
новая папка / 80
.pdf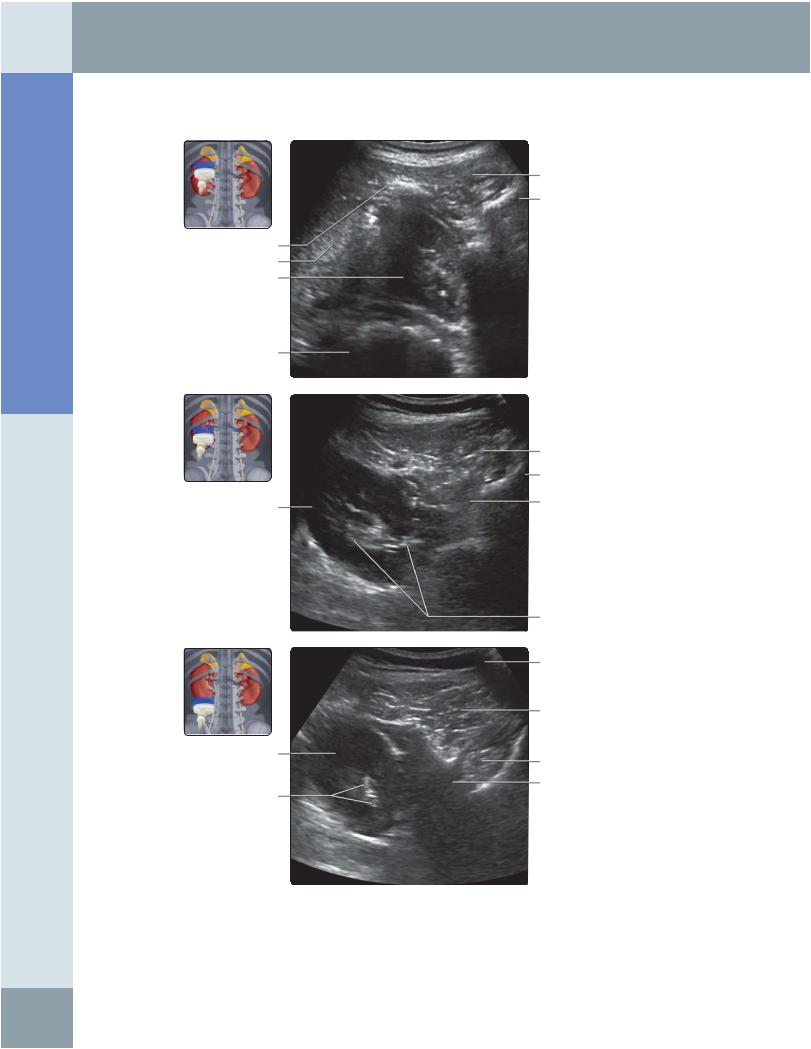
Anatomy: Abdomen
Kidneys
LEFT KIDNEY, POSTERIOR ABDOMEN SCAN
Shadowing from rib
Spleen
Upper pole of left kidney
Gas in stomach
Mid pole of left kidney
Lower pole of left kidney
Renal sinus echoes
Left erector spinae muscle
Vertebral body
Left erector spinae muscle
Vertebral body
Left psoas muscle
Renal sinus echoes
Subcutaneous fat
Left quadratus lumborum muscle
Left psoas muscle
Posterior pararenal fat
(Top) Transverse grayscale ultrasound of the upper pole of the left kidney using the posterior approach is shown. Note the proximity of the kidney to the skin surface and absence of intervening bowel/other major structures, making this a suitable approach for renal interventional procedures. (Middle) Transverse grayscale ultrasound of the upper pole of the left kidney using the posterior approach shows the proximity of the kidney to the skin surface and absence of intervening bowel/other major structures, making this a suitable approach for renal interventional procedures. (Bottom) Transverse grayscale ultrasound of the lower pole of the left kidney using the posterior approach is shown.
