
- •Preface and Acknowledgments
- •Contents
- •Contributors
- •1: Embryology for Urologists
- •Introduction
- •Renal Development
- •Pronephros
- •Mesonephros
- •Metanephros
- •Development of the Collecting System
- •Critical Steps in Further Development
- •Anomalies of the Kidney
- •Renal Agenesis
- •Renal Aplasia
- •Renal Hypoplasia
- •Renal Ectopia
- •Renal Fusion
- •Ureteral Development
- •Anomalies of Origin
- •Anomalies of Number
- •Incomplete Ureteral Duplication
- •Complete Ureteral Duplication
- •Ureteral Ectopia
- •Embryology of Ectopia
- •Clinical Correlation
- •Location of Ectopic Ureteral Orifices – Male (in Descending Order According to Incidence)
- •Symptoms
- •Ureteroceles
- •Congenital Ureteral Obstruction
- •Pipestem Ureter
- •Megaureter-Megacystis Syndrome
- •Prune Belly Syndrome
- •Vascular Ureteral Obstructions
- •Division of the Urogenital Sinus
- •Bladder Development
- •Urachal Anomalies
- •Cloacal Duct Anomalies
- •Other Bladder Anomalies
- •Bladder Diverticula
- •Bladder Extrophy
- •Gonadal Development
- •Testicular Differentiation
- •Ovarian Differentiation
- •Gonadal Anomalies
- •Genital Duct System
- •Disorders of Testicular Function
- •Female Ductal Development
- •Prostatic Urethral Valves
- •Gonadal Duct Anomalies
- •External Genital Development
- •Male External Genital Development
- •Female External Genital Development
- •Anomalies of the External Genitalia
- •References
- •2: Gross and Laparoscopic Anatomy of the Upper Urinary Tract and Retroperitoneum
- •Overview
- •The Kidneys
- •The Renal Vasculature
- •The Renal Collecting System
- •The Ureters
- •Retroperitoneal Lymphatics
- •Retroperitoneal Nerves
- •The Adrenal Glands
- •References
- •3: Gross and Laparoscopic Anatomy of the Lower Urinary Tract and Pelvis
- •Introduction
- •Female Pelvis
- •Male Pelvis
- •Pelvic Floor
- •Urinary Bladder
- •Urethra
- •Male Urethra
- •Female Urethra
- •Sphincter Mechanisms
- •The Bladder Neck Component
- •The Urethral Wall Component
- •The External Urethral Sphincter
- •Summary
- •References
- •4: Anatomy of the Male Reproductive System
- •Testis and Scrotum
- •Spermatogenesis
- •Hormonal Regulation of Spermatogenesis
- •Genetic Regulation of Spermatogenesis
- •Epididymis and Ductus Deferens
- •Accessory Sex Glands
- •Prostate
- •Seminal Vesicles
- •Bulbourethral Glands
- •Penis
- •Erection and Ejaculation
- •References
- •5: Imaging of the Upper Tracts
- •Anatomy of the Upper Tracts and Introduction to Imaging Modalities
- •Introduction
- •Renal Upper Tract Basic Anatomy
- •Modalities Used for Imaging the Upper Tracts
- •Ultrasound
- •Radiation Issues
- •Contrast Issues
- •Renal and Upper Tract Tumors
- •Benign Renal Tumors
- •Transitional Cell Carcinoma
- •Renal Mass Biopsy
- •Renal Stone Disease
- •Ultrasound
- •Plain Radiographs and IVU
- •Renal Cystic Disease
- •Benign Renal Cysts
- •Hereditary Renal Cystic Disease
- •Complex Renal Cysts
- •Renal Trauma
- •References
- •Introduction
- •Pathophysiology
- •Susceptibility and Resistance
- •Epidemiological Breakpoints
- •Clinical Breakpoints
- •Pharmacodynamic Parameters
- •Pharmacokinetic Parameters
- •Fosfomycin
- •Nitrofurantoin
- •Pivmecillinam
- •b-Lactam-Antibiotics
- •Penicillins
- •Cephalosporins
- •Carbapenems
- •Aminoglycosides
- •Fluoroquinolones
- •Trimethoprim, Cotrimoxazole
- •Glycopeptides
- •Linezolid
- •Conclusion
- •References
- •7: An Overview of Renal Physiology
- •Introduction
- •Body Fluid Compartments
- •Regulation of Potassium Balance
- •Regulation of Acid–Base Balance
- •Diuretics
- •Suggested Reading
- •8: Ureteral Physiology and Pharmacology
- •Ureteral Anatomy
- •Modulation of Peristalsis
- •Ureteral Pharmacology
- •Conclusion
- •References
- •Introduction
- •Afferent Signaling Pathways
- •Efferent Signaling
- •Parasympathetic Nerves
- •Sympathetic Nerves
- •Vesico-Spinal-Vesical Micturition Reflex
- •Peripheral Targets
- •Afferent Signaling Mechanisms
- •Urothelium
- •Myocytes
- •Cholinergic Receptors
- •Muscarinic Receptors
- •Nicotinic Receptors
- •Adrenergic Receptors (ARs)
- •a-Adrenoceptors
- •b-Adrenoceptors
- •Transient Receptor Potential (TRP) Receptors
- •Phosphodiesterases (PDEs)
- •CNS Targets
- •Opioid Receptors
- •Serotonin (5-HT) Mechanisms
- •g-Amino Butyric Acid (GABA) Mechanisms
- •Gabapentin
- •Neurokinin and Neurokinin Receptors
- •Summary
- •References
- •10: Pharmacology of Sexual Function
- •Introduction
- •Sexual Desire/Arousal
- •Endocrinology
- •Steroids in the Male
- •Steroids in the Female
- •Neurohormones
- •Neurotransmitters
- •Dopamine
- •Serotonin
- •Pharmacological Strategies
- •CNS Drugs
- •Enzyme-inducing Antiepileptic Drugs
- •Erectile Function
- •Ejaculatory Function
- •Premature Ejaculation
- •Abnormal Ejaculation
- •Conclusions
- •References
- •Epidemiology
- •Calcium-Based Urolithiasis
- •Uric Acid Urolithiasis
- •Infectious Urolithiasis
- •Cystine-Based Urolithiasis
- •Aims
- •Who Deserves Metabolic Evaluation?
