
- •CONTENTS
- •PREFACE
- •ABBREVIATIONS
- •GENERAL AND COLORECTAL
- •CASE 1:
- •ANSWER 1
- •CASE 2:
- •ANSWER 2
- •CASE 3:
- •ANSWER 3
- •CASE 4:
- •ANSWER 4
- •CASE 5:
- •ANSWER 5
- •CASE 6:
- •ANSWER 6
- •CASE 7:
- •ANSWER 7
- •CASE 8:
- •ANSWER 8
- •CASE 9:
- •ANSWER 9
- •CASE 10:
- •ANSWER 10
- •CASE 11:
- •ANSWER 11
- •CASE 12:
- •ANSWER 12
- •CASE 13:
- •ANSWER 13
- •CASE 14:
- •ANSWER 14
- •CASE 15:
- •ANSWER 15
- •CASE 16:
- •ANSWER 16
- •CASE 17:
- •ANSWER 17
- •CASE 18:
- •ANSWER 18
- •CASE 19:
- •ANSWER 19
- •CASE 20:
- •ANSWER 20
- •UPPER GASTROINTESTINAL
- •CASE 21:
- •ANSWER 21
- •CASE 22:
- •ANSWER 22
- •CASE 23:
- •ANSWER 23
- •CASE 24:
- •ANSWER 24
- •CASE 25:
- •ANSWER 25
- •CASE 26:
- •ANSWER 26
- •CASE 27:
- •ANSWER 27
- •CASE 28:
- •ANSWER 28
- •CASE 29:
- •ANSWER 29
- •CASE 30:
- •ANSWER 30
- •CASE 31:
- •ANSWER 31
- •CASE 32:
- •ANSWER 32
- •CASE 33:
- •ANSWER 33
- •CASE 34:
- •ANSWER 34
- •CASE 35:
- •ANSWER 35
- •CASE 36:
- •ANSWER 36
- •BREAST AND ENDOCRINE
- •CASE 37:
- •ANSWER 37
- •CASE 38:
- •ANSWER 38
- •CASE 39:
- •ANSWER 39
- •CASE 40:
- •ANSWER 40
- •CASE 41:
- •VASCULAR
- •CASE 42:
- •ANSWER 42
- •CASE 43:
- •ANSWER 43
- •CASE 44:
- •ANSWER 44
- •CASE 45:
- •ANSWER 45
- •CASE 46:
- •ANSWER 46
- •CASE 47:
- •ANSWER 47
- •CASE 48:
- •ANSWER 48
- •CASE 49:
- •ANSWER 49
- •CASE 50:
- •ANSWER 50
- •CASE 51:
- •ANSWER 51
- •CASE 52:
- •ANSWER 52
- •CASE 53:
- •ANSWER 53
- •CASE 54:
- •ANSWER 54
- •CASE 55:
- •ANSWER 55
- •CASE 56:
- •ANSWER 56
- •UROLOGY
- •CASE 57:
- •ANSWER 57
- •CASE 58:
- •ANSWER 58
- •CASE 59:
- •ANSWER 59
- •CASE 60:
- •ANSWER 60
- •CASE 61:
- •ANSWER 61
- •CASE 62:
- •ANSWER 62
- •CASE 63:
- •ANSWER 63
- •CASE 64:
- •ANSWER 64
- •ORTHOPAEDIC
- •CASE 65:
- •ANSWER 65
- •CASE 66:
- •ANSWER 66
- •CASE 67:
- •ANSWER 67
- •CASE 68:
- •ANSWER 68
- •CASE 69:
- •Questions
- •ANSWER 69
- •CASE 70:
- •ANSWER 70
- •CASE 71:
- •ANSWER 71
- •CASE 72:
- •ANSWER 72
- •CASE 73:
- •ANSWER 73
- •CASE 74:
- •ANSWER 74
- •CASE 75:
- •ANSWER 75
- •CASE 76:
- •ANSWER 76
- •CASE 77:
- •ANSWER 77
- •CASE 78:
- •ANSWER 78
- •CASE 79:
- •ANSWER 79
- •CASE 80:
- •ANSWER 80
- •CASE 81:
- •ANSWER 81
- •EAR, NOSE AND THROAT
- •CASE 82:
- •ANSWER 82
- •CASE 83:
- •ANSWER 83
- •CASE 84:
- •ANSWER 84
- •CASE 85:
- •ANSWER 85
- •NEUROSuRGERY
- •CASE 86:
- •ANSWER 86
- •CASE 87:
- •ANSWER 87
- •CASE 88:
- •ANSWER 88
- •CASE 89:
- •ANSWER 89
- •ANAESTHESIA
- •CASE 90:
- •ANSWER 90
- •CASE 91:
- •ANSWER 91
- •CASE 92:
- •ANSWER 92
- •CASE 93:
- •ANSWER 93
- •CASE 94:
- •ANSWER 94
- •POSTOPERATIVE COMPLICATIONS
- •CASE 95:
- •ANSWER 95
- •CASE 96:
- •ANSWER 96
- •CASE 97:
- •ANSWER 97
- •CASE 98:
- •ANSWER 98
- •CASE 99:
- •ANSWER 99
- •CASE 100:
- •ANSWER 100

100 Cases in Surgery
ANSWER 32
The patient has chronic pancreatitis. The x-ray demonstrates pancreatic calcification (arrow in Figure 32.2).
Figure 32.2 plain x-ray of the abdomen. arrow shows pancreatic calcification.
Chronic pancreatitis is an irreversible inflammation causing pancreatic fibrosis and calcification. Patients usually present with chronic abdominal pain and normal or mildly elevated pancreatic enzyme levels. The pancreas may have lost its endocrine and exocrine function, leading to diabetes mellitus and steatorrhea.