64
Kidneys
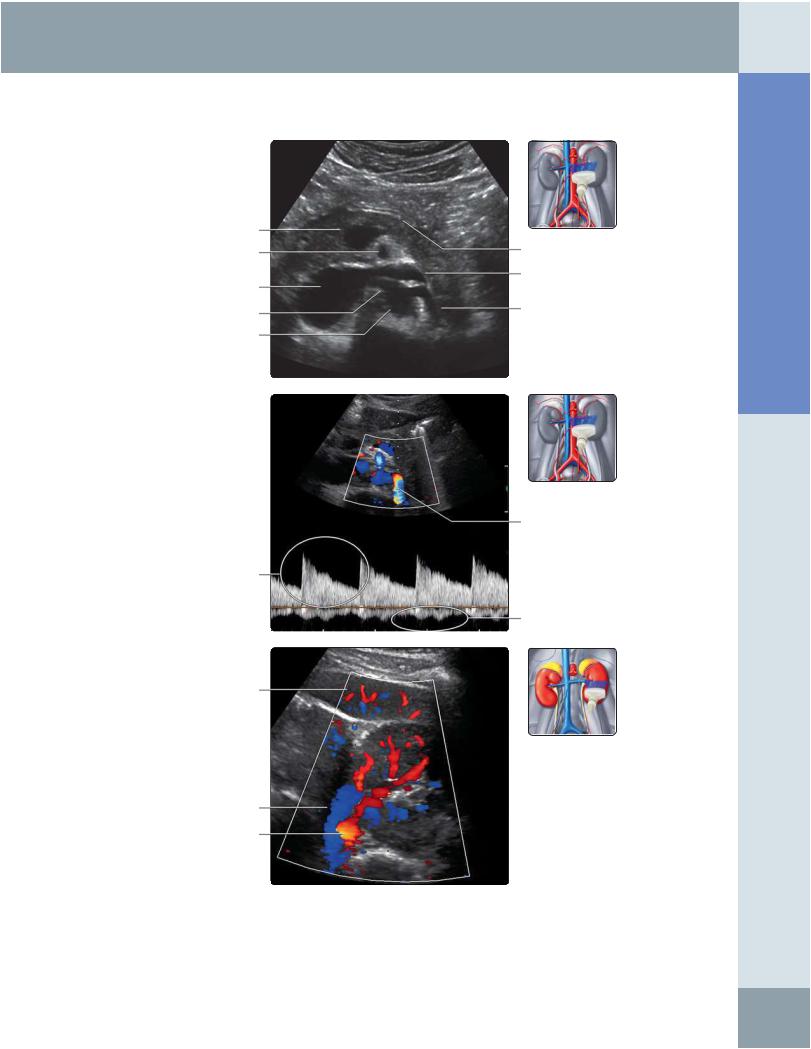
LEFT MAIN RENAL ARTERY AND VEIN
Splenic vein/superior mesenteric vein
confluence Superior mesenteric artery
Inferior vena cava
Right renal artery
Aorta
Continuous forward systolic arterial flow
Spleen
Left renal vein
Left renal artery
Pancreas
Left renal vein
Left renal artery
Left renal artery
Phasic venous flow
(Top) Transverse ultrasound in the anterior midline shows that the left renal artery arises from the anterolateral aorta just around or below the level of the superior mesenteric artery. The normal caliber of the renal artery ranges from 5-8 mm. The left renal vein courses between the aorta and superior mesenteric artery. (Middle) Spectral Doppler waveform of the left renal artery and vein is shown. The normal PSV in the artery ranges from 60-140 cm/s with a normal resistive index < 0.7 and pulsatility index < 1.8. There is variability in venous velocity consequent upon cardiac and respiratory activity. The renal vein normally measures 4-9 mm in caliber with a PSV of 1833 cm/s. (Bottom) Transverse color Doppler waveform of the left renal hilum obtained from an anterolateral approach is shown. An anterior approach may not be feasible secondary to bowel gas. The left renal artery is posterior to the left renal vein.