- •Metabolic Workup for Stone Producers
- •Medical History and Physical Examination
- •Stone Analysis
- •Serum Chemistry
- •Urine Evaluation
- •Urine Cultures
- •Urinalysis
- •Twenty-Four Hour Urine Collections
- •Radiologic Imaging
- •Medical Management
- •Conservative Management
- •Increased Fluid Intake
- •Citrus Juices
- •Dietary Restrictions
- •Restricted Oxalate Diet
- •Conservative Measures
- •Selective Medical Therapy
- •Absorptive Hypercalciuria
- •Thiazide
- •Orthophosphate
- •Renal Hypercalciuria
- •Primary Hyperparathyroidism
- •Hyperuricosuric Calcium Oxalate Nephrolithiasis
- •Enteric Hyperoxaluria
- •Hypocitraturic Calcium Oxalate Nephrolithiasis
- •Distal Renal Tubular Acidosis
- •Chronic Diarrheal States
- •Thiazide-Induced Hypocitraturia
- •Idiopathic Hypocitraturic Calcium Oxalate Nephrolithiasis
- •Hypomagnesiuric Calcium Nephrolithiasis
- •Gouty Diathesis
- •Cystinuria
- •Infection Lithiasis
- •Summary
- •References
- •12: Molecular Biology for Urologists
- •Introduction
- •Inherited Changes in Cancer Cells
- •VEGR and Cell Signaling
- •Targeting mTOR
- •Conclusion
- •References
- •13: Chemotherapeutic Agents for Urologic Oncology
- •Introduction
- •Bladder Cancer
- •Muscle Invasive Bladder Cancer
- •Metastatic Bladder Cancer
- •Conclusion
- •Prostate Cancer
- •Other Chemotherapeutic Drugs or Combinations for Treating HRPC
- •Conclusion
- •Renal Cell Carcinoma
- •Chemotherapy
- •Immunotherapy
- •Angiogenesis Inhibitor Drugs
- •Conclusion
- •Testicular Cancer
- •Stage I Seminoma
- •Stage I non-seminomatous Germ Cell Tumours (NSGCT)
- •Metastatic Germ Cell Tumours
- •Low-Volume Metastatic Disease (Stage II A/B)
- •Advanced Metastatic Disease
- •Salvage Chemotherapy for Relapsed or Refractory Disease
- •Conclusion
- •Penile Cancer
- •Side Effects of Chemotherapy
- •Conclusion
- •References
- •14: Tumor and Transplant Immunology
- •Antibodies
- •Cytotoxic and T-helper Cells
- •Immunosuppression
- •Induction Therapy
- •Maintenance Therapy
- •Rejection
- •Posttransplant Lymphoproliferative Disease
- •Summary
- •References
- •15: Pathophysiology of Renal Obstruction
- •Causes of Renal Obstruction
- •Effects on Prenatal Development
- •Prenatal Hydronephrosis
- •Spectrum of Renal Abnormalities
- •Renal Functional Changes
- •Renal Growth/Counterbalance
- •Vascular Changes
- •Inflammatory Mediators
- •Glomerular Development Changes
- •Mechanical Stretch of Renal Tubules
- •Unilateral Versus Bilateral
- •Limitations of Animal Models
- •Future Research
- •Issues in Patient Management
- •Diagnostic Imaging
- •Ultrasound
- •Intravenous Urography
- •Antegrade Urography and the Whitaker Test
- •Nuclear Renography
- •Computed Tomography
- •Magnetic Resonance Urography
- •Hypertension
- •Postobstructive Diuresis
- •References
- •Introduction
- •The Normal Lower Urinary Tract
- •Anatomy
- •Storage Function
- •Voiding Function
- •Neural Control
- •Symptoms
- •Flow Rate and Post-void Residual
- •Voiding Cystometry
- •Male
- •Female
- •Neurourology
- •Conclusions
- •References
- •17: Urologic Endocrinology
- •The Testis
- •Normal Androgen Metabolism
- •Epidemiological Aspects
- •Prostate
- •Brain
- •Muscle Mass and Adipose Tissue
- •Bones
- •Ematopoiesis
- •Metabolism
- •Cardiovascular System
- •Clinical Assessment
- •Biochemical Assessment
- •Treatment Modalities
- •Oral Preparations
- •Parenteral Preparations
- •Transdermal Preparations
- •Side Effects and Treatment Monitoring
- •Body Composition
- •Cognitive Decline
- •Bone Metabolism
- •The Kidneys
- •Endocrine Functions of the Kidney
- •Erythropoietin
- •Calcitriol
- •Renin
- •Paraneoplastic Syndromes
- •Hypercalcemia
- •Hypertension
- •Polycythemia
- •Other Endocrine Abnormalities
- •References
- •General Physiology
- •Prostate Innervation
- •Summary
- •References
- •Wound Healing
- •Inflammation
- •Proliferation
- •Remodeling
- •Principles of Plastic Surgery
- •Tissue Characteristics
- •Grafts
- •Flap
- •References
- •Lower Urinary Tract Symptoms
- •Storage Phase
- •Voiding Phase
- •Return to Storage Phase
- •Urodynamic Parameters
- •Urodynamic Techniques
- •Volume Voided Charts
- •Pad Testing
- •Typical Test Schedule
- •Uroflowmetry
- •Post Voiding Residual
- •Further Diagnostic Evaluation of Patients
- •Cystometry with or Without Video
- •Cystometry
