
новая папка / 450-550 operativ
.pdf
442 |
SRB’s Surgical Operations |
Fig. 15-6B
Figs 15-6A and B: Relations of thyroid gland–diagrammatic look.
2.Inferior thyroid artery is a branch of thyrocervical trunk of subclavian artery runs upwards, medially then downwards behind the carotid sheath and middle cervical sympathetic ganglion, in front of vertebral vessels divides into 4-5 terminal branches which pierce the pretracheal fascia separately to supply and enter the lower pole of the thyroid. Its ascending branch also supplies the parathyroid glands (both lower and upper).
3.yroidea ima artery (3-10%) also called as lowest thyroid artery arises from arch of aorta or brachiocephalic artery enters the gland and isthmus.
4.Accessory thyroid arteries arise from tracheal and oesophageal arteries also supply the gland (Fig. 15-7).
Venous supply is by –
1.Superior thyroid vein from upper pole accompanying the artery to join IJV or common facial vein.
2.Middle thyroid vein is a short, wide, thin walled vein begins from mid-lateral aspect of the lateral lobe running a short distance in front or behind the carotid artery, immediately enters into the IJV. Secure ligation of the vein is needed and if it tears, it may extend into IJV causing torrential haemorrhage. As it is the one that holds the gland
posteriorly, it should be ligated rst to mobilise the gland. Occasionally this vein may be absent. One should also remember that there is no middle thyroid artery.
3.Inferior thyroid veins begin at lower pole of isthmus form a plexus in front of trachea later joining the respective brachiocephalic vein. ese veins are not accompanied with inferior thyroid artery. Occasionally both inferior thyroid veins form a common trunk – thyroidea
ima vein which joins left brachiocephalic vein.
4.Kocher’s 4th thyroid vein may be present occasionally between middle and inferior thyroid vein, joins either IJV or middle thyroid or inferior thyroid vein.
Note:
Anterior jugular vein is a small but variable vein begins at submental region below the chin, descends vertically in superficial fascia 1 cm from midline. At 2.5 cm above the sternum, it pierces the deep investing fascia to enter the suprasternal space. Here it is connected by a communicating vein to opposite side called as jugular venous arch. Later the vein runs laterally deep to sternocleidomastoid towards its posterior border up to the clavicle to join the external jugular vein. Anterior jugular vein is variable – may be absent; may be in midline; may be quite large drained by common facial vein. This vein is important in thyroid surgeries even though it is not related to venous drainage of thyroid gland (Fig. 15-8).
Nerve Supply
It is mainly from middle cervical ganglion partly from superior and inferior cervical ganglion.
Lymphatic Drainage
(1) Primary nodes are tracheaprelaryngeal nodes (Delphian), pretracheal and paratracheal nodes, oesophageal nodes, and mediastinalnodes(brachiocephalicalso called assuperior mediastinal nodes). (2) Secondary nodes are deep cervical, supraclavicular and occipital nodes (Fig. 15-9).
Note:
Recurrent laryngeal nerve is in trachea-oesophageal groove in relation to Berry’s ligament and is very important structure in thyroidectomy. Parathyroid glands are four in number, two on each side – often embedded in thyroid gland. Removal of all four glands in thyroidectomy may lead into severe hypoparathyroidism and hypocalcaemia.
Fig. 15-7: Vessels of the thyroid gland. |
Fig. 15-8: Anatomy of anterior jugular vein. |

Chapter 15 Surgery for Thyroid and Parathyroid |
443 |
Fig. 15-9: Lymphatic drainage of thyroid gland.
Anatomy and Relations of Nerves with Thyroid Gland
External Laryngeal Nerve
External laryngeal nerve is a branch of superior laryngeal nerve. Vagus gives superior laryngeal nerve branch from its inferior ganglion of vagus which is at the level of greater cornu of hyoid bone, which in turn divides into internal laryngeal and external laryngeal nerves. Internal laryngeal nerve pierces the thyrohyoid membrane and gives sensory supply to larynx above the vocal cord and hypopharynx. External laryngeal nerve runs close to superior thyroid vessels to supply cricothyroid muscle which is tensor of vocal cord. It may get injured while ligating superior pedicle causing defective pitch of the voice. So the upper pedicle of thyroid should be ligated close to gland but after identi cation and dissection of the nerve (Fig. 15-10).
