centered at the porta hepatis, shows the common bile duct anterior to the right hepatic artery and portal vein. The IVC is seen posterior to the portal vein. (Bottom) Oblique color Doppler ultrasound of the liver, centered at the porta hepatis, shows the common bile duct is anterior to the portal vein and the right hepatic artery is between these 2 structures. This is the typical anatomy in this location, although anatomic variants of the right hepatic artery may occur in which the hepatic artery may be located anterior to the common bile duct.
Abdomen Anatomy:
17
Anatomy: Abdomen
Liver
LONGITUDINAL LIVER
Middle hepatic vein
Heart Left hepatic vein
Middle hepatic vein
IVC
A wave
S wave
D wave
Left portal vein
Main portal vein
IVC
Left hepatic vein
IVC
(Top) Longitudinal grayscale ultrasound of the right lobe of the liver is shown, centered at the level of the IVC. (Middle) Longitudinal color Doppler ultrasound of the liver is shown at the level of the IVC. (Bottom) Spectral tracing of the IVC shows a typical triphasic waveform with A, S, and D waves representing reflection of cardiac motion in the IVC.
18
Liver
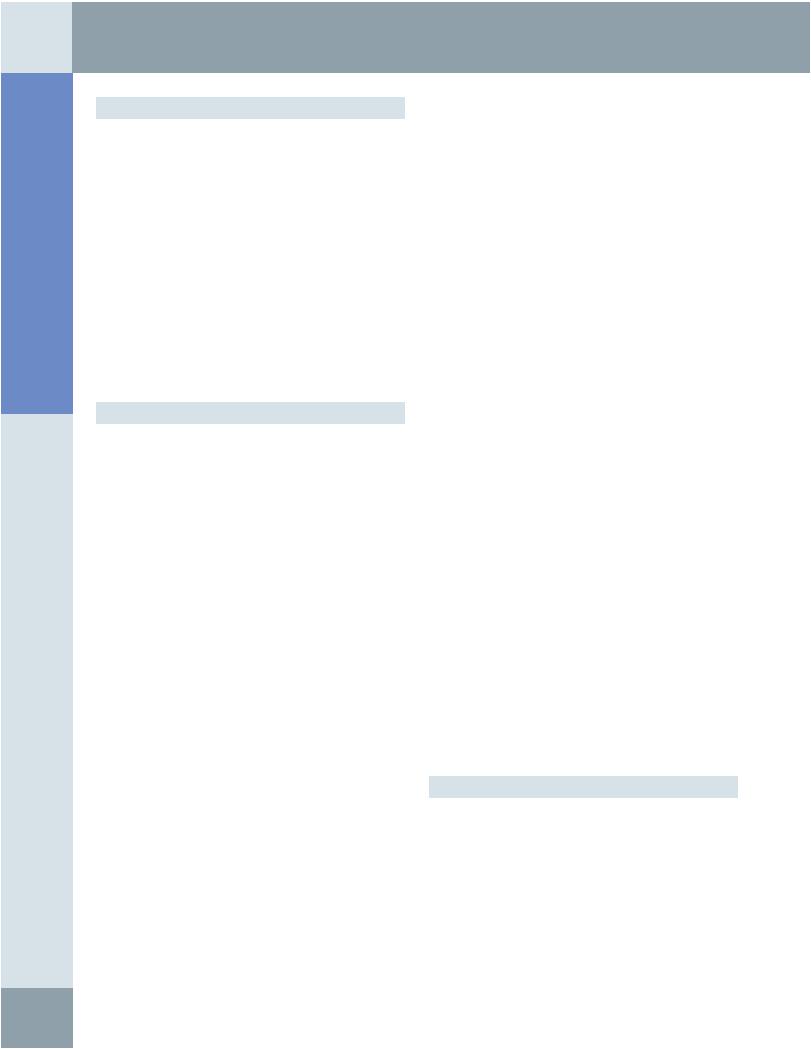
OTHER VIEWS OF LIVER
Inferior liver margin
Diaphragm
Right kidney
Right lobe of liver
Liver capsule
Hepatic vein branch
Portal vein branch
Gallbladder fundus
Gallbladder wall
Gallbladder lumen
Gallbladder wall fold
(Top) Longitudinal grayscale ultrasound of the right lobe of the liver shows the liver ends just above the inferior margin of the right kidney. Normal hepatic length should be < 15-15.5 cm. Notice that the normal hepatic parenchyma is slightly hyperechoic compared to the normal kidney. (Middle) Transverse high-resolution ultrasound of the liver capsule, as seen here, is typically obtained with higher frequencies (7-9 MHz). Subtle nodularity of the capsule and small subcapsular liver lesions that may not be as well visualized with standard (3-5 MHz) frequencies are best visualized with this view. Note the hepatic veins have no discernible wall, whereas the portal veins have slightly echogenic walls. (Bottom) Longitudinal oblique ultrasound shows a normal gallbladder with anechoic fluid within the lumen and normal appearance of the gallbladder wall. Normal gallbladder wall thickness should be measured at the interface with the liver and should be less than 3 mm in thickness. A fold in the gallbladder neck is incidentally seen in this patient.