- •Videocystometrography (Cystometry + Cystourethrography)
- •Cystometric Findings
- •Comment:
- •Measurements During the Storage Phase:
- •Measurements During the Voiding Phase:
- •Abnormal Function
- •Disorders of Sensation
- •Causes of Hypersensitive Bladder Sensation
- •Causes of Hyposensitive Bladder Sensation
- •Disorders of Detrusor Motor Function
- •Bladder Outflow Tract Dysfunction
- •Detrusor–Urethral Dyssynergia
- •Detrusor–Bladder Neck Dyssynergia
- •Detrusor–Sphincter Dyssynergia
- •Complex Urodynamic Investigation
- •Urethral Pressure Measurement
- •Technique
- •Neurophysiological Evaluation
- •Conclusion
- •References
- •Endoscopy
- •Cystourethroscopy
- •Ureteroscopy and Ureteropyeloscopy
- •Nephroscopy
- •Virtual Reality Simulators
- •Lasers
- •Clinical Application of Lasers
- •Condylomata Acuminata
- •Urolithiasis
- •Benign Prostatic Hyperplasia
- •Ureteral and Urethral Strictures
- •Conclusion
- •References
- •Introduction
- •The Prostatitis Syndromes
- •The Scope of the Problem
- •Category III CP/CPPS
- •The Goal of Treatment
- •Conservative Management
- •Drug Therapy
- •Antibiotics
- •Anti-inflammatories
- •Alpha blockers
- •Hormone Therapies
- •Phytotherapies
- •Analgesics, muscle relaxants and neuromodulators
- •Surgery
- •A Practical Management Plan
- •References
- •Orchitis
- •Definition and Etiology
- •Clinical Signs and Symptoms
- •Diagnostic Evaluation
- •Treatment of Infectious Orchitis
- •Epididymitis
- •Definition and Etiology
- •Clinical Signs and Symptoms
- •Diagnostic Evaluation of Epididymitis
- •Treatment of Acute Epididymitis
- •Treatment of Chronic Epididymitis
- •Treatment of Spermatic Cord Torsion
- •Fournier’s Gangrene
- •Definition and Etiology
- •Risk Factors
- •Clinical Signs and Symptoms
- •Diagnostic Evaluation
- •Treatment
- •References
- •Fungal Infections
- •Candidiasis
- •Aspergillosis
- •Cryptococcosis
- •Blastomycosis
- •Coccidioidomycosis
- •Histoplasmosis
- •Radiographic Findings
- •Treatment
- •Tuberculosis
- •Clinical Manifestations
- •Diagnosis
- •Treatment
- •Schistosomiasis
- •Clinical Manifestations
- •Diagnosis
- •Treatment
- •Filariasis
- •Clinical Manifestations
- •Diagnosis
- •Treatment
- •Onchocerciasis
- •References
- •25: Sexually Transmitted Infections
- •Introduction
- •STIs Associated with Genital Ulcers
- •Herpes Simplex Virus
- •Diagnosis
- •Treatment
- •Chancroid
- •Diagnosis
- •Treatment
- •Syphilis
- •Diagnosis
- •Treatment
- •Lymphogranuloma Venereum
- •Diagnosis
- •Treatment
- •Chlamydia
- •Diagnosis
- •Treatment
- •Gonorrhea
- •Diagnosis
- •Treatment
- •Trichomoniasis
- •Diagnosis
- •Treatment
- •Human Papilloma Virus
- •Diagnosis
- •Treatment
- •Scabies
- •Diagnosis
- •Treatment
- •References
- •26: Hematuria: Evaluation and Management
- •Introduction
- •Classification of Hematuria
- •Macroscopic Hematuria
- •Microscopic Hematuria
- •Dipstick Hematuria
- •Pseudohematuria
- •Factitious Hematuria
- •Menstruation
- •Aetiology
- •Malignancy
- •Urinary Calculi
- •Infection and Inflammation
- •Benign Prostatic Hyperplasia
- •Trauma
- •Drugs
- •Nephrological Causes
- •Assessment
- •History
- •Examination
- •Investigations
- •Dipstick Urinalysis
- •Cytology
- •Molecular Tests
- •Blood Tests
- •Flexible Cystoscopy
- •Upper Urinary Tract Evaluation
- •Renal USS
- •KUB Abdominal X-Ray
- •Intravenous Urography (IVU)
- •Computed Tomography (CT)
- •Retrograde Urogram Studies
- •Magnetic Resonance Imaging (MRI)
- •Additional Tests and Renal Biopsy
- •Intractable Hematuria
- •Loin Pain Hematuria Syndrome
- •References
- •27: Benign Prostatic Hyperplasia (BPH)
- •Historical Background
- •Pathophysiology
- •Patient Assessment
- •Treatment of BPH
- •Watchful Waiting
- •Drug Therapy
- •Interventional Therapies
- •Conclusions
- •References
- •28: Practical Guidelines for the Treatment of Erectile Dysfunction and Peyronie´s Disease
- •Erectile Dysfunction
- •Introduction
- •Diagnosis
- •Basic Evaluation
- •Cardiovascular System and Sexual Activity
- •Optional Tests
- •Treatment
- •Medical Treatment
- •Oral Agents
- •Phosphodiesterase Type 5 (PDE 5) Inhibitors
- •Nonresponders to PDE5 Inhibitors
- •Apomorphine SL
- •Yohimbine
- •Intracavernosal and Intraurethral Therapy
- •Intracavernosal Injection (ICI) Therapy
- •Intraurethral Therapy
- •Vacuum Constriction Devices