Recurrent Laryngeal Nerve
Recurrent laryngeal nerve is a branch of vagus which hooks around ligamentum arteriosum on the left with arch of aorta and right
Fig. 15-10A
B
C
Figs 15-10B and C
Figs 15-10A to C: Anatomy of recurrent laryngeal nerve and external laryngeal nerve.
subclavian artery on the right side. It runs in the tracheo-oesophageal groove near the posteromedial surface close to thyroid gland. Nerve lies in between branches of inferior thyroid artery. On the right side, the nerve runs between branches of the artery in approximately 50% of patients, anterior to the artery in 25% and posterior in 25%. On the left, the nerve runs posteriorly to the artery in 50% of patients, in 35% the nerve runs between branches, in 15% it is anterior to the artery. So the nerve is always near the artery, but the exact relationship cannot be determined. Hence inferior thyroid artery should be ligated away from the gland (old theory, not practiced now). Anomalies of the nerve should be remembered. In 5% of cases nerve passes through the gland. Nerve may be much more away from the gland. Nerve may be closely

444 |
SRB’s Surgical Operations |
adherent to gland posteriorly. Nerve may lie within the ligament of Berry (25%). Redd in 1943 described 28 variations in RLN relation to inferior thyroid artery. In his observation – RLN is deep to artery in 40%; super cial in 20% and in between branches in 35%; only in 17% of cases pattern were same in both sides.
Nonrecurrent laryngeal nerve may be present in 1 to 5 in 1,000 cases with a horizontal course. In 5 of 1000 patients, a nonrecurrent laryngeal nerve is found on the right side. is arrangement occurs when a retroesophageal right subclavian artery arises from the dorsal side of the aortic arch. e non-recurrent laryngeal nerve branches from the vagus at approximately at the level of the cricoid cartilage and directly enters the larynx without looping around the subclavian artery. A left-sided non-recurrent laryngeal nerve can occur only when a right-sided aortic arch and ligamentum arteriosum are concurrent with a left retroesophageal subclavian artery.
RLN supplies all muscles (abductors, adductors) of the larynx except cricothyroid and also sensory supply of larynx below the vocal cords (Fig. 15-11).
Muscles of the Larynx
Cricothyroid – It is the only muscle which is located on the external aspect of the larynx. It is supplied by external laryngeal nerve. It is tensor and mild adductor of the vocal cord.
Abductors of the vocal cord – Posterior cricoarytenoids. Adductors of the vocal cord – Lateral cricoarytenoids, transverse arytenoid, thyroarytenoids and cricothyroids.
Relaxant of vocal cords – yroarytenoids and vocalis.
Muscles which close the laryngeal inlet – Oblique arytenoids and aryepiglottic.
Muscles which open the laryngeal inlet – yroepiglotticus (Fig. 15-12).
Positions of vocal cord –
Median; paramedian (1.5 mm); normal; cadaveric/neutral (3.5 mm); gentle abduction (7 mm); completely abducted (9.5 mm).
Fig. 15-11: Nerves and arteries related to thyroid gland. External and recurrent laryngeal nerves and superior and inferior thyroid arteries are important structures while doing thyroidectomy. Parathyroid glands are also equally important.
Fig. 15-12: Thyroid and cricothyroid cartilages with cricothyroid muscle. Cricothyroid has got straight and oblique parts. Straight originates from arch of cricoid cartilage to posteroinferior margin of the thyroid lamina. Oblique part runs from cricoid cartilage to inferior horn of thyroid cartilage. Cricothyroid is supplied by external branch of superior laryngeal nerve. Branch is closely associated with superior thyroid vessels.