Abdomen Anatomy:
19
Anatomy: Abdomen
Biliary System
TERMINOLOGY
Abbreviations
•Extrahepatic biliary structures
○Gallbladder (GB)
○Cystic duct (CD)
○Right hepatic (RH) and left hepatic (LH) ducts
○Common hepatic duct (CHD)
○Common bile duct (CBD)
Definitions
•Proximal/distal biliary tree
○Proximal refers to portion of biliary tree that is in closer in proximity to liver andhepatocytes
○Distal refers to caudal end closer to ampulla and bowel
•Central/peripheral
○Central refers to biliary ducts close to porta hepatis
○Peripheral refers to higher-order branches of intrahepatic biliary tree extending into hepatic parenchyma
IMAGING ANATOMY
Overview
•Biliary ducts carry bile from liver to duodenum
○Bile is produced continuously by liver, stored and concentrated by GB, and released intermittently by GB contraction in response to presence of fat in duodenum
○Hepatocytes form bile → bile canaliculi → interlobular biliary ducts → collecting bile ducts → right and left hepatic ducts → common hepatic duct → common bile duct → intestines
•Common bile duct forms in free edge of lesser omentum by union of cystic duct and common hepatic duct
○Length of duct: 5-15 cm, depending on point of junction of cystic and common hepatic ducts
○Descends posterior and medial to duodenum, lying on dorsal surface of pancreatic head
○Joins with pancreatic duct to form hepaticopancreatic ampulla of Vater
○Ampulla opens into duodenum through major duodenal (hepaticopancreatic) papilla
○Distal common bile duct is thickened into sphincter of Boyden and hepaticopancreatic segment is thickened into a sphincter of Oddi
–Contraction of these sphincters prevents bile from entering duodenum; forces it to collect in GB
–Relaxation of sphincters in response to parasympathetic stimulation and cholecystokinin (released by duodenum in response to fatty meal)
•Vessels, nerves, and lymphatics
○Arteries
–Hepatic arteries supply intrahepatic ducts
–Cystic artery supplies proximal common duct
–RH artery supplies middle part of common duct
–Gastroduodenal and pancreaticoduodenal arcade supply distal common duct
–Cystic artery supplies GB (usually from right hepatic artery; variable)
○Veins
–From intrahepaticducts → hepatic veins
–From common duct → portal vein (in tributaries)
–From GB directly into liver sinusoids, bypassing portal vein
○Nerves
–Sensory: Right phrenic nerve
–Parasympathetic and sympathetic: Celiac ganglion and plexus; contraction of GB and relaxation of biliary sphincters is caused by parasympathetic stimulation, but more important stimulus is from hormone cholecystokinin
○Lymphatics
–Same course and name as arterial branches
–Collect at celiac lymph nodes and node of omental foramen
–Nodes draining GB are prominent in porta hepatis and around pancreatic head
•Gallbladder
○~ 7-10 cm long, holds up to 50 mL of bile
○Lies in shallow fossa on visceral surface of liver
○Vertical plane through GB fossa and middle hepatic vein divides left and right hepatic lobes
○May touch and indent duodenum
○Fundus is covered with peritoneum and relatively mobile; body and neck attached to liver and covered by hepatic capsule
○Fundus: Wide tip of GB, projects below liver edge (usually)
○Body: Contacts liver, duodenum, and transverse colon
○Neck: Narrowed, tapered, and tortuous; joins cystic duct
○Cystic duct: 3-4 cm long, connects GB to common hepatic duct; marked by spiral folds of Heister; helps to regulate bile flow to and from GB