- •Surgical Therapy
- •Conclusion
- •Peyronie´s Disease (PD)
- •Introduction
- •Oral Drug Therapy
- •Intralesional Drug Therapy
- •Iontophoresis
- •Radiation Therapy
- •Surgical Therapy
- •References
- •29: Premature Ejaculation
- •Introduction
- •Epidemiology
- •Defining Premature Ejaculation
- •Voluntary Control
- •Sexual Satisfaction
- •Distress
- •Psychosexual Counseling
- •Pharmacological Treatment
- •On-Demand Treatment with Tramadol
- •Topical Anesthetics
- •Phosphodiesterase Inhibitors
- •Surgery
- •Conclusion
- •References
- •30: The Role of Interventional Management for Urinary Tract Calculi
- •Contraindications to ESWL
- •Complications of ESWL
- •PCNL Access
- •Instrumentation for PCNL
- •Nephrostomy Drains Post PCNL
- •Contraindications to PCNL
- •Complications of PCNL
- •Semirigid Ureteroscopy
- •Flexible Ureteroscopy
- •Electrohydraulic Lithotripsy (EHL)
- •Ultrasound
- •Ballistic Lithotripsy
- •Laser Lithotripsy
- •Ureteric Stents
- •Staghorn Calculi
- •Lower Pole Stones
- •Horseshoe Kidneys and Stones
- •Calyceal Diverticula Stones
- •Stones and PUJ Obstruction
- •Treatment of Ureteric Colic
- •Medical Expulsive Therapy (MET)
- •Intervention for Ureteric Stones
- •Stones in Pregnancy
- •Morbid Obesity
- •References
- •Anatomy and Function
- •Pathophysiology
- •Management
- •Optical Urethrotomy/Dilatation
- •Urethral Stents
- •Preoperative Assessment
- •Urethroplasty
- •Anastomotic Urethroplasty
- •Substitution Urethroplasty
- •Grafts Versus Flaps
- •Oral Mucosal Grafts
- •Tissue Engineering
- •Graft Position
- •Conclusion
- •References
- •32: Urinary Incontinence
- •Epidemiology and Risk Factors
- •Pathophysiology
- •Urge Incontinence
- •Conservative Treatments
- •Pharmacotherapy
- •Invasive/ Surgical Therapies
- •Stress Urinary Incontinence
- •Male SUI Therapies
- •Female SUI Therapies
- •Mixed Urinary Incontinence
- •Conclusions
- •References
- •33: Neurogenic Bladder
- •Introduction
- •Examination and Diagnostic Tests
- •History and Physical Examination
- •Imaging
- •Urodynamics (UDS)
- •Evoked Potentials
- •Classifications
- •Somatic Pathways
- •Brain Lesions
- •Cerebrovascular Accident (CVA)
- •Parkinson’s Disease (PD)
- •Multiple Sclerosis
- •Huntington’s Disease
- •Dementias
- •Normal Pressure Hydrocephalus (NPH)
- •Tumors
- •Psychiatric Disorders
- •Spinal Lesions and Pathology
- •Intervertebral Disk Prolapse
- •Spinal Cord Injury (SCI)
- •Transverse Myelitis
- •Peripheral Neuropathies
- •Metabolic Neuropathies
- •Pelvic Surgery
- •Treatment
- •Summary
- •References
- •34: Pelvic Prolapse
- •Introduction
- •Epidemiology
- •Anatomy and Pathophysiology
- •Evaluation and Diagnosis
- •Outcome Measures
- •Imaging
- •Urodynamics
- •Indications for Management
- •Biosynthetics
- •Surgical Management
- •Anterior Compartment Repair
- •Uterine/Apical Prolapse
- •Enterocele Repair
- •Conclusion
- •References
- •35: Urinary Tract Fistula
- •Introduction
- •Urogynecologic Fistula
- •Vesicovaginal Fistula
- •Etiology and Risk Factors
- •Clinical Factors
- •Evaluation and Diagnosis
- •Pelvic Examination
- •Cystoscopy
- •Imaging
- •Treatment
- •Conservative Management
- •Surgical Management
- •Urethrovaginal Fistula
- •Etiology and Presentation
- •Diagnosis and Management
- •Ureterovaginal Fistula
- •Etiology and Presentation
- •Diagnosis and Management
- •Vesicouterine Fistula
- •Etiology and Presentation
- •Diagnosis and Management
- •Uro-Enteric Fistula
- •Vesicoenteric Fistula
- •Pyeloenteric Fistula
- •Urethrorectal Fistula
- •References
- •36: Urologic Trauma
- •Introduction
- •Kidney
- •Expectant Management
- •Endovascular Therapy
- •Operative Intervention
- •Operative Management: Follow-up
- •Reno-Vascular Injuries
- •Pediatric Renal Injuries
- •Adrenal
- •Ureter
- •Diagnosis
- •Treatment
- •Delayed Diagnosis
- •Bladder and Posterior Urethra
- •Bladder Injuries: Initial Management
- •Bladder Injuries: Formal Repair
- •Anterior Urethral Trauma
- •Fractured Penis
- •Penile Amputation
- •Scrotal and Testicular Trauma
- •Imaging
- •CT-IVP (CT with Delayed Images)
- •Technique
- •Cystogram
- •Technique
- •Retrograde Urethrogram (RUG)
- •Technique
- •Retrograde Pyelogram (RPG)
- •Technique
- •One-Shot IVP
- •Technique
- •References
- •37: Bladder Cancer
- •Who Should Be Investigated?