Assessment of voice change
•Pitch of the voicewhether raised/lowered or pitch locked
•Breath support during speaking is adequate or not
•Ability to alter the rapidity of speech – slow/fast/medium
•Altered laryngeal and neck muscle tension
•Indirect laryngoscopywith tongue pulled out using gauze, warmedILS is introduced into the oral cavity to see vocalcords. Patient is asked to say ‘e’ to see the vocalcord movements
Rule of ‘2’ in thyroid
•2 lobes
•2 origins – Thyroglossal duct, C cells neural crest
•2 capsules – true,false
•2 arteries
•2 nerves related deep
•2 tubes related deep
•2 muscles related deep
•2 lymphatic drainage area – central and lateral
•2 parathyroids each lateral lobe
•2 triangles – BHEARS; JOLLS
•2 hormones (T3/T4; Calcitonin)
Jolls triangle |
BHEARS triangle |
Formedbymidline;strapmuscles; |
RLN; CCA; inferior thyroid artery; at |
sup thyroid pedicle. Its floor is |
anteromedialaspect ofthe thyroid. |
cricothyroid. It contains external |
|
laryngealnerve. |
|
Hyoid Bone
It is U shaped bone located in the middle of the anterior aspect of the neck between chin and thyroid cartilage. It develops from 2nd and 3rd branchial arches. It is suspended by tips of the styloid processes of two temporal bones by stylohyoid ligament. It lies at the level of base of the mandible in front and 3rd cervical vertebra behind. It provides attachment to tongue and oor of the mouth above; larynx below; epiglottis and pharynx behind. It has got central body and two pairs of greater and lesser cornua.

Anterior surface of the body is convex and is directed forwards and upwards. Posterior surface of body is directed backwards and downwards. ere is a transverse ridge in the body which divides the body of the bone into upper and lower parts and deep cervical fascia is attached to it. Geniohyoid, mylohyoid, genioglossus, hyoglossus, sternohyoid, omohyoid and thyrohyoid muscles are attached to body.
yrohyoid membrane is attached to upper border from behind and below. Pretracheal fascia is attached to lower border. Greater cornua gives origin to middle constrictor medially and hyoglossus laterally; insertion of stylohyoid muscle; attachment of brous loop (pulley) of central tendon of the digastric muscle. Two small conical spike like projections lesser cornua give attachments to stylohyoid ligaments one on each side.
Thyroid moves upwardsduring deglutition–
•During 1st stage ofdeglutition
↓
•Hyoid moves upwards by constrictor action
↓
•Pulls pretracheal fascia upwards
↓
•Pulls ligamentofBerry
↓
•Pulls thyroid upwards
Note:
All structures enclosed in pretracheal fascia willmove with deglutition –
•Thyroglossal cyst
•Pretracheal lymph nodes
•Subhyoid bursa
 EXCISION OF THYROGLOSSAL CYST
EXCISION OF THYROGLOSSAL CYST
yroglossal cyst is due to congenital incomplete regression of the thyroglossal duct along its pathway, persisting as tubulodermoid cystic swelling in the midline towards left which causes a ‘tug’ while protruding the tongue and also moves upwards while swallowing. Often gland will be present only in the wall of the cyst with empty thyroid fossa. Ultrasound neck, radioisotope study, T3, T4, TSH and FNAC of cyst is needed before surgical removal. Entire track up to the foramen caecum of tongue (at the junction of middle and posterior third of the tongue) should be excised to prevent recurrence or stula formation (Fig. 15-13).