!Causes of chronic pancreatitis
•Alcohol dependence: most common cause
•Idiopathic: approximately 30 per cent of cases
•Cholelithiasis: this is the most common cause of acute pancreatitis, but it is associated with chronic pancreatitis in less than 25 per cent of cases
•Pancreatic duct strictures
•Pancreatic trauma
•Hereditary pancreatitis: mutations in the gene for cationic trypsinogen on chromosome 7 appear to be involved in 60–75 per cent of cases of hereditary pancreatitis
•Recurrent acute pancreatitis
•Cystic fibrosis: an autosomal recessive disorder accounting for a small percentage of patients with chronic pancreatitis
•Congenital causes: pancreas divisum can cause chronic pancreatitis, although this is rare
•Autoimmune disorders: Sjögren’s syndrome, primary biliary cirrhosis, and renal tubular acidosis
•Other conditions: hyperlipidaemia, hyperparathyroidism, and uraemia can cause chronic pancreatitis
72
Upper Gastrointestinal
Diagnostic studies may be normal in the early stages of chronic pancreatitis. The inflammatory changes can only be diagnosed on histological analysis of a biopsy. The mean age of onset is 40 years, with a male preponderance of 4:1. Pancreatic calcification is observed in approximately one-third of plain x-rays of patients with chronic pancreatitis (arrow in Figure 32.2). ERCP provides an accurate visualization of the pancreatic ductal system and is useful for diagnosing chronic pancreatitis. One limitation of ERCP is that it cannot be used to evaluate the pancreatic parenchyma, and histologically proven chronic pancreatitis can be found after a normal ERCP. MRCP imaging provides information on the pancreatic parenchyma and adjacent abdominal viscera. Pancreatic function tests can provide useful information using the serum trypsin or faecal fat levels.
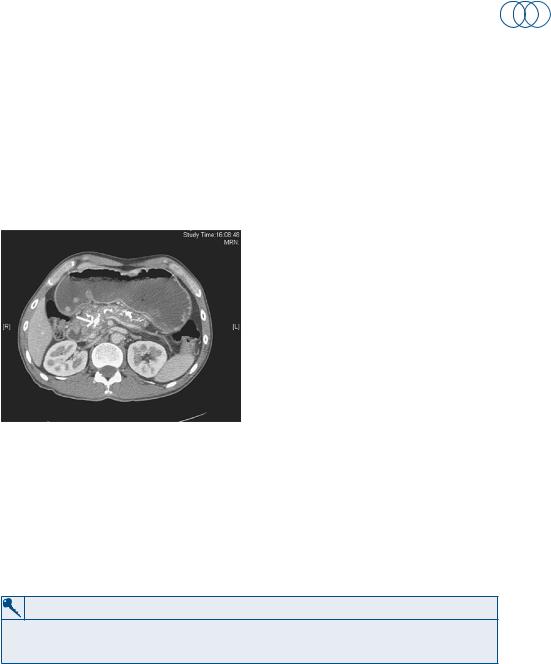
Figure 32.3 Computerized tomography showing changes consistent with chronic pancreatitis.
Treatment should primarily be a low-fat diet and abstinence from alcohol. Pancreatic enzyme supplements (creon) may reduce steatorrhoea. If conventional medical therapy is unsuccessful and the patient has severe intractable pain, coeliac ganglion blockade can be considered. Surgery is associated with significant morbidity and mortality and relieves symptoms in approximately 75 per cent of patients. It does not result in the return of normal endocrine and exocrine function. Surgery can be performed to bypass an obstructing lesion (pancreaticojejunostomy) or to remove the damaged gland (pancreaticoduodenectomy or distal pancreatectomy).
KEY POINTS
•thirty per cent of cases of chronic pancreatitis are idiopathic.
•Chronic pancreatitis increases the risk of pancreatic carcinoma.
73
This page intentionally left blank

Upper Gastrointestinal
CASE 33: abDominal pain anD jaunDiCe
history
A GP has referred a 64-year-old woman to the general surgical team on call. She has been complaining of pain in the upper part of the abdomen and generalized itching. Her daughter has also noticed a yellowish discolouration of her skin. The symptoms began about a week ago and became gradually worse. On further questioning she reports passing dark urine and pale stools for the last few days. She is usually fit and well, does not drink alcohol and denies any recent foreign travel.
examination
The patient is clinically jaundiced and tender in the right upper abdomen. The liver is not enlarged and rectal examination reveals pale stool on the glove. Her temperature is 37°C, blood pressure 130/80 mmHg and pulse rate 72/min. Bilirubin is detected on urinalysis.
INVESTIGATIONS
|
|
Normal |
haemoglobin |
12 g/dl |
11.5–16.0 g/dl |
mean cell volume |
80 fl |
76–96 fl |
White cell count |
11.5 × 109/l |
4.0–11.0 × 109/l |
platelets |
315 × 109/l |
150–400 × 109/l |
Sodium |
137 mmol/l |
135–145 mmol/l |
potassium |
4.2 mmol/l |
3.5–5.0 mmol/l |
urea |
6 mmol/l |
2.5–6.7 mmol/l |
Creatinine |
62 μmol/l |
44–80 μmol/l |
amylase |
72 iu/dl |
0–100 iu/dl |
alp |
556 iu/l |
35–110 iu/l |
aSt |
45 iu/l |
5–35 iu/l |
ggt |
127 iu/l |
11–51 iu/l |
albumin |
38 g/l |
35–50 g/l |
bilirubin |
122 mmol/l |
3–17 mmol/l |
Questions
•What do the blood results show?
•What are the causes of this condition?
•What are the options for investigation and treatment?
75