- •Epidemiology
- •Risk Factors
- •Role of Screening
- •Signs and Symptoms
- •Imaging
- •Cystoscopy
- •Urine Tests
- •PDD-Assisted TUR
- •Pathology
- •NMIBC and Risk Groups
- •Intravesical Chemotherapy
- •Intravesical Immunotherapy
- •Immediate Cystectomy and CIS
- •Radical Cystectomy with Pelvic Lymph Node Dissection
- •sexual function-preserving techniques
- •Bladder-Preservation Treatments
- •Neoadjuvant Chemotherapy
- •Adjuvant Chemotherapy
- •Preoperative Radiotherapy
- •Follow-up After TUR in NMIBC
- •References
- •38: Prostate Cancer
- •Introduction
- •Epidemiology
- •Race
- •Geographic Variation
- •Risk Factors and Prevention
- •Family History
- •Diet and Lifestyle
- •Prevention
- •Screening and Diagnosis
- •Current Screening Recommendations
- •Biopsy
- •Pathology
- •Prognosis
- •Treatment of Prostate Cancer
- •Treatment for Localized Prostate Cancer (T1, T2)
- •Radical Prostatectomy
- •EBRT
- •IMRT
- •Brachytherapy
- •Treatment for Locally Advanced Prostate Cancer (T3, T4)
- •EBRT with ADT
- •Radical Prostatectomy
- •Androgen-Deprivation Therapy
- •Summary
- •References
- •39: The Management of Testis Cancer
- •Presentation and Diagnosis
- •Serum Tumor Markers
- •Primary Surgery
- •Testis Preserving Surgery
- •Risk Stratification
- •Surveillance Versus Primary RPLND
- •Primary RPLND
- •Adjuvant Treatment for High Risk
- •Clinical Stage 1 Seminoma
- •Risk-Stratified Adjuvant Treatment
- •Adjuvant Radiotherapy
- •Adjuvant Low Dose Chemotherapy
- •Primary Combination Chemotherapy
- •Late Toxicity
- •Salvage Strategies
- •Conclusion
- •References
- •Index
211
PathoPhysiology of lowEr Urinary tract obstrUction
Table 16.1. Voiding and post-micturition symptoms as defined |
suitable range, and is comparable to the typical |
|||||
by the international continence society (ics) standardisation |
voided volume on the individual’s frequency |
|||||
committee in 200217,18 |
|
volume chart, is a means by which to ascertain |
||||
Voiding symptoms |
|
that the flow rate test is representative and infor- |
||||
|
mative. Qmax is affected by VV, so nomograms |
|||||
slow stream |
the patient’s perception of |
|||||
have been developed to aid interpretation,exem- |
||||||
|
reduced urine flow, usually |
plified by the Liverpool nomograms for men |
||||
|
compared to previous |
and women22 and the Siroky nomogram for |
||||
|
performance or in |
men.23,24 At low VV, the bladder has insufficient |
||||
|
comparison with others |
|||||
|
volume to expel and Qmax may be reduced as a |
|||||
intermittent stream |
the urine flow stops and starts, |
|||||
result; nonetheless, informative conclusions can |
||||||
|
on one or more occasions, |
sometimes be drawn regardless of low VV.25 |
||||
|
during micturition |
Above 550 mL, the bladder starts to overfill and |
||||
hesitancy |
difficulty initiating micturition, |
efficiency declines,26 again causing artefactual |
||||
|
resulting in a delay in the |
reduction in Qmax. Failure of expulsion of the |
||||
|
onset of voiding after the |
entire bladder contents, leading to a PVR, signi- |
||||
|
individual is ready to pass |
fies inefficient bladder emptying; this suggests |
||||
|
urine |
either reduced bladder contractility or outlet |
||||
straining |
describes the muscular effort |
obstruction, or both. |
|
|
||
|
used to initiate, maintain, or |
|
The normal flow curve should have a rapid |
|||
|
improve the urinary stream |
upstroke, a clear Qmax, and decline quickly to |
||||
terminal dribble |
the term used to describe a |
end cleanly. Abnormal patterns include; |
||||
|
|
|
|
|||
|
prolonged final part of |
1. |
Prostatic (men): Characterized by a slow |
|||
|
micturition, when the flow |
|||||
|
|
upstroke, reduced Qmax, and prolonged down- |
||||
|
has slowed to a trickle/ |
|
||||
|
dribble |
|
stroke. |
|
|
|
Post-micturition symptoms |
2. |
Urethral stricture (men): the pattern has a |
||||
|
“plateau” appearance. |
|
|
|||
feeling of incomplete |
a self-explanatory term for a |
|
|
|
||
3. Intermittent (men or women): several peaks |
||||||
emptying |
feeling experienced by the |
|||||
|
in the flow curve can result if the patient |
|||||
|
individual after passing urine |
|
||||
|
|
strains during voiding. Likewise, a poorly |
||||
Post micturition |
involuntary loss of urine |
|
||||
|
sustained detrusor contraction causes the |
|||||
dribble |
immediately after he or she |
|
||||
|
stream to fluctuate. |
|
|
|||
|
has finished passing urine, |
|
|
|
||
|
usually after leaving the |
In men of the appropriate age group, a prostatic |
||||
|
toilet in men, or after rising |
|||||
|
pattern with a reduced Qmax |
when VV is ade- |
||||
|
from the toilet in women |
|||||
|
|
quate is suggestive of BOO but accuracy is inad- |
||||
|
|
equate by itself.27 Where Q |
max |
is above the |
||
|
|
expected range, outlet obstruction is unlikely. |
||||