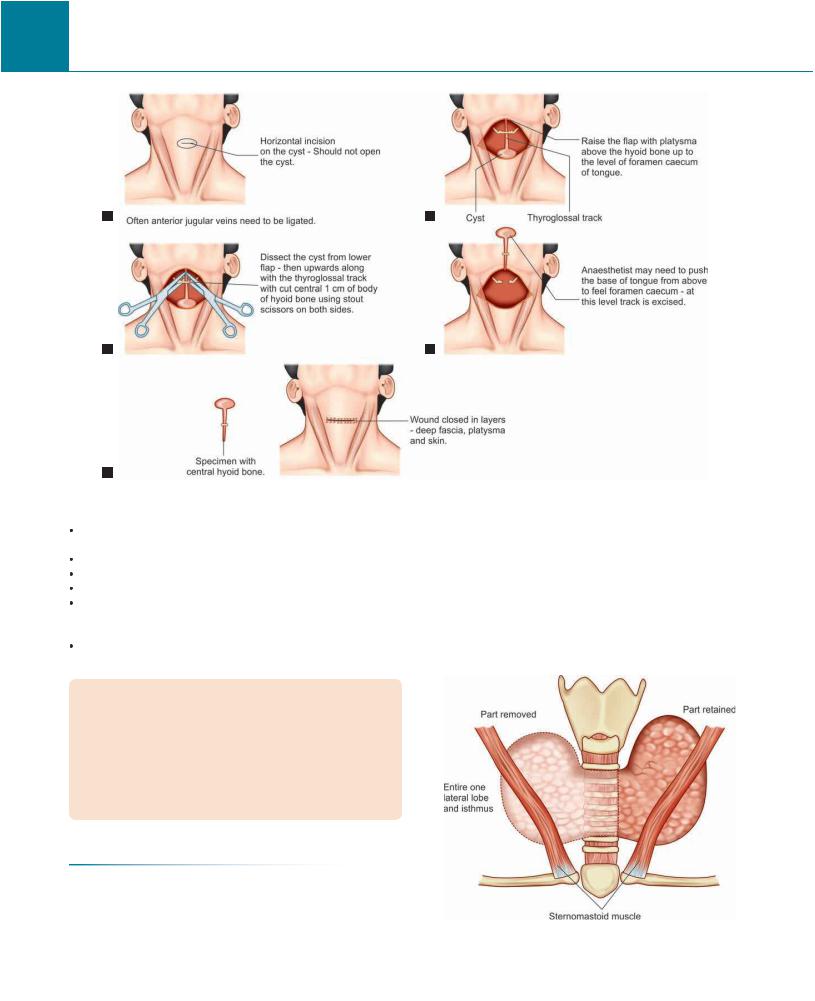
Technique (Sistrunk Operation) (Fig. 15-14)
It is done under general anaesthesia. Position is supine with neck extended. rough transverse neck incision placed over the cyst, skin ap is raised above along with platysma. Care should be taken not to open the cyst. Deep fascia is opened vertically in midline. Cyst with surrounding tissues is dissected up to the hyoid bone. Sternohyoid and thyrohyoid muscles are separated and retracted. Cyst is mobilized upwards along with the track. Track is densely adherent to the body of hyoid bone above. Hyoid bone is separated from the thyrohyoid membrane through a clean fascial plane without fear of opening the pharyngeal wall. Geniohyoid and mylohyoid muscles superiorly and sternohyoid inferiorly are divided o from the hyoid. Central 1 cm part of the hyoid bone is resected along with intact track within it. Track with adjacent tissues is dissected above up to the foramen caecum. Adjacent tissues also should be removed because of possibility of multiple tracks which otherwise lead to recurrence or fistula formation. Often anaesthetist is asked to apply digital pressure over
Chapter 15 Surgery for Thyroid and Parathyroid |
445 |
A
B
Figs 15-13A and B: Thyroglossal cyst when present commonly normal lateral lobes will be present. But occasionally normal lateral lobes may be absent and only thyroid tissue existing in these patients will be in the wall of the thyroglossal cyst.
base of the tongue near foramen caecum to facilitate the dissection and to con rm the reach up to the foramen caecum. Track is ligated at foramen caecum using 3 zero vicryl and removed. Recurrence rate by removal of only track without central hyoid is 25%. Removal of track with central hyoid reduces the recurrence rate to 5%. Haemostasis is maintained using bipolar cautery. A suction drain is placed.
 omplications of Neck Injury
omplications of Neck Injury
 THYROIDECTOMY
THYROIDECTOMY
yroidectomy is a surgery of precision, patience and perfection.
Principles are –
Absolute haemostasis. Bipolar cautery should be used. Minimise/ avoid using monopolar cautery in main dissection as lateral heat may damage RLN or parathyroid blood supply.
446 |
SRB’s Surgical Operations |
A
C
E
Fig. 15-14: Thyroglossal cyst excision steps – A to E.
Prevention of injury to recurrent laryngeal nerve and external laryngeal nerve.
Preservation of parathyroid glands. Cosmesis.
Meticulous technique.
RLN and ELN should be identi ed during dissection. All vessels should be ligated individually.One should avoid mass ligation even though it is commonly practiced.
Middle thyroid vein, superior thyroid artery and vein then inferior thyroid vessels are ligated in order.
Preoperative preparation
•Blood grouping, cross matching and required blood should be kept ready.
•Indirect laryngoscopy. Patientis asked to tell ‘E’ to check the abduction of vocal cord. IL scope should be soaked in warm water to prevent fogging andblurring of the IL scope.
•Serum calcium estimation; T3, T4, TSH; Thyroid antibodies, endocrinologist’s opinion.
•ECG and cardiac fitness especially in toxic goiter.
•Radioisotope iodine scan; FNAC.