Abdomen Anatomy:
65
Anatomy: Abdomen
Kidneys
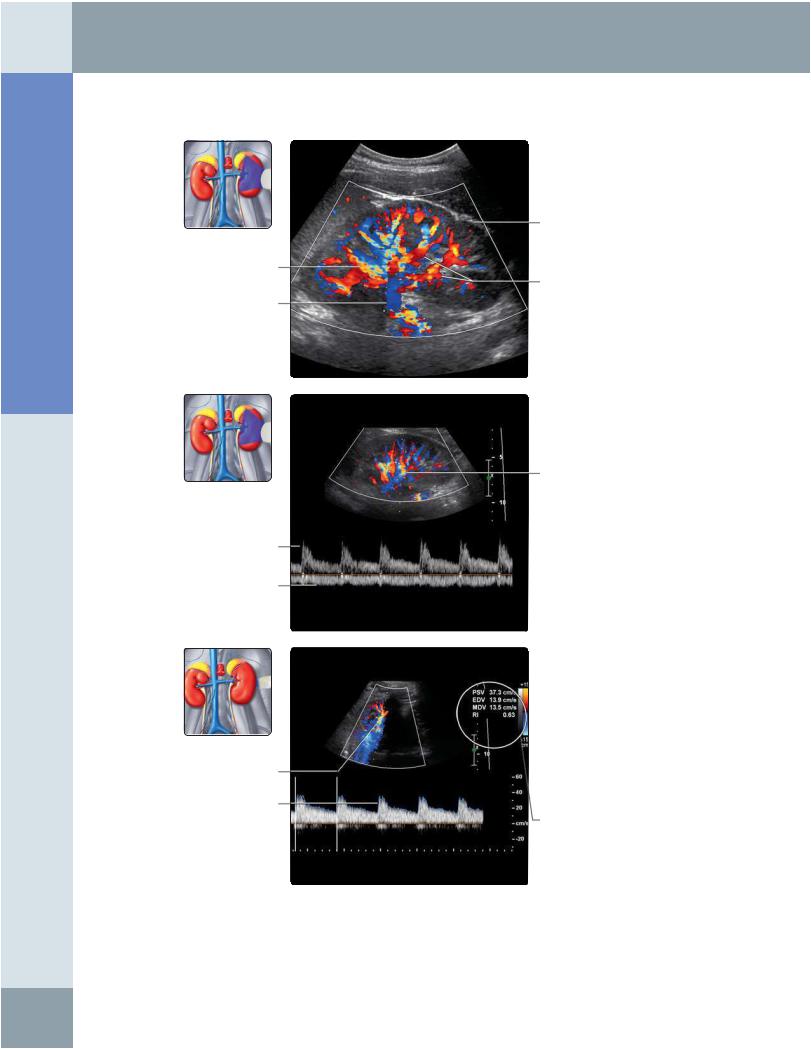
LEFT INTRARENAL ARTERY AND VEIN
Color aliasing
Main renal vein
Low-resistance renal artery spectral
Doppler waveform
Venous waveform
Segmental renal artery
Renal artery spectral Doppler waveform with autotrace
Renal cortex
Intrarenal segmental arteries
Intrarenal renal artery
Renal Doppler indices
(Top) Longitudinal color Doppler ultrasound of the left kidney shows renal artery branches as red and renal vein branches as blue. There is some color aliasing in the veins, shown as yellow. (Middle) In this spectral Doppler waveform of a left segmental renal artery, there is continuous flow throughout the cardiac cycle with a lowresistance pattern. The segmental renal vein shows mild phasicity. (Bottom)
Spectral Doppler waveform of a left segmental renal artery in the transverse plane is shown. Doppler indices are normal: PSV of 37.3 cm/s, EDV of 13.9 cm/s, and resistive index (RI) of 0.63.
66
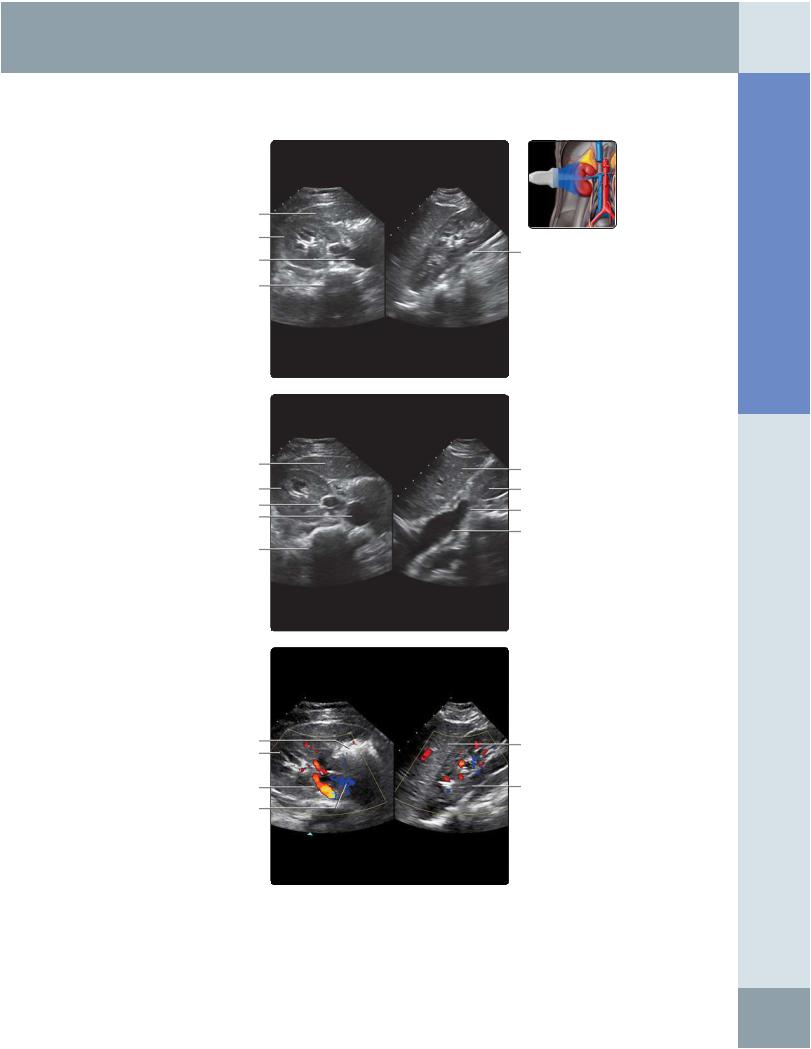
Right lobe of liver
Right kidney in transverse plane
Inferior vena cava
Vertebra
Right lobe of liver
Transverse image of right kidney
Right renal vein Inferior vena cava
Vertebra
Bowel Right kidney in transverse plane
Right renal artery
Inferior ven cava
Kidneys
MULTIPLANAR ULTRASOUND OF RIGHT KIDNEY
Right kidney in sagittal plane
Liver
Right kidney
Right renal vein
Longitudinal image of inferior vena cava
Right lobe of liver
Right kidney in longitudinal plane
Abdomen Anatomy:
(Top) 3D real-time ultrasound with a matrix probe in shown in which simultaneous axial and sagittal images are obtained. The sagittal plane can be steered electronically to obtain the long axis of the kidney. (Middle) In this 3D real-time ultrasound with a matrix probe, the sagittal plane has been steered electronically to obtain a longitudinal view of the inferior vena cava and right renal vein. (Bottom) 3D real-time ultrasound with a matrix probe in shown in which simultaneous axial and sagittal images are obtained. This technology can enable imaging in planes not otherwise feasible.
67
Anatomy: Abdomen
Bowel
GROSS ANATOMY
Divisions
•Esophagus: Cervical and thoracic segments
•Stomach
○Hollow muscular organ between esophagus and small intestine
○Location: Intraperitoneal, in left upper quadrant, bordered superiorly by left hemidiaphragm, posterolaterally by spleen, posteroinferiorly by pancreas
–Greater omentum attached from greater curvature and drapes over small and large intestines
–Lesser omentum attached from lesser curvature to porta hepatis, covers lesser sac
○Function
–Gastric acid production for breakdown of large molecules of food into smaller molecules in preparation for small intestinal absorption
–Storage of food
○Sections