•Normal measurement limits of bile ducts
○CBD/CHD
–< 6-7 mm in patients without history of biliary disease in most studies
–Controversy about dilatation related to previous cholecystectomy and old age
○Intrahepatic ducts
–Normal diameter of 1st and higher-order branches < 2 mm or < 40% of diameter of adjacent portal vein
–1st (i.e., LH duct and RH duct) and 2nd-order branches are normally visualized
–Visualization of 3rd and higher-order branches is often abnormal and indicates dilatation
ANATOMY IMAGING ISSUES
Imaging Recommendations
•Patient should fast for at least 4 hours prior to US examination to ensure GB is not contracted after a meal, ideally fasting for 8-12 hours (overnight)
•Complete assessment includes scanning liver, porta hepatis region, and pancreas in sagittal, transverse, and oblique views
•Subcostal and right intercostal transverse views help align bile ducts and GB along imaging plane for optimal visualization
•Usually structures are better assessed and imaged with patient in full suspended inspiration and in left lateral oblique position
20
Biliary System
•Harmonic imaging provides improved contrast between bile ducts and adjacent tissues, leading to improved visualization of bile ducts, luminal content, and wall
•For imaging of gallstone disease, special maneuvers are recommended
○Move patient from supine to left lateral decubitus position
–Demonstrates mobility of gallstones
–Gravitates small gallstones together to appreciate posterior acoustic shadowing
○Set focal zone at level of posterior acoustic shadowing
–Maximizes effect of posterior acoustic shadowing
Imaging Approaches
•Transabdominal ultrasound is ideal initial investigation for suspected biliary tree or GB pathology
○Cystic nature of bile ducts and GB (especially if these are dilated) provides inherently high-contrast resolution
○Acoustic window provided by liver and modern state of the art ultrasound technology provides good spatial resolution
○Common indications of US for biliary and GB disease include
–Right upper quadrant/epigastric pain
–Abnormal liver function test or jaundice
–Suspected gallstone disease
–Pancreatitis
○US plays key role in multimodality evaluation of complex biliary problems
•Supplemented by various imaging modalities including MR/MRCP and CT
Imaging Pitfalls
•Common pitfalls in evaluation of GB
○Posterior shadowing may arise from GB neck, Heister valves of CD, or adjacent gas-filled bowel loops
–Mimics cholelithiasis
–Scan after repositioning patient in prone or left lateral decubitus positions
○Food material within gastric antrum/duodenum
–Mimics GB filled with gallstones or GB containing milk of calcium
–During real-time scanning, carefully evaluate peristaltic activity of involved bowel with oral administration of water
•Common pitfalls in US evaluation of biliary tree
○Redundancy, elongation, or folding of GB neck on itself
–Mimics dilatation of CHD or proximal CBD
–Avoided by scanning patient in full suspended inspiration
–Careful real-time scanning allows separate visualization of CHD/CBD medial to GB neck
○Presence of gas-filled bowel loops adjacent to distal extrahepatic bile ducts
–Obscure distal biliary tree and render detection of choledocholithiasis difficult
–Scan with patient in decubitus positions or after oral intake of water
○Gas/particulate material in adjacent duodenum and pancreatic calcification
–Mimic choledocholithiasis within CBD
○Presence of gas within biliary tree