is not so clear-cut,since relief of obstruction with |
However, sensitivity of flow rate testing by itself |
|||||
prostate resection surgery does not lead to reso- |
as a diagnostic test for BOO is inadequate. |
|||||
lution of storage urinary problems.21
Flow Rate and Post-void Residual
Flow rate machines measure flow volume over time and evaluate various parameters, of which the maximum flow rate (Qmax), flow pattern and post-void residual (PVR) volume are most widely used clinically. Findings have to be interpreted in the light of clinical circumstances; checking the voided volume (VV) falls into a
Voiding Cystometry
BOO is characterized by increased detrusor pressure and reduced urine flow rate.17 It is usually diagnosed by studying the synchronous values of flow rate and detrusor pressure, and is thus a urodynamic diagnosis.17
Consensus on what constitutes BOO in men has been achieved because of the relatively homogeneous nature of male BOO, reflecting

|
|
|
|
|
|
212 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Practical Urology: EssEntial PrinciPlEs and PracticE |
|
high prevalence of benign prostate enlargement |
2. An alternative nomogram has been proposed |
||||||
in older men, and the availability of transure- |
by a different group.39 |
||||||
thral resection surgery to relieve obstruction. |
3. The BOOI is applicable in men with benign |
||||||
This provided suitable circumstances to derive |
|||||||
prostate enlargement and no relevant neuro- |
|||||||
urodynamic nomograms28; the nomogram of |
|||||||
logical problem. Nonetheless, the parameters |
|||||||
Abrams and Griffiths was adopted and adapted |
|||||||
of the BOOI have been evaluated in women, |
|||||||
by the International Continence Society as a |
|||||||
such that the BOOI evaluated in conjunction |
|||||||
standardized criterion for diagnosing male |
|||||||
BOO. Thus a plot of Qmax |
against simultaneous |
with Qmax could be a usable urodynamic |
|||||
detrusor pressure (P |
Q |
) allows derivation of |
parameter of female BOO.40 A separate study |
||||
|
|
det |
max |
|
|
||
the bladder outlet obstruction index (BOOI), |
came to similar conclusions, but cut-off val- |
||||||
from which a definite diagnosis of BOO, equivo- |
ues were different.41 |
||||||
cal BOO or unobstructed can be made, as illus- |
4. An alternative compared women with ana- |
||||||
trated in Fig. 16.1. The concept superseded the |
|||||||
tomical BOO against women with stress uri- |
|||||||
earlier concept of a urethral resistance factor, |
|||||||
nary incontinence,42 with revisions using a |
|||||||
which originated from rigid tube hydrodyn- |
|||||||
amics. Since the urethra is an irregular and |
larger study group in 2000,43 and a control |
||||||
distensible conduit, whose walls and surround- |
group without stress incontinence in 2004.44 |
||||||
ings have active and passive elements which |
5. A panel of criteria derived during videouro- |
||||||
influence the flow, a resistance factor does not |
dynamic evaluation has been proposed based |
||||||
reliably provide a valid |
comparison |
between |
|||||
on study of a group of women clinically felt |
|||||||
patients.29 |
|
|
|
|
|||
|
|
|
|
to have BOO.45 |
|||
While measurements to derive a BOOI are |
|||||||
6. Area under the curve of detrusor pressure |
|||||||
generally made by invasive urodynamic testing, |
|||||||
during voiding, adjusted for voided volume, is |
|||||||
noninvasive techniques are now emerging30,31 |
|||||||
which may be able to derive an estimate of the |
a proposed parameter for diagnosing female |
||||||
detrusor pressure generating maximum flow |
BOO, though more work is needed.46 |
||||||
(i.e., with no catheter within the bladder lumen |
7. Abnormalities of free flow pattern are seen in |
||||||
to measure pressure). Penile cuff intermittent |
|||||||
a greater proportion of women subsequently |
|||||||
urethral compression32 is one approach and a |
|||||||
concluded to be obstructed on urodynamic |
|||||||
nomogram has been developed for the tech- |
|||||||
evaluation.47 |
|||||||
nique.33 Similar noninvasive pressure measure- |
|||||||
ment can be derived from a modified condom |
|
||||||
collecting device.34 Detrusor wall thickness is |
Causes of Bladder Outlet |
||||||
another parameter which may also indirectly |
|||||||
signify the presence of BOO.35,36 |
|
Obstruction |
|||||
Diagnosis of BOO in women has not been |
|||||||
standardized and remains an area of ongoing |
|
||||||
discussion.37 Proposals for urodynamic diagno- |
Male |
||||||
sis of BOO have been made as follows; |
|
The additional anatomical structure of the male |
|||||
1. Female BOO nomogram38; derived a nomo- |
|||||||
bladder outlet is the prostate gland, which |
|||||||
gram based on study of several hundred |
|||||||
encompasses the urethra between the genital |
|||||||