–Gastroesophageal junction/cardia, lower esophageal sphincter
–Fundus and body: Delineated by horizontal plane passing through cardia
–Antrum/pylorus: Lower section facilitating entry of gastric contents into duodenum
○Curvatures
–Greater curvature: Lateral wall of stomach
–Lesser curvature: Medial wall of stomach
○Rugae/internal ridges increase surface area for digestion
○Arterial supply
–Right and left gastric arteries supply lesser curvature
–Right and left gastroepiploic arteries supply greater curvature
–Short gastric artery supplies fundus
○Venous drainage
–Follow arteries and drain into portal vein and its tributaries
•Small bowel
○Between stomach and large intestine
○~ 4-7 meters in length
○Centrally located in abdomen
○Intraperitoneal, except for 2nd-4th portions of duodenum
○Function: Further breakdown of food molecules from stomach with eventual absorption
○Intraluminal extensions/folds valvulae conniventes increase surface area for absorption
–Abundant in proximal small bowel, decrease in number in distal small bowel loops
○Duodenum
–C-shaped hollow tube connecting stomach with jejunum
–Begins with duodenal bulb, ends in ligament of Treitz (duodenojejunal junction)
–Arterial supply and venous drainage: Superior and inferior pancreaticoduodenal artery, pancreaticoduodenal veins
○Jejunum
–Connects duodenum with ileum
–~ 2.5 meters in length
–Begins at ligament of Treitz
–Along with ileum, suspended by mesentery
–Arterial supply and venous drainage: Superior mesenteric artery and vein
○Ileum
–Connects jejunum with ascending colon
–~ 3.5 meters in length
–Along with jejunum, suspended by mesentery
–Arterial supply and venous drainage: Superior mesenteric artery and vein
•Large bowel
○Between small bowel and anus
○~ 1.5 meters in length
○Peripherally located in abdomen
–Cecum and appendix, transverse colon, and rectosigmoid are intraperitoneal
–Ascending colon, descending colon, and middle rectum are retroperitoneal
–Distal rectum is extraperitoneal
○Function: Absorption of remaining water, storage, and elimination of waste
○Sections
–Ascending colon: Located in right side of abdomen, includes cecum where appendix arises
–Hepatic flexure: Turn of colon at liver
–Transverse colon: Traverses upper abdomen
–Splenic flexure: Turn of colon at spleen
–Descending colon: Left side of abdomen
–Sigmoid/rectum: At posterior pelvis
○With taenia coli: 3 bands of smooth muscle just under serosa
–Haustration: Sacculations in colon resulting from contraction of taenia coli
–Epiploic appendages: Small fat accumulations on viscera
○Arterial supply
–Superior mesenteric artery supplies colon from appendix through splenic flexure
–Ileocolic branch supplies cecum
–Right colic branch supplies ascending colon
–Middle colic branch supplies transverse colon