–May mimic choledocholithiasis, differentiated by presence of reverberation artifacts
–Limits US detection of biliary calculus
Key Concepts
•Direct venous drainage of GB into liver bypasses portal venous system, often results in sparing of adjacent liver from generalized steatosis (fatty liver)
•Nodal metastasis from GB carcinoma to peripancreatic nodes may simulate a primary pancreatic tumor
•Sonography: Optimal means of evaluating GB for stones and inflammation (acute cholecystitis); best done in fasting state (distends GB)
•Intrahepatic bile ducts follow branching pattern of portal veins
○Usually lie immediately anterior to portal vein branch; confluence of hepatic ducts just anterior to bifurcation of right and main portal veins
CLINICAL IMPLICATIONS
Clinical Importance
•In patients with obstructive jaundice, US plays key role
○Differentiates biliary obstruction from liver parenchymal disease
○Determines presence, level, and cause of biliary obstruction
•Common variations of biliary arterial and ductal anatomy result in challenges to avoid injury at surgery
○CD may run in common sheath with bile duct
○Anomalous right hepatic ducts may be severed at cholecystectomy
•Close apposition of GB to duodenum can result in fistulous connection with chronic cholecystitis and erosion of gallstone into duodenum
Function & Dysfunction
•Obstruction of common bile duct is common
○Gallstones in distal bile duct
○Carcinoma arising in pancreatic head or bile duct
○Result is jaundice due to back up of bile salts into bloodstream
Embryologic Events
•Abnormal embryological development of fetal ductal plate can lead to spectrum of liver and biliary abnormalities including
○Polycystic liver disease
○Congenital hepatic fibrosis
○Biliary hamartomas
○Caroli disease
○Choledochal cysts
SELECTED REFERENCES
1.Shackelford RT: Shackelford’s Surgery of the alimentary tract. 7th edition. Elsevier/Saunders, 2013
2.Standring S et al: Gray's anatomy: the anatomical basis of clinical practice. Edinburgh: Churchill Livingstone/Elsevier,2008
Abdomen Anatomy:
21
Anatomy: Abdomen
Biliary System
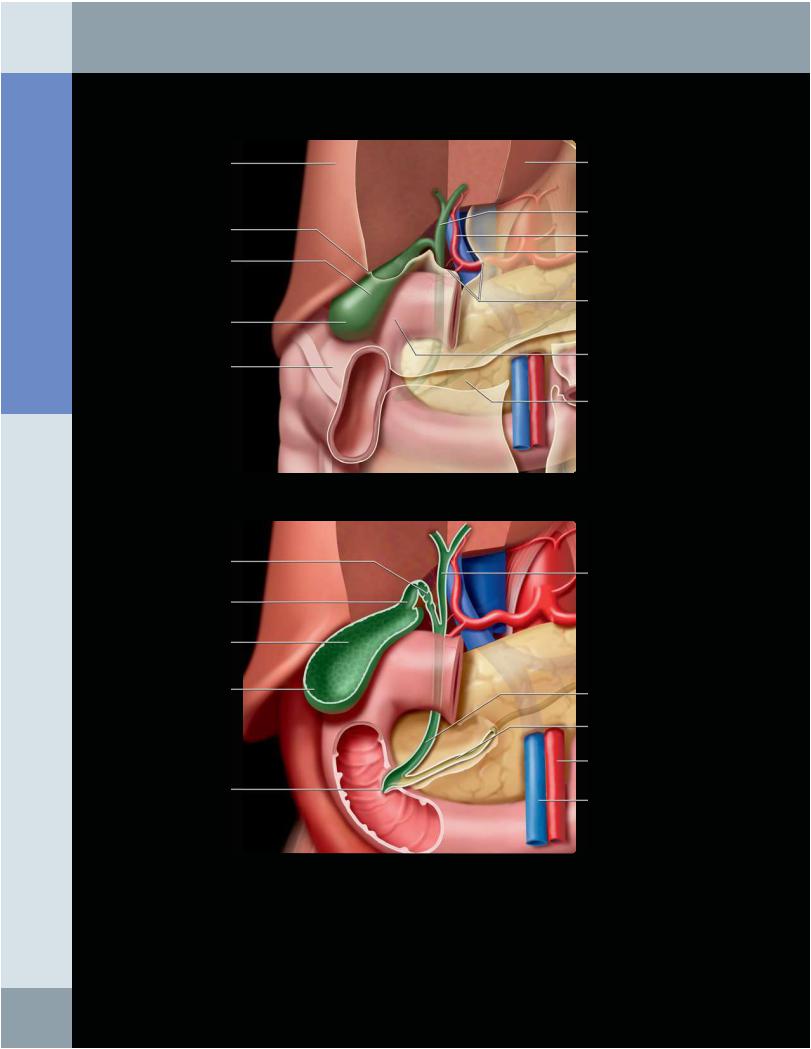
GALLBLADDER IN SITU
Right hepatic lobe
Peritoneal reflection
Gallbladder (body)
Gallbladder (fundus)
Colon (hepatic flexure)
Cystic duct
Neck
Body
Fundus
Ampulla
Left hepatic lobe
Extrahepatic bile duct
Proper hepatic artery Main portal vein
Lesser omentum (cut edge, anterior)
Duodenum
Pancreas
Common hepatic duct
Common bile duct
Pancreatic duct
Superior mesenteric artery
Superior mesenteric vein
(Top) Graphic shows that the gallbladder is covered with peritoneum, except where it is attached to the liver. The extrahepatic bile duct, hepatic artery, and portal vein run in the lesser omentum. The fundus of the gallbladder extends beyond the anterior-inferior edge of the liver and can be in contact with the hepatic flexure of the colon. The body (main portion of the gallbladder) is in contact with the duodenum. (Bottom) The neck of the gallbladder narrows before entering the cystic duct, which is distinguished by its tortuous course and irregular lumen. The duct lumen is irregular due to redundant folds of mucosa, called the spiral folds of Heister, that are believed to regulate the rate of filling and emptying of the gallbladder. The cystic duct joins the hepatic duct to form the common bile duct, which passes behind the duodenum and through the pancreas to enter the duodenum.