women defined as obstructed on clinical |
and urethral sphincters. With aging, the gland |
||||||
grounds, with quite a heterogeneous group of |
undergoes benign prostate enlargement (BPE), |
||||||
causative pathologies. The study estimated |
which can typically be shown to be a conse- |
||||||
the prevalence of female BOO at 6.5%. The |
quence of benign prostate hyperplasia (BPH); |
||||||
BPH can only be diagnosed where pathological |
|||||||
nomogram |
employs |
somewhat |
different |
||||
specimens by biopsy or resection are available.48 |
|||||||
parameters from the male BOOI, using the |
|||||||
The prevalence of BPH determined from autopsy |
|||||||
maximum |
detrusor |
pressure ascertained |
|||||
studies shows that it does not occur below the |
|||||||
during invasive urodynamics and the maxi- |
|||||||
age of 30 years and that almost 90% of men have |
|||||||
mum flow rate on free flow testing. |
|
developed BPH by their ninth decade.49 Likewise, |
|||||
213
PathoPhysiology of lowEr Urinary tract obstrUction
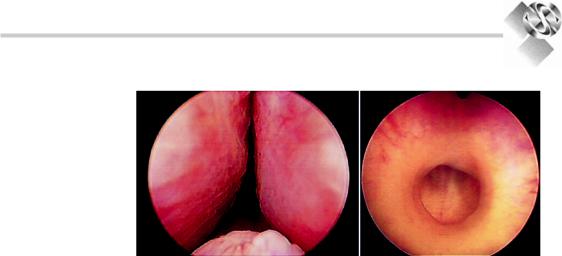
Figure 16.3. Left panel; a urethroscopic view of the intrusion of the lateral lobes and median lobe of a benignly enlarged prostate gland. Right panel; urethroscopic view of a dense fibrotic urethral stricture.
there is a steady increase in both LUTS50 and |
placebo, the alpha-blocker terazosin, the 5-alpha |
BPE,51 and all three processes are clearly inter- |
reductase inhibitor finasteride and combination |
related with ageing in men.52 |
therapy, suggested that factors other than BOO |
Implicitly, the intrusion of the prostate into |
alone almost certainly contribute to LUTS in |
the urethral lumen in BPE (Fig. 16.3) can be |
BPH. Recent studies using botulinum injections |
expected to provide a degree of anatomical |
within the prostate suggest that afferent nerve |
impedance to urine flow during voiding by |
activity may also be an element of LUTS in |
direct flow impedance, and by distortion of the |
BPE.58 Furthermore, the persistence of LUTS |
bladder outlet. Thus, flow rate does decline with |
after effective surgical management of BPE21 |
ageing in a population of men with BPE.25 The |
strongly suggests that age-related changes in |
role of anatomical impedance to flow is sup- |
bladder function contribute to male LUTS as a |
ported clinically by the response to treatment |
codependent variable alongside BPE.59 The |
aimed at reducing male sex hormones, which |
inherent difficulties of controlling for the range |
reduces the trophic factors giving rise to BPH |
of contributory variables means that the |
and thereby can partly reverse the enlargement. |
pathophysiology of male LUTS will remain a |
Within the prostate, the conversion of andro- |
source of considerable scientific debate for the |
gens to dihydrotestosterone by 5-alpha reductase |
foreseeable future. |
is a means by which this can be achieved.53 A |
Urethral strictures are another mechanism |
second contribution to BOO in BPE is the active |
giving rise to BOO in men. They comprise an |
contraction of smooth muscle in the prostate |
inelastic circumferential fibrous constriction |
stroma. The smooth muscle of the prostate |
(Fig. 16.3), and thereby differ from BPE in that |
expresses alpha-adrenergic receptors, falling |
there is not contribution of active muscle con- |
into at least two subtypes in the human pros- |
traction to the BOO. They can be present at any |
tate.54 Clinically, alpha-adrenergic antagonists |
point along the urethra; postsurgical bladder |
relax prostate smooth muscle, indicating a con- |
neck stenosis is a related situation. Strictures |
tribution of functional prostate muscle activity |
have comparatively little effect on lower urinary |
in BOO.55 On this basis, alpha-adrenergic antag- |
tract function until they cause significant con- |
onists and hormonal therapy may respectively |
striction of the lumen. Characteristically, the pat- |
decrease BOO by relaxing or shrinking the pros- |
tern of urine flow differs from that seen in BPE. |
tate. These clinical observations support the |
Strictures usually arise as a consequence of ure- |
hypothesis that there are both dynamic and |
thral trauma,which can be iatrogenic.Congenital |
static components of BOO associated with BPE. |
male urethral strictures have been described. |
The Olmstead County Study of Urinary |
Cobb’s collar is a congenital narrowing in the |
Symptoms and Health Status56 studied 2,115 |
male urethral bulb of uncertain etiology.60 |
men between 40 and 79 years of age and showed |
BPE and urethra stricture are by far the most |
that the severity of LUTS, peak flow rate, and |
common causes of BOO in men. Rare causes of |
extent of prostate enlargement were all age- |
obstruction in men include congenital urethral |
dependent and interrelated. However, the |