–Inferior mesenteric artery supplies descending colon through rectum
–Left colic branch supplies descending colon
–Sigmoid branches supply sigmoid
–Superior rectal artery supplies superior rectum
–Middle and inferior rectum are supplied by arteries of same name originating from internal iliac artery
○Venous drainage
–Superior and inferior mesenteric veins
•Anus
○External opening of rectum
–Termination of gastrointestinal tract
○With sphincters for controlling defecation
○Internal anal sphincter
–Thin ring of smooth muscle surrounding anal canal, deep to submucosa
–Under involuntary control
–Continuous with muscularis propria of rectum
68
Bowel
–Forms an incomplete ring in females
○External anal sphincter
–Thick ring of skeletal muscle around internal anal sphincter
–Under voluntary control
–3 parts from superior to inferior: Deep, superficial, and subcutaneous
○Longitudinal muscle
–Thin muscle between internal and external anal sphincters
–Conjoined muscle from muscularis propria of rectum and levator ani
Histology
•Bowel wall throughout GI tract has uniform general histology, comprised of 4 layers
○Mucosa
–Functions for absorption and secretion
–Composed of epithelium and loose connective tissue
–Lamina propria
–Muscularis mucosa (deep layer of mucosa)
○Submucosa
–Consists of fibrous connective tissue
–Contains Meissner plexus
○Muscularis externa
–Muscular layer responsible for peristalsis or propulsion of food through gut
–Contains Auerbach plexus
○Serosa
–Epithelial lining continuous with peritoneum
IMAGING ANATOMY
Overview
•GI tract extends from mouth to anus
•Esophagus, which is intrathoracic, is difficult to visualize with external ultrasound due to rib cage and air-containing lungs
○Endoluminal ultrasound performed to assess mural pathology
•Stomach to rectum lie within abdomen and pelvis
•Stomach, 1st part of duodenum, jejunum, ileum, transverse colon, and sigmoid colon suspended within peritoneal cavity by peritoneal folds and are mobile
•2nd to 4th part of duodenum, ascending colon, descending colon, and rectum are typically extraperitoneal/retroperitoneal
○Retroperitoneal structures have more fixed position and are easyto locate
•Stomach located in left upper quadrant
○Identified by presence of rugae/mural folds
○Prominent muscular layer facilitates identification of pylorus
•Small bowel loops are located centrally within abdomen
○Abundant valvulae conniventes helps identify jejunal loops
○Jejunalization of ileum seen in celiac disease to compensate for atrophy of folds in proximal small bowel
○Contents of jejunal loops are usually liquid and appear hypoechoic/anechoic
•Cecum and colon identified by haustral pattern
○Located peripherally in abdomen
○Contain feces and gas
○Haustra seen as prominent curvilinear echogenic arcs with posterior reverberation