Di erent Types of Thyroidectomies
Hemithyroidectomy
It is removal of one lateral lobe with entire isthmus. It is done in benign disease involving only one lobe like solitary nodule thyroid either toxic or nontoxic (adenoma/colloid goitre of one lobe/ colloid cyst). After hemithyroidectomy, if histology report comes
B
D
as differentiated malignancy either papillary or follicular then completion thyroidectomy is done immediately within one week. If histology report comes after one week then completion thyroidectomy is done after 3 weeks. Reexploration is not advisable in 2nd and 3rd weeks (Fig. 15-15).
Subtotal Thyroidectomy
It is removal of most of both lateral lobes including isthmus, except around 8 gram of tissue (or tissue equal to pulp of little nger) in lower
Fig. 15-15: Hemithyroidectomy: Entire one lateral lobe and entire isthmus are removed retaining entire opposite lateral lobe. It is done in solitary nodule/toxic or non-toxic adenoma in one lobe.

Chapter 15 Surgery for Thyroid and Parathyroid |
447 |
Fig. 15-16: Subtotal thyroidectomy.
pole. It is done in toxic thyroid and often in nontoxic multinodular goitre. It reduces the incidence of hypoparathyroidism and injury to recurrent laryngeal nerve (Fig. 15-16).
Partial Thyroidectomy (Thomas)
It is removal of mobilised gland in front of trachea including entire isthmus. It was the procedure done earlier in nontoxic multinodular goitre. It is at present not commonly used (Fig. 15-17).
Near Total Thyroidectomy
Here both lateral lobes except small tissue in lower pole are removed. It is to safeguard the recurrent laryngeal nerve and parathyroid blood supply. It is advocated in papillary carcinoma of thyroid (usually in
Fig. 15-17: Partial thyroidectomy is removal of mobilized gland in front of the tracheal level. Glands in trachea-oesophageal grooves are retained. It is not commonly done now.
Fig. 15-18: Near total thyroidectomy.
young individuals). Isthmus is entirely removed. Tissue is retained either in one or both sides (Fig. 15-18).
Total Thyroidectomy
Here entire gland is removed without retaining any tissue. It is the present procedure of choice in most of the thyroid diseasesexcept benign disease limited to one lateral lobe. It is done at present in nontoxic multinodular goitre, toxic goitre, carcinoma thyroid (follicular/ medullary/papillary/operable/anaplastic) (Fig. 15-19).
Fig. 15-19: Total thyroidectomy. It is done in follicular carcinoma and medullary carcinoma of thyroid.
Hartley Dunhill Operation
It is removal of one entire lateral lobe, isthmus and partial/subtotal removal of opposite lateral lobe. It is used in nontoxic multinodular goitre (Fig. 15-20).
Isthmectomy
It is done in advanced carcinoma or occasionally in Riedel’s thyroiditis to treat severe stridor due to tracheal narrowing.
Note: Isthmus should be removed in entirety in any type of thyroidectomy, and if it is retained partially it gets adherent to wound in front creating a cosmetically poor scar (Fig. 15-21).

448 |
SRB’s Surgical Operations |
Fig. 15-20: Hartley Dunhill operation.
Fig. 15-21: Emil Theodor Kocher – Father of thyroid surgery.
Procedure (Fig. 15-21)
Anaesthesia
General anesthesia is used. Occasionally local anaesthesia can be used in patients who are not t for general anaesthesia. Oesophageal stethoscope often may be required to place in case of retro/paraoesophageal goitres.
Position
Neck is extended by placing sandbag/round bolus/Dunhill pillow/ folded sheet/in atable thyroid pillow/in atable intravenous uid cu underneath the shoulder. Ring should be kept under the occiput. Both arms are kept beside patient’s bodyand hands are tugged/tucked under the patient’s buttock. Cotton pads are placed under the elbow to prevent ulnar nerve compression. Head end of the table is elevated to 15° to improve venous return so as to reduce venous congestion in the neck and so oozing (reverse Trendelenburg/Rose/Barking dog/Kocher’s position). is increases the risk of air embolism due to negative pressure created in neck veins. Veins should be ligated securely and then only cut. Any doubtful air in IJV should be aspirated immediately (Fig. 15-22).
Anaesthetists are on the head end away from the eld of surgery with sides kept free for surgeon, assistant and scrub nurse.
Cleaning of the area – neck, face, chest up to nipples is done. Draping is done on all sides. Double towel is placed under the head and one of the towels (outer one) is covered over the outer part of the endotracheal tube. Sterile transparent plastic drape is ideal if available. Surgeon stands on right side, assistant on left side and scrub nurse on right side at foot end of the patient. Energy sources like cautery (both unipolar and bipolar)/ ligaseal/harmonic, etc. are kept ready. Suction apparatus with ne suction tip is needed (Fig. 15-23).