abnormalities,61,62 foreign bodies,63 uretero- |
Veterans Affairs Cooperative Study57 comparing |
coele,64 adult onset voiding dysfunction.65 |

214
Practical Urology: EssEntial PrinciPlEs and PracticE
Female |
|
|
|
2. |
BOO caused by stress incontinence surgery is |
|||||||
In women, several factors can contribute to BOO |
|
symptomatic of |
the conflicting roles of the |
|||||||||
|
lower urinary tract in being responsible both |
|||||||||||
(Table 16.2), which consequently represents a |
|
|||||||||||
|
for urinary storage and intermittent expulsion |
|||||||||||
more diverse |
situation |
pathophysiologically |
|
|||||||||
|
of the urine. In women with incontinence, the |
|||||||||||
than is the case in men. As discussed above, |
|
|||||||||||
|
need to improve urine storage surgically car- |
|||||||||||
this renders formal standardized diagnosis |
|
|||||||||||
|
ries an implicit risk that voiding may be |
|||||||||||
problematic. |
|
|
|
|
||||||||
1. Pelvic Organ Prolapse (POP). Deficiency of |
|
impaired.For most women,voiding function is |
||||||||||
|
satisfactorily preserved, but a minority do suf- |
|||||||||||
ligamentous support of the pelvic floor and |
|
|||||||||||
|
fer impaired voiding, taking the form of void- |
|||||||||||
weakness of the musculature results in pro- |
|
|||||||||||
|
ing symptoms, an increased post-void residual |
|||||||||||
lapse of pelvic and abdominal organs. Where |
|
|||||||||||
|
or acute urinary retention. This is recognized |
|||||||||||
the anterior vaginal compartment is affected, |
|
|||||||||||
|
for the main surgical options available, includ- |
|||||||||||
the altered configuration may distort the ure- |
|
|||||||||||
|
ing midurethral slings,74 other forms of sling75 |
|||||||||||
thra, which can impair voiding.Where middle |
|
and colposuspension,76 along with techniques |
||||||||||
compartment prolapse to the level of the vag- |
|
no longer in general use such as the Stamey |
||||||||||
inal introitus is present, a direct compression |
|
|||||||||||
|
procedure77 and bone-anchored slings.78 |
|
||||||||||
effect on the urethra could also |
occur. |
3. |
Functional causes; the lower urinary |
tract |
||||||||
Obstructive voiding, LUTS, in general, and |
||||||||||||
|
musculature and the range of CNS structures |
|||||||||||
occult stress incontinence can all coexist.72 |
|
|||||||||||
|
contributing |
to |
their regulation requires |
|||||||||
Some women with prolapse find that voiding |
|
|||||||||||
|
coordinated activity to achieve normal func- |
|||||||||||
is impeded during the daytime, as a conse- |
|
|||||||||||
|
tion. Some women manifest voiding abnor- |
|||||||||||
quence of upright posture, and complain of |
|
|||||||||||
|
malities, |
which |
appear |
to |
derive |
from |
||||||
incontinence |
overnight, when the |
supine |
|
|||||||||
|
excessive |
activity, failure |
of |
relaxation, or |
||||||||
position reduces the |
prolapse. The |
precise |
|
|||||||||
|
impaired coordination of some of these com- |
|||||||||||
effect can be hard to evaluate urodynami- |
|
|||||||||||
|
plex components. In part, this can derive |
|||||||||||
cally,73 since effects on voiding are dependent |
|
|||||||||||
|
from failure to acquire normal toileting hab- |
|||||||||||
on the patient’s position, which will affect the |
|
|||||||||||
|
its in childhood, or acquired in adulthood,65 |
|||||||||||
anatomical relationship between the abnor- |
|
leading |
to |
dysfunctional |
voiding79 |
and |
||||||
mally mobile structures and markedly influ- |
|
“pseudo-dyssynergia.” Fowler’s syndrome is |
||||||||||
ence their function. |
|
|
|
|||||||||
|
|
|
an acute onset condition arising in adult |
|||||||||
|
|
|
|
|
||||||||
|
|
|
|
|
women, characterized by painless retention, |
|||||||
Table 16.2. causes of female bladder outlet obstruction |
|
and diagnosed by high urethral closure pres- |
||||||||||
|
sures and abnormal urethral sphincter EMG |
|||||||||||
Anatomical |
|
Functional |
|
|
||||||||
|
|
|
activity 80 (Fig. 16.4). |
|
|
|
||||||
|
|
|
|
|
|
|
|
|||||
gynecological; pelvic organ |
bladder neck obstruction |
prolapse, fibroids, lichen |
|
sclerosus66 |
|
Postsurgical |
Pseudodyssynergia |
Urethral abnormalities, |
fowler’s syndrome |
such as diverticulum,67 |
|
stenosis68 |
|
Mass lesions such as |
|
uterine fibroids,69 other |
|
intra-abdominal |
|
lesions70 |
|
Ureterocoele71 |
|
Neurourology
Impaired voiding function is common in patients with neurological disease, resulting from reduced bladder contractility (Fig. 16.4), BOO, or both. In lower motor neurone neurological lesions, BOO can be a consequence of pelvic floor denervation, leading to pelvic organ prolapse and urethral distortion. For upper motor neurone neurological lesions, the problem is one of failure of the urethral sphincter to relax appropriately at the time of voiding. This can