○Cecum identified by curvilinear arc of hyperechogenicity (representing feces and gas) in right lower quadrant blind-ending caudally
○Not uncommonly, cecum high-lying and may be horizontally placed
○Sigmoid colon variable length and mobile
○Junction of left colon with sigmoid colon identified in left iliac fossa by tracing descending colon
○Rectosigmoid junction has fixed position and is identified with full bladder, which acts as acoustic window
•Appendicular base normally located in right lower quadrant
○Length and direction of tip vary
○Retrocecal appendix and pelvic appendix can be difficult to locate transabdominally
–Transvaginal ultrasound examination useful to identify pelvic appendix
•Normal measurements of bowel caliber
○Small bowel < 3 cm
○Large bowel
–Cecum < 9 cm
–Transverse colon < 6 cm
•Stratified appearance of bowel wall on histology is depicted by 5 distinct layers on ultrasound as alternating echogenic/sonolucent (hypoechoic) appearance (gut signature)
○Interface of lumenand mucosa: Echogenic
○Muscularis mucosa: Hypoechoic
○Submucosa: Echogenic
○Muscularis propria/externa: Hypoechoic
○Serosa: Echogenic
•Normal bowel wall thickness < 3 mm
Bowel Motility
•Bowel is hollow viscus and is constantly mobile due to peristalsis
○Assessing direction of flow of contents often challenging
○When visibility permits, direction of flow can be determined by following long segments of bowel in continuous fashion
•Fixed points of bowel are easy to assess with transabdominal ultrasound
○Pylorus, "C loop" of duodenum, and ileocecal junction useful landmarks to assess direction of content flow
•Different bowel pathologies have potential to alter normal gut motility
•Real-time dynamic ultrasound provides useful information regarding bowel mobility, which can aid in diagnosis of underlying condition
○Cine function useful to store dynamic images for review
•Abnormal bowel identified as thickened or dilated segments
○Thickened bowel demonstrates reduced peristalsis
–Stands out among normally peristalsing loops of normal bowel
Abdomen Anatomy:
69
Anatomy: Abdomen
Bowel
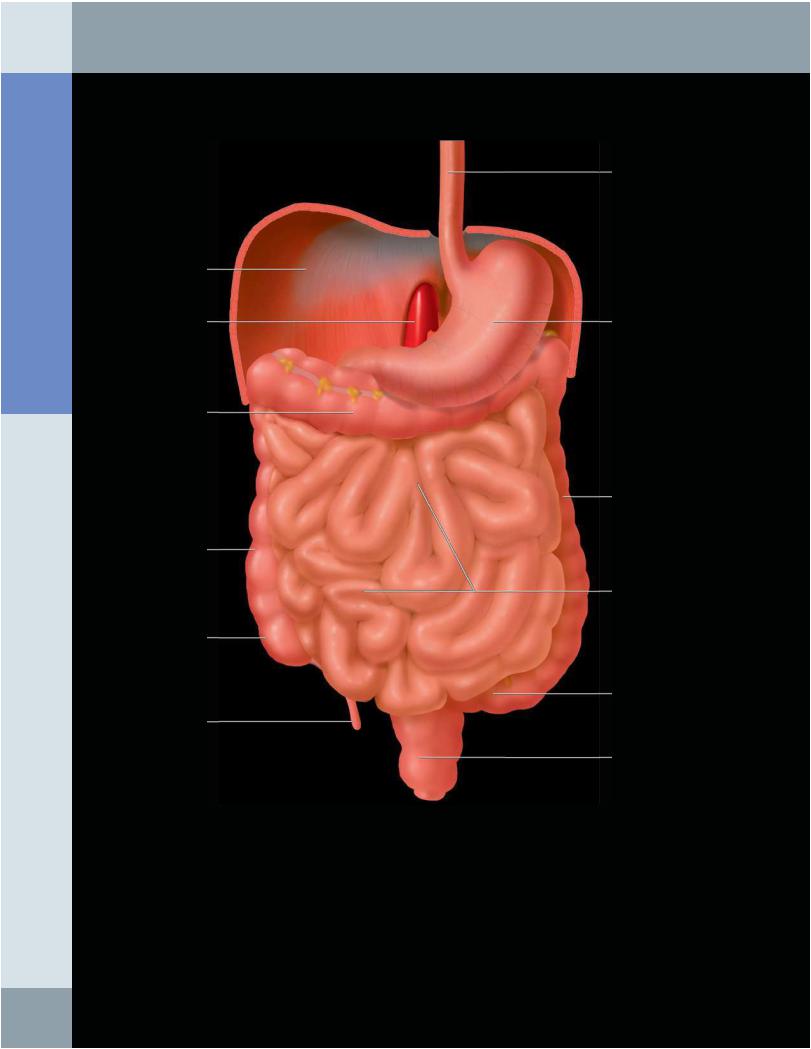
GASTROINTESTINAL TRACT IN SITU
Esophagus
Right hemidiaphragm
Aorta |
Stomach |
Transverse colon
Descending colon
Ascending colon
Small intestine
Cecum
Sigmoid
Appendix
Rectum
Graphic shows the gastrointestinal tract in situ. The liver and the greater omentum have been removed. Note the relatively central location of the small intestine compared with the peripherally located large intestine. Most of the bowel segments are intraperitoneal, apart from the 2nd to 4th parts of the duodenum, the ascending and descending colon, and middle 1/3 of the rectum, which are retroperitoneal. The distal 1/3 of the rectum is extraperitoneal.