22
Biliary System
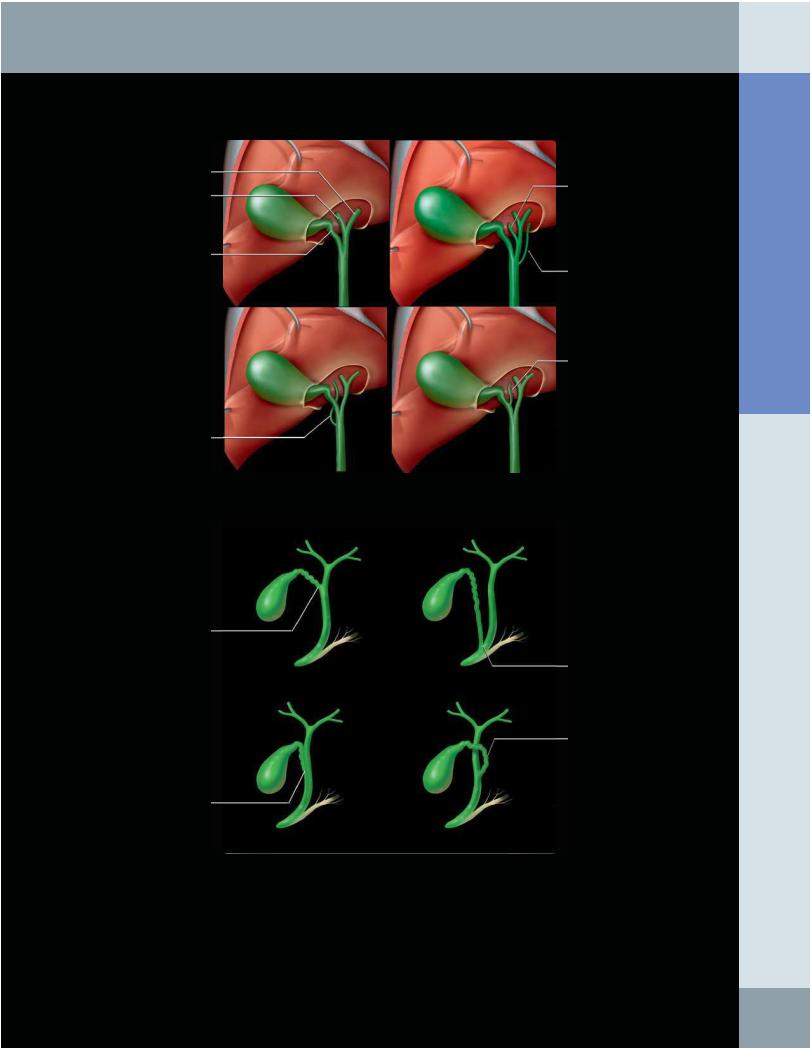
Left hepatic duct
Right hepatic duct
Cystic duct
Accessory right hepatic (joining common bile duct)
Conventional junction of cystic and common hepatic ducts
Cystic and common bile ducts in common sheath
ANATOMIC VARIATIONS OF BILIARY TREE
Accessory right hepatic (joining common hepatic duct)
Accessory left hepatic (joining common bile duct)
Accessory right hepatic (joining cystic duct)
Low insertion of cystic duct
Spiral course of cystic duct around common hepatic duct
(Top) Graphic shows the conventional arrangement of the extrahepatic bile ducts, but variations are common (20% of population) and may lead to inadvertent ligation or injury at surgery (such as during cholecystectomy), where the cystic duct is clamped and transected. Most accessory ducts are on the right side and usually enter the common hepatic duct, but they may enter the cystic or common bile duct. Accessory left ducts enter the common bile duct. While referred to as "accessory," these ducts are the sole drainage of bile from at least 1 hepatic segment. Ligation or laceration can lead to significant hepatic injury or bile peritonitis. (Bottom) The course and insertion of the cystic duct are highly variable, leading to difficulty in isolation and ligation at cholecystectomy. The cystic duct may be mistaken for the common hepatic or common bile duct.
Abdomen Anatomy:
23