Incision
Horizontal crease incision is placed two fingerbreadth (2-3 cm) above the sternal notch extending from posterior border of one sternocleidomastoid to opposite side. Incision is marked by placing stretched thread or silk over the skin. It can be marked using marking ink. Often few surgeons use 60 ml of 1 in 400000 adrenaline saline to inject into the super cial fascia to reduce bleeding while raising the
ap. Skin is incised using no 15 blade. In women with heavy breasts incision is placed slightly at higher level than usual as subsequent scar may be dragged downwards close to sternum creating ugly scar. Platysma is identi ed and incised slightly at higher level than skin to prevent it getting adherent to scar at a later period (Fig. 15-24).
Raising the Flaps
Upper flap (subplatysmal flap) is raised up to thyroid cartilage (platysma is absent in the midline); lower ap up to sternoclavicular joint/clavicular heads and suprasternal notch (Figs 15-25 and 15-26).
Rising of ap is done either using cautery or no. 15 blade or curved sharp scissor or blunt gauze dissection using nger. All bleeders are fulgurated properly.Care should be taken not to injure anterior jugular veins running on either side of the midline. ere may be chance of air embolism if it is injured. In the lower part of the wound near lower ap both anterior jugular veins communicate through a communicating vein which if injured may cause bleeding and air embolism. In such situation anterior jugular veins distal to the communicating vein level should be ligated to prevent air embolism. Later veins are ligated proximally (Fig. 15-27).
Retraction of the Flaps
A self-retaining Joll’s thyroid retractor is placed. Silk skin sutures to upper and lower aps can be placed to retract instead of Joll’s retractor. Hamburger–Brennan–Mahorner self-retaining retractor can also be used (Figs 15-28 to 15-30).
Dissection
Deep fascia is incised vertically in midline/median raphe. Strap muscles are retracted (sternohyoid and omohyoid are in outer plane; sternothyroid is in deeper plane). Midline plane is blood less. Incision is done and plane is opened using either cautery or 15 no blade or ne scissor. Strap muscles are retracted laterally using a deep retractor. If gland is large and if there is di culty in mobilising gland then strap muscles can be cut between two Kocher’s clamps at their upper part (as nerve supply to strap muscles is at lower part through ansa hypoglossi) (Figs 15-31 and 15-32).

Chapter 15 Surgery for Thyroid and Parathyroid |
449 |
Figs 15-22(1)

450 |
SRB’s Surgical Operations |
Figs 15-22(2)
Figs 15-22(1 and 2): Position of the patient in thyroidectomy. Neck is extended by placing the sandbag under the shoulder. 15° head up position is used. After cleaning, draping is done using double sterile towels to the head.
Fig. 15-23: Position and cleaning the area.
yroid fossa lateral and deep to the lateral lobe is dissected using blunt (peanut) and sharp dissection. Lateral lobe of the thyroid is held using gauze or Babcock’s forceps to retract medially. Short stout middle thyroid vein is identi ed and ligated securely (double ligation is better) using 3 zero silk/vicryl. Blind dissection (should be avoided) near middle thyroid vein may tear or avulse it from IJV causing torrential haemorrhage. is allows proper mobilization of the gland to identify parathyroid glands and recurrent laryngeal nerve
(Fig. 15-33).
Gland is now retracted downwards and laterally to expose the superior pole. It is dissected with sharp and peanut dissections. Superior thyroid artery and vein supplies the gland from superior pole. is space in front of cricothyroid is called as cricothyroid space of Reeves. In this space external laryngeal nerve which is just proximal to superior pole deviates towards cricothyroid muscle. Cricothyroid muscle is tensor of vocal cord which maintains the pitch of the voice.
is nerve should not be injured. So artery and vein are individually
Fig. 15-24: Incision for thyroidectomy.
Fig.15-25:Subplatysmalplaneisusedwhileraisingthe apinthyroidectomy.

Chapter 15 Surgery for Thyroid and Parathyroid |
451 |
Fig. 15-26: Raising of upper ap and lower aps in subplatysmal plane.
Fig. 15-27: Flaps are raised using monopolar cautery or scissor or gauze or nger dissection.