70
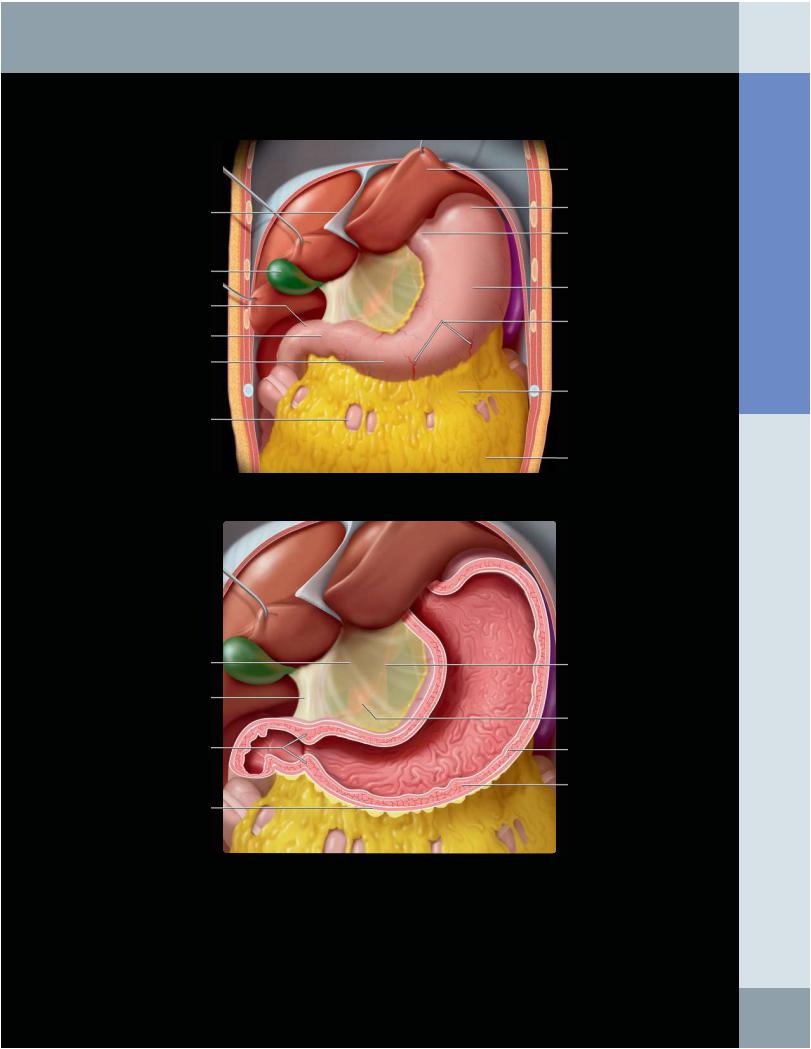
Bowel
Falciform ligament
Gallbladder
Duodenal bulb
Pylorus
Antrum
Transverse colon
Hepatogastric ligament
Hepatoduodenal ligament
Pyloric sphincter
Outer(longitudinal) muscle layer
STOMACH AND DUODENUM IN SITU
Liver (left lobe)
Fundus
Cardia
Body
Gastroepiploic artery branches
Gastrocolic ligament
Greater omentum
Left gastric artery
Celiac artery
Inner (oblique) muscle layer
Middle (circular) muscle layer
(Top) Graphic shows the stomach and proximal duodenum in situ. The liver and gallbladder have been retracted upward. Note that the lesser curvature and anterior wall of the stomach touch the underside of the liver and the gallbladder abuts the duodenal bulb. The greater curvature is attached to the transverse colon by the gastrocolic ligament, which continues inferiorly as the greater omentum, covering most of the colon and small bowel. (Bottom) Graphic shows the lesser omentum extending from the stomach to the porta hepatis, divided into the broader and thinner hepatogastric ligament and the thicker hepatoduodenal ligament. The lesser omentum carries the portal vein, hepatic artery, common bile duct, and lymph nodes. The free edge of the lesser omentum forms the ventral margin of the epiploic foramen. Note the layers of gastric muscle; the middle circular layer is thickest.
Abdomen Anatomy:
71
Anatomy: Abdomen
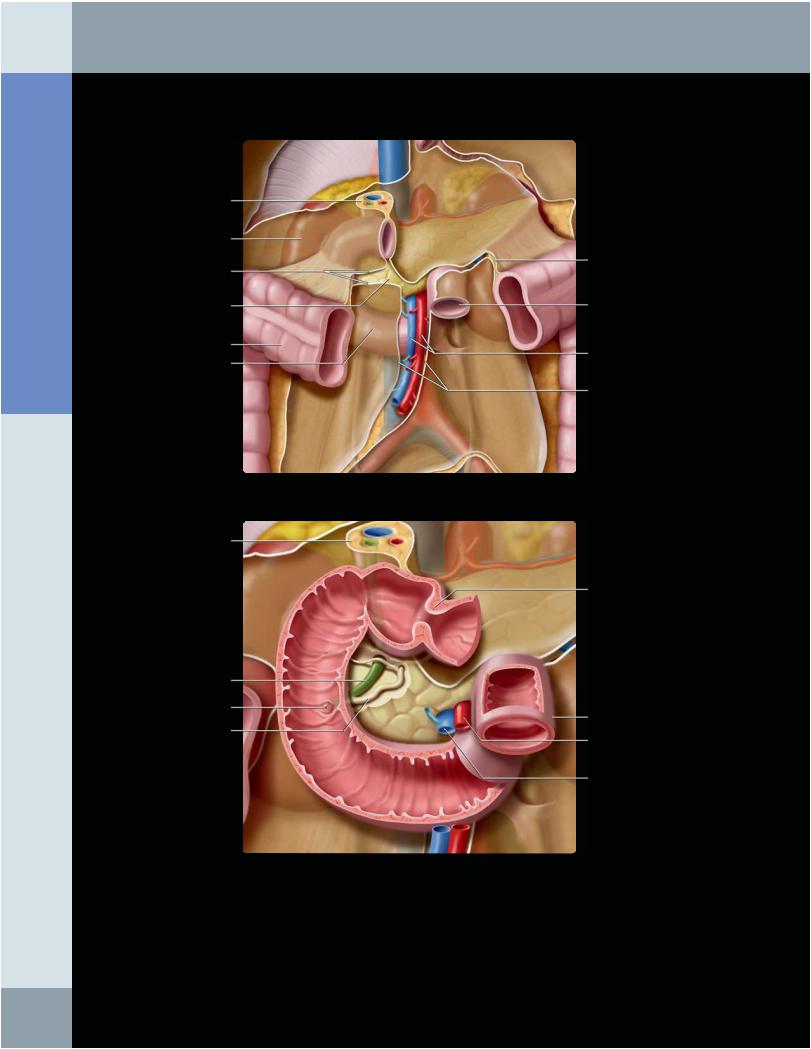
DUODENUM
Hepatoduodenal ligament
Right kidney
Root of transverse mesocolon
Pancreas
Transverse colon Duodenum (3rd portion)
Hepatoduodenal ligament
Common bile duct
Major papilla (of Vater)
Pancreatic duct
Bowel
Transverse mesocolon
Jejunum
Superior mesenteric artery and vein
Root of small bowel mesentery
Pylorus
Proximal jejunum
Superior mesenteric artery
Superior mesenteric vein
(Top) The duodenum is retroperitoneal, except for the bulb (1st part). The proximal jejunum is intraperitoneal. The hepatoduodenal ligament attaches the duodenum to the porta hepatis and contains the portal triad (bile duct, hepatic artery, portal vein). The root of the transverse mesocolon and mesentery both cross the duodenum. The 3rd portion of the duodenum crosses in front of the aorta and inferior vena cava (IVC) and behind the superior mesenteric vessels. The 2nd portion of the duodenum is attached to the pancreatic head and lies close to the hilum of the right kidney. (Bottom) Graphic shows the duodenal bulb suspended by the hepatoduodenal ligament. The duodenal-jejunal flexure is suspended by the ligament of Treitz, an extension of the right crus. The major pancreaticobiliary papilla enters the medial wall of the 2nd portion of the duodenum.
72

Bowel
SMALL INTESTINE
Celiac artery
Superior mesenteric artery
Ileocolic artery
Liver
Stomach
Transverse colon
Greater omentum
Jejunal straight arteries
Jejunal arterial arcades
Ileal straight arteries
Pancreas
Superior mesenteric artery
Duodenum (3rd part)
Aorta
Inferior vena cava
Small bowel loops
(Top) Graphic shows the vascular supply of the entire small intestine from the superior mesenteric artery (SMA). The small bowel segments are displaced inferiorly. The SMA arises from the anterior abdominal aorta and gives off the inferior pancreaticoduodenal branch that supplies the duodenum and pancreas. Arising from the left side of the SMA are numerous branches to the jejunum and ileum. Jejunal arteries are generally larger and longer than those of the ileum. After a straight course, the arteries form multiple intercommunicating curvilinear arcades. (Bottom) Graphic shows the sagittal section of the central abdomen, revealing the jejunum and ileum suspended in a radial pattern by the mesentery. Note the overlying greater omentum attached from the inferior portion of the stomach to drape the small bowel segments and transverse colon.
Abdomen Anatomy:
73
